Hair shaft disorders, involving dysplastic abnormalities in the shaft, may be caused by genetic mutations or acquired through environmental exposures. The second part of this review presents these disorders classified according to the degree of hair fragility. It is important to take a thorough medical history and examine the hair to detect changes in texture, density, quality, and whether fragility is observed or not. Trichoscopy is a useful, noninvasive tool that can suggest a diagnosis in most cases. Specific treatments for hair shaft disorders are not available at present. We recommend general care practices to prevent hair damage; examples are avoiding excessive brushing, chemical products, hairstyles that introduce tension, and exposure to excessive heat. Some hair shaft disorders improve with puberty. Others may respond to treatments such as topical applications of minoxidil.
Las displasias pilosas constituyen alteraciones en la estructura del tallo que pueden estar provocadas por factores ambientales o por mutaciones genéticas. En esta revisión se presentan las displasias pilosas sin o con escasa fragilidad capilar. Es importante realizar una exhaustiva anamnesis y una exploración del cabello dirigida a detectar cambios en la textura, la densidad, la calidad y la presencia de fragilidad en el cabello. La tricoscopia es una herramienta útil y no invasiva, que permite hacer una aproximación diagnóstica en la mayoría de los casos. Actualmente no existe un tratamiento específico para el manejo de las displasias pilosas, se recomiendan cuidados generales para prevenir el daño del cabello como el cepillado excesivo, los productos químicos, los peinados con tensión y la exposición excesiva al calor. Algunas displasias pilosas mejoran con el inicio de la pubertad, y en otros casos, tratamientos como el minoxidil tópico pueden resultar de utilidad.
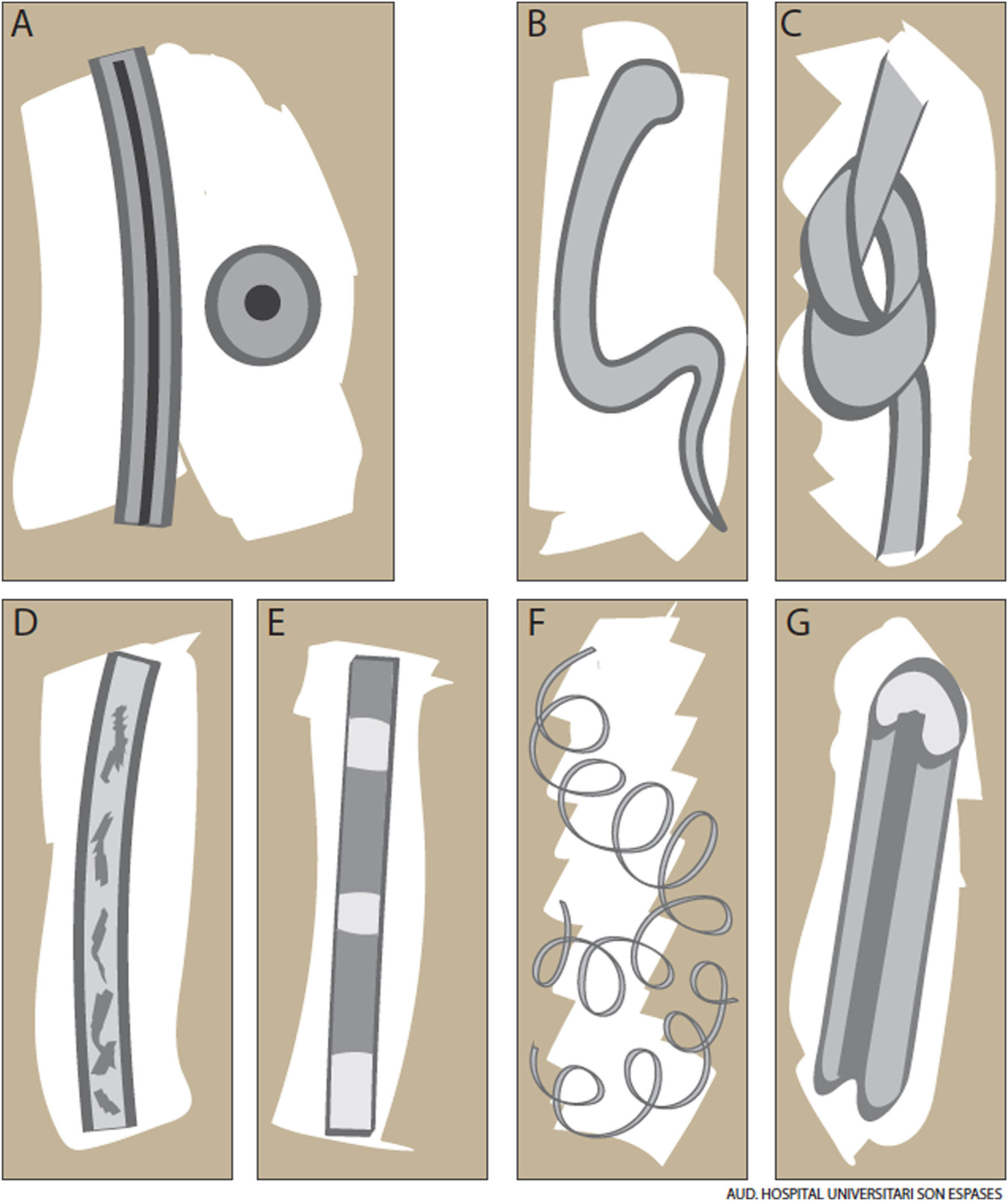
Hair shaft disorders, which are characterized by structural defects in the shaft (Fig. 1A), are caused by exposure to environmental factors or genetic mutations.1,2
Hair Shaft Disorders With Minimal or No Hair FragilityShort Anagen Hair SyndromeShort anagen hair syndrome, a congenital hair cycle disorder caused by an abnormally short anagen phase, was described by Kersey in 1987.3 It is common in clinical practice but is underdiagnosed.4,5
Short anagen hair syndrome generally affects girls aged between 2 and 4 years. Typical comments from parents are “her hair isn’t growing” or “she’s never needed a haircut”.4 Physical examination shows short hair measuring less than 6 cm. The shafts are not fragile and there are no signs of scalp inflammation. A pull test performed in 5 areas of the scalp is strongly positive, with over 5 hairs extracted per area. Performance of this test on the same day as the patient’s hair has been washed can result in a false negative. Optical microscopic examination shows telogen hairs with tapered ends (Fig. 1B), confirming that they have not been cut.5
Short anagen hair syndrome should primarily be differentiated from loose anagen hair syndrome. Although the conditions are clinically similar, the latter is characterized by defective anchoring into the scalp. Congenital hypotrichosis must also be ruled out by inquiring about family history and performing a full physical examination to rule out ectodermal dysplasia and skeletal abnormalities.
Short anagen hair syndrome usually improves during puberty and does not require treatment. Topical minoxidil 2%, however, can be attempted as it prolongs the anagen phase of the hair cycle.
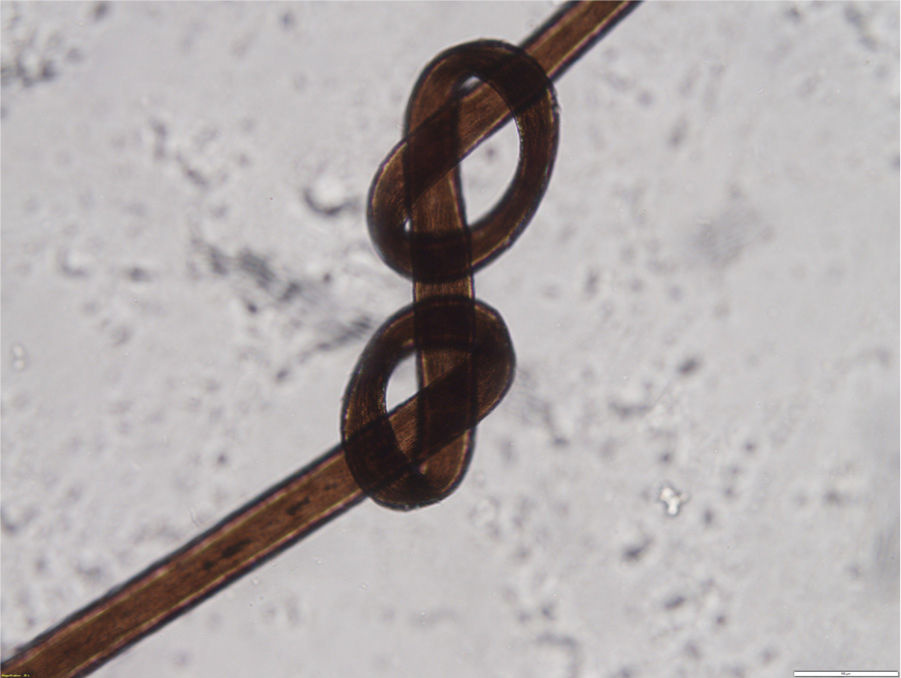
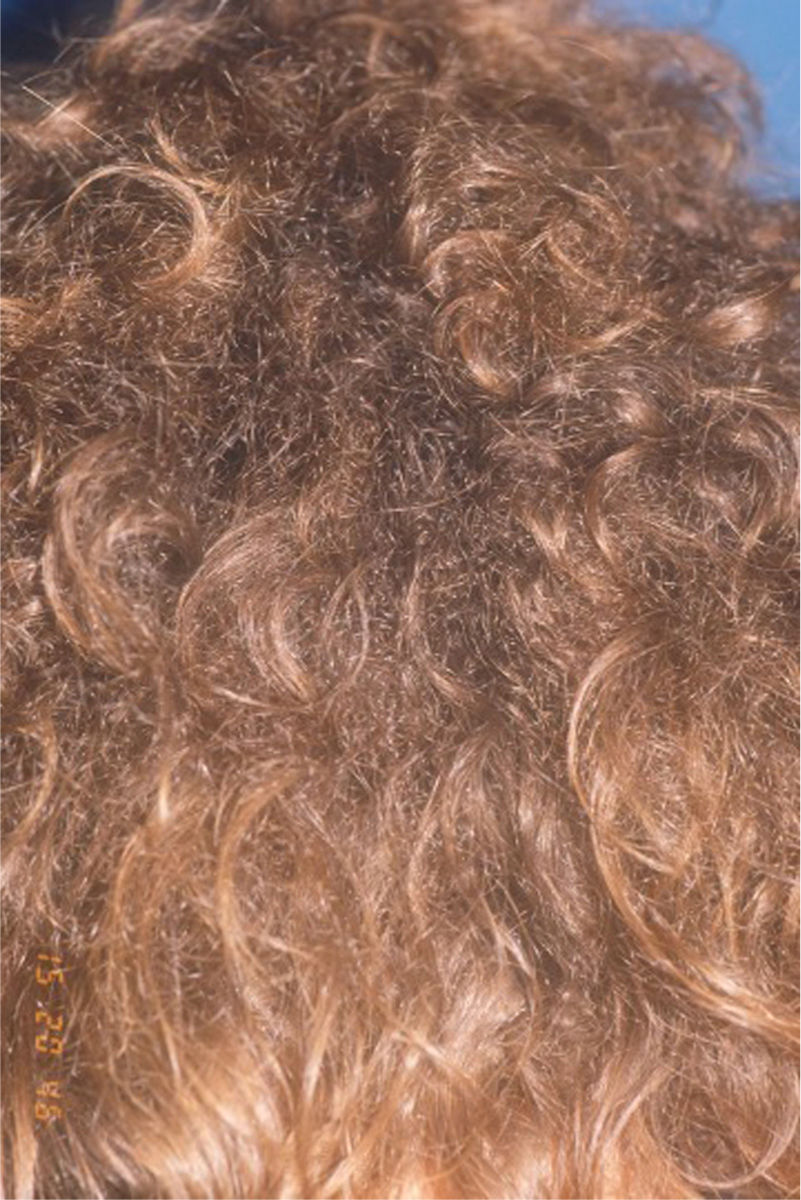
TrichonodosisTrichonodosis is a hair shaft disorder characterized by actual knots on the shaft. It was described by Galewsky and MacLeod, and while common, few reports have been published. It should be suspected whenever hair shafts showing angles or abrupt changes in direction are observed.6 Shafts may feature 1 (Fig. 1C) or 2 knots (Fig. 2), which are generally the site of breakage. Knots typically occur in curly hair and are caused by local trauma, scratching, or tics; they are normally an incidental finding.7 They can also occur in armpit or pubic hair as a result of scratching and parasites.8 Trichonodosis has no treatment, but avoidance of local trauma is recommended.
Pili Annulati (Ringed Hair or Morse Alphabet Hair)Pili annulati is a rare hair shaft condition that affects the medulla.1 It is usually present at birth or appears during early childhood.9 Although some sporadic cases exist, pili annulati is mostly inherited in an autosomal dominant fashion and has been linked to mutations in genes on chromosome 12q24.32-24.33.10,11
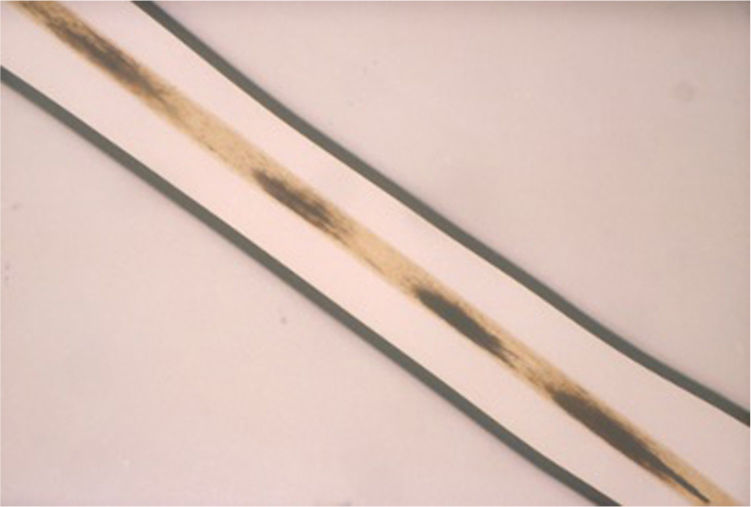
Clinically, the hair has an almost normal or shiny speckled appearance (Fig. 3), similarly to in pili torti.1 Macroscopic examination and trichoscopy show bright bands, which are seen as dark bands by optical microscopy (Fig. 4). They are due to the presence of air cavities in the medulla and a thin cortex. Although pili annulati generally affects the scalp, there may also be beard, armpit, or pubic hair involvement.12
The bright bands seen by trichoscopy in pili annulati must be differentiated from bands observed in normal hair with an intermittent medulla. In the second case they occupy less than 50% of the width of the hair shaft (Fig. 1D) whereas in the first case, they occupy between 50% and 100% (Fig. 1E).9
Pili annulati usually occurs in isolation, although associations have been reported with alopecia areata, autoimmune thyroid disease, and primary immunoglobulin deficiency A.9,11
On rare occasions, pili annulati may cause hair shaft fragility or breakages. It is an uncommon reason for consultation and prognosis is excellent. Gentle brushing is recommended to prevent breakage.11,13
Pseudopili AnnulatiPseudopili annulati is also characterized by the presence of bands, but in this case, they are the result of an optical effect caused by the reflection of light on areas of hair containing twisted, angled hair shafts. Trichoscopy will not show these bands, just hair shafts of varying diameters with curves or twists.9
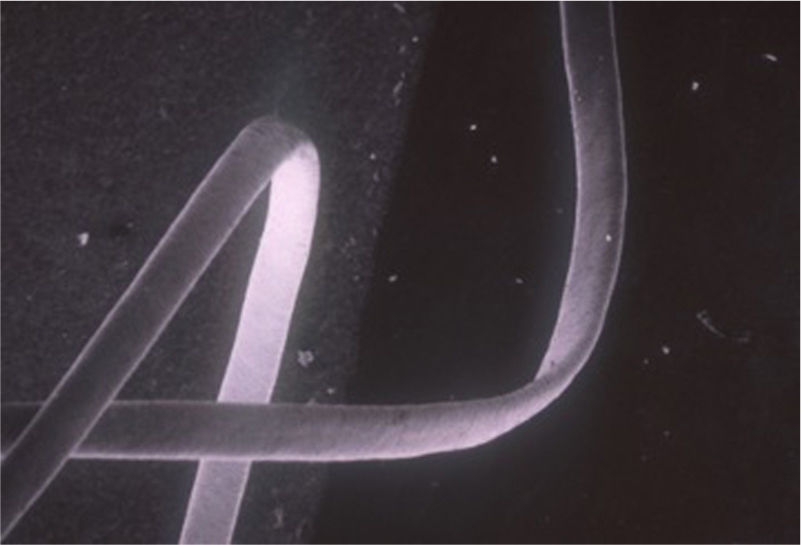
Woolly HairWoolly hair refers to coiled, fine, flat “tagliatelle-like” hair (Fig. 1F) that twists up to 180º around its axis (Fig. 5)6,9. It usually affects White individuals. There are 3 types, described below.1
Diffuse Woolly HairDiffuse woolly hair is rare. In children, it presents as very fine, soft, curly hair through which the scalp can be seen. Trichoscopy of the shaft shows a “crawling snake” appearance; breakages or areas of hypotrichosis may also be seen.7,9
Individuals with woolly hair may have keratinization disorders and eye, teeth, bone, or other abnormalities. Autosomal dominant forms due to mutations in KTR75 (12q13) and autosomal recessive forms due to mutations in P2RY5 (13q14.2-q14.3), LIPH (3q27-q28), and LAH2 (3q27-q28) have been described. Syndromes involving woolly hair include Naxos syndrome, which is caused by mutations in the plakoglobin gene and consists of woolly hair, palmoplantar keratoderma, and cardiomyopathy.6 Other syndromes include Carvajal-Huerta syndrome, Noonan syndrome, hair hypotrichosis with woolly hair, ectodermal dysplasia/skin fragility syndrome, and trichohepatoenteric syndrome. There have been 4 recent reports of patients with neurological abnormalities and woolly hair.11,14
There are no definitive treatments for woolly hair, but the condition can improve over the years. Nonablative fractional laser therapy in a series of 3 adults produced favorable results.15
Woolly Hair NevusWoolly hair nevus is characterized by single or multiple well-circumscribed patches of woolly hair (Fig. 6) that may be present at birth or appear during the first 2 years of life.9,16 Histology shows clusters of miniaturized anagen hairs.6,17 Up to 50% of patients have an epidermal or melanocytic nevus in the same area or in another part of the head. This nevus can appear in isolation or be accompanied by eye or teeth abnormalities, delayed speech development, or congenital triangular alopecia.6
Diffuse Partial Woolly HairDiffuse partial woolly hair is characterized by the same hair shaft alterations as those seen in woolly hair, but they affect individual shafts surrounded by 10–12 normal-appearing hairs1,18. It usually affects children and adolescents, and can be sporadic or familial. Autosomal dominant forms might be related to mutations in the KRT74 gene (12q.13).1 No external triggers have been identified.1,18,19
Trichoscopy shows similar findings to those seen in woolly hair, although the hair shafts are not so tightly coiled. Electron microscopy shows longitudinal grooves and a curved, flat, oval cross-section.20,21
Acquired Progressive Kinking of the HairAcquired progressive kinking of the hair is more common in young men. Unlike partial diffuse woolly hair, it tends to occur in specific areas, and is particularly common in the frontotemporal region (Fig. 7).1 Patients progressively develop short, kinked hair, similar to beard hair; they may also have trichiasis.22,23 Trichoscopic findings are similar to those seen in woolly hair.1 Although acquired progressive kinking of the hair is more common in men, 2 cases have been reported in postmenopausal women.24 Onset might be related to oral retinoid use.6 No genetic causes have been identified.
Acquired progressive kinking of the hair can progress to androgenetic alopecia and is therefore treated with topical minoxidil and oral finasteride.25
Acquired Partial Kinking of the HairAcquired partial kinking of the hair affects the distal end of isolated hair shafts; the proximal end is unaffected. It is more common in young women, and could be linked to the use of cosmetic treatments.
Trichoscopy shows a normal-appearing proximal end, with mild distal kinking and thinning.
Acquired partial kinking of the hair usually improves with time, use of hair conditioners, and avoidance of external aggressions.1
Straight Hair NevusContrarily to woolly hair nevus, straight hair nevus is characterized by a well-defined area of straight hair surrounded by curly hair, although it has also been described in patients with straight hair.26,27 The few cases that have been published have occurred in association with keratinization disorders, such as ichthyosis and epidermal nevi.6,28
Trichoscopy shows straight hairs. Electron microscopy shows irregularities in the number and size of cuticle cells, which are arranged in a disorganized fashion. Other findings are increased porosity on cross-section and several longitudinal grooves.27,29,30 Histology shows increased sebaceous glands in the affected area.6
Although mutations have not been identified, it has been proposed that straight hair nevus might be due to mosaicism or constitute a hair shaft disorder caused by alterations in the underlying skin, rather than an entity in its own right,6,27 as it has always been observed in association with a keratinization disorder or local sebaceous hyperplasia (eg, nevoid sebaceous hyperplasia).
Uncombable Hair Syndrome (Pili Canaliculi et Trianguli)Uncombable hair syndrome, also known as pili canaliculi et trianguli, is characterized by fair, dry, lusterless hair that grows in multiple directions, making it impossible to style (Fig. 8).31 Hair growth can be normal or slow and hair shafts are not normally fragile. Uncombable hair syndrome develops in childhood, typically between the ages of 3 months and 3 years, and shows no predilection for sex. It may be an isolated phenomenon, although there have been reports of associations with ectodermal dysplasias, retinal dysplasias, juvenile cataracts, polydactyly, and tooth alterations.31
Uncombable hair syndrome can be sporadic or familial; autosomal and recessive forms have been described.1 In recent years, mutations have been identified in 3 genes that code for key structural proteins involved in hair formation: PADI3 (peptidyl arginine deaminase 3), TGM3 (transglutaminase 3), and TCHH (trichohyalin).32
Dermoscopy is useful, but the diagnostic method of choice is electron microscopy, which shows longitudinal depressions or grooving and irregular, triangular, and kidney-shaped forms on cross-section (Fig. 1G).31,33
Because electron microscopy is costly and is available at all centers, alternative diagnostic tools have been proposed, including hair cross-sectioning with hematoxylin-eosin staining, which shows typical triangular shapes,34 and more recently, frozen-section examination (similar to that used in Mohs micrographic surgery)35 and epoxy resin embedding.36
Uncombable hair syndrome tends to improve with the onset of puberty. Biotin supplementation has produced favorable results in some patients.37 Zinc pyrithione shampoo might also be useful as it causes a rebound effect, increasing the production of oil on the scalp and providing a certain conditioning effect that improves the dry appearance of the hair.1
DiscussionHair disorders are a common reason for consultation in dermatology and a cause of anguish among patients and/or parents. It is important to take a thorough history and examine the hair to check for signs of fragility and changes in texture, density, and quality. Trichoscopy is a useful, noninvasive tool that suggests a diagnosis in most cases. It is particularly useful for evaluating children, as it does not require the removal of hair.17
Hair shaft disorders may sometimes be part of a more complex syndrome, so multidisciplinary evaluation may be necessary.1 Genetic counseling is recommended for patients with hereditary or congenital hair shaft disorders.12
Specific treatments are not currently available for the management of hair shaft disorders. Some conditions, such as pili torti, trichorrhexis invaginata, woolly hair, and pili canaliculi, improve with the onset of puberty. Others, such as trichorrhexis nodosa, monilethrix, and pili annulati, may improve with the use of minoxidil. Oral retinoids are a useful alternative for certain cases of trichorrhexis invaginata or monilethrix.12
General hair care is recommended for patients with hair shaft disorders, who should be advised to use tension-free hairstyles and avoid external aggressions, such as excessive brushing, chemical products, and exposure to excessive heat.12
FundingNo funding was received for this study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Dr. Martín-Santiago for her comments during the preparation of this manuscript and for the clinical images provided, Dr. Saus for his dedication and microscopic images, and Marina Cascales for kindly preparing the graphic representations.
Please cite this article as: Giacaman A, Ferrando J. Claves diagnósticas en displasias pilosas II. Actas Dermosifiliogr. 2022;113:150–156.