A 7-year-old boy diagnosed with B-cell acute lymphoblastic leukemia on chemotherapy and broad-spectrum antibiotics presented with a 2-week history of fever and a painful localized nodule on his right thigh.
Physical examination revealed a 2cm solitary painful, well-demarcated, violaceous nodule on the patient's right thigh. The lab test results revealed an absolute neutrophil count of 0, platelet count of 44,000/μL, and C-reactive protein of 200mg/dL (reference range, 0.1–0.5mg/dL).
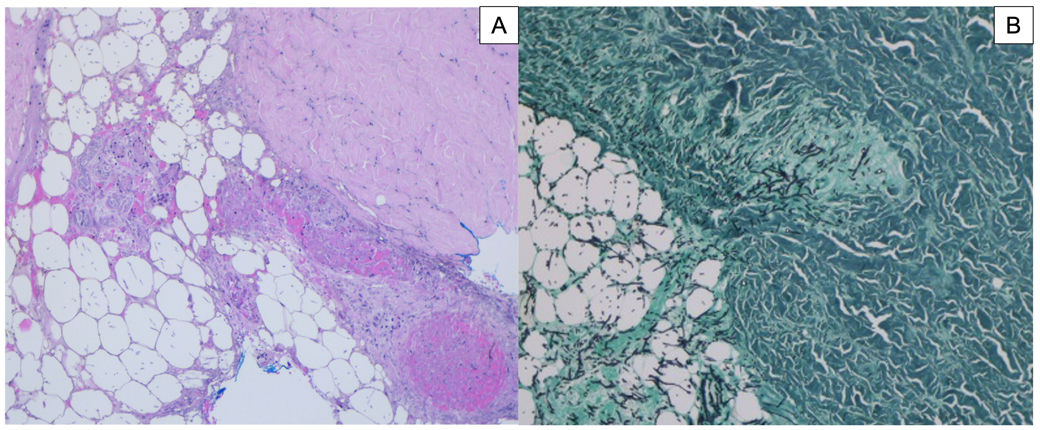
Histopathological examination of the nodule revealed the presence of epithelioid non-necrotizing granulomas on the hypodermis and septate hyphae, some with dichotomous acute angle branching on the reticular dermis and hypodermis (Fig. 1).
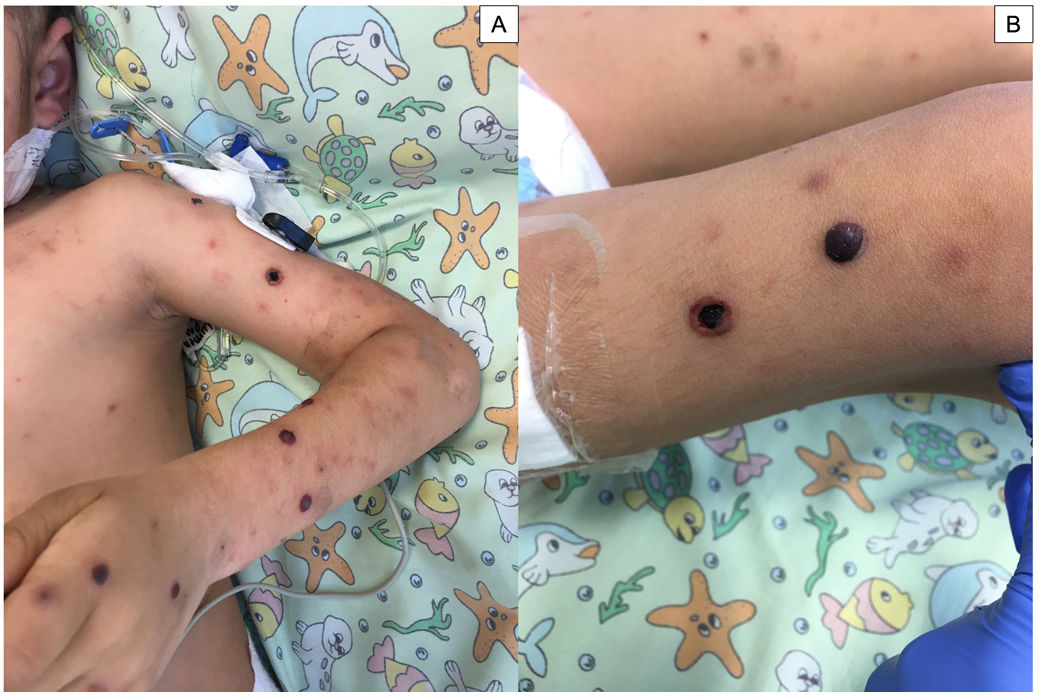
Assessments looking for systemic involvement were performed through thoracic and sinus CT scans, brain MRI, dilated-pupil fundus examination, and abdominal ultrasound, all of which were initially within normal limits. Combined therapy with voriconazole and liposomal amphotericin was initiated. Five days into treatment, the patient developed high fever, dyspnea, and dissemination of cutaneous lesions that rapidly progressed toward central necrosis, with the formation of hemorrhagic bullae and new subcutaneous nodules in the lower extremities (Fig. 2). The studies conducted to assess systemic involvement showed bilateral diffuse ground-glass pulmonary opacities and nasal septum perforation.
What is the diagnosis?
Diagnosis and commentsThe patient was diagnosed with nasal septum destruction due to an invasive fungal infection. Fusarium Solani was isolated in culture. Antifungal drug doses were up-titrated, followed by surgical debridement of the infected nasal tissues. Treatment with granulocyte colony-stimulating factor and IV immunoglobulin was indicated. The patient improved, with lesion and fever resolution. Antifungal treatment was discontinued after 19 weeks.
Fusarium spp. is an angioinvasive opportunistic fungus that may cause superficial, locally invasive, and disseminated infection. Immunocompromised patients, particularly those with prolonged and profound neutropenia, or severe T-cell immunodeficiency, are at particular risk for invasive and disseminated disease. Among patients with hematologic malignancies, the infection typically develops after receiving cytotoxic therapy.1
Although Aspergillosis and Mucormycosis are the most widely described invasive mold infections, cases of disseminated infections by Fusarium spp. are on the rise.2 In a recent review of disseminated fusariosis in pediatric patients with hematologic malignancies, the mortality rate reported was >50%.3
In immunocompromised patients, the most frequent clinical presentation is disseminated and invasive fusariosis, which most commonly affects the sinus, lungs, and skin.4,5 Disseminated disease typically presents with erythematous–violaceous papules and nodules that progress toward central necrosis within a few days.6
Fusarial sinusitis occurs in 18% of pediatric and adult cases, more commonly among patients with acute leukemia and prolonged and profound neutropenia. The infection may progress into mucosal necrosis due to the angioinvasive nature of Fusarium spp.5 Sinus involvement has been reported in 5 prior pediatric cases, with only 1 presenting with nasal septum destruction.
Pathogen isolation through culture is required for diagnostic purposes. Blood cultures are positive in 40% of invasive cases5; however, a faster diagnosis may be achieved by examining skin tissue by imprint cytology and conventional histopathology when clinical suspicion is high. The finding of hyaline septate filaments that typically dichotomize in acute angles and reniform adventitious conidia is highly suggestive of fusariosis. The distinction between Aspergillus spp. and Fusarium spp. is only conclusive through culture identification.6
The limited data on fusariosis treatment in children, and the relative resistance of Fusarium spp. to most antifungal compounds, hinder an appropriate treatment. A multifaceted approach is advised in these cases, including systemic antifungal drugs, surgical debridement of infected tissues, and measures to enhance immunity. Considering the high mortality rates of immunocompromised children, some authors recommend using a combination of antifungal drugs.4
FundingThis work has not received any funding.
Conflict of interestsThe authors declare that they have no conflict of interest.