Intussusception is the infolding of one portion of the bowel within another and is the most common cause of intestinal obstruction in early childhood. Adult intussusception accounts for fewer than 5% of all intussusceptions and only 1% of all bowel obstructions.1 The symptoms are those of partial or complete mechanical bowel obstruction, and in partial cases, the course can be intermittent or chronic.2
Cutaneous melanoma is rarely diagnosed as the etiology of intussusception in adults and is therefore not usually suspected when obstructive symptoms appear.
We describe a 47-year-old woman diagnosed with superficial spreading cutaneous melanoma on the left shoulder. The lesion showed no ulceration and had a diameter of 8mm, a Breslow depth of 4mm, and a Clark level of III. Following surgical resection and the detection of positive sentinel lymph nodes, axillary lymphadenectomy was performed; histology was negative. The patient received adjuvant therapy with interferon, but experienced recurrence in the left supraclavicular lymph nodes 2 years later. After 3 doses of fotemustine, the left supraclavicular lymph nodes were resected en bloc; 3 of these nodes were positive. The patient received radiation therapy to the surgical site.
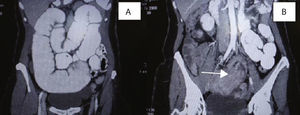
Some months later, the patient was urgently referred to the general surgery department for colicky abdominal pain, digestive intolerance, loose stools, and macrocytic anemia. Computed tomography (CT) revealed bowel obstruction (Fig. 1), and probable intestinal metastasis of the cutaneous melanoma was suspected.
During surgery, intussusception was observed and the head was found to consist of a bluish mass; the intussuscepted jejunum (Fig. 2) and all visible blue lymph nodes were resected en bloc.
Macroscopically, the small bowel specimen was 39cm in length, with intussusception at 14.5cm caused by a blackish tumor of 4×7cm that occluded the entire lumen. The microscopic report described melanoma infiltrating the muscularis propria; 5 of the 17 lymph nodes isolated in the mesocolon were positive. The resection borders were free of tumor.
The postoperative course was unremarkable, and the patient was referred to the oncology department for follow-up.
Intussusception in an adult is a potentially serious condition that is usually secondary to an intestinal wall lesion: benign or malignant tumor, inflammatory lesion (appendicitis, Meckel diverticulum), or even a foreign body in the small bowel. Therefore, it almost always occurs in the ileocecal area, but is less common in the jejunojejunal or ileocecocolic areas.
The preoperative diagnostic techniques of choice are CT and ultrasound. Recent studies recommend that patients with cutaneous melanoma who develop gastrointestinal symptoms should undergo contrast-enhanced studies (enteroclysis, opaque enema, etc.), complemented by CT, depending on the result.3
The definitive diagnosis is established after surgery and histology. In general, immunohistochemical staining of the material obtained is essential for the diagnosis of metastatic tumors.4
Bowel resection is the surgical technique of choice because of its increased safety and adherence to oncologic principles. The intussusception should only be reduced first when there is a potential benefit to the patient.2
Other groups advocate conservative treatment when the etiology of intussusception is not clear; such treatment will depend on the type of intussusception and on the clinical signs and symptoms and should always be accompanied by follow-up.5
Intussusception can now be diagnosed and treated laparoscopically, although in cases of complete bowel obstruction, the technique is complicated by the distension of the intestinal loops and the fragility of the intestinal wall.
The head of the intussusception is often a malignant lesion (52% of cases),6 and there are cases where this lesion is a metastasis of a cutaneous melanoma.7
The presence of an early complication caused by bowel obstruction, investigated by appropriate diagnostic methods, can lead to the early diagnosis of metastatic spread of a melanoma,8 as in the case we describe.
Once metastasis is diagnosed, surgery is the only option for treating complications of bowel obstruction due to melanoma (e.g. chronic anemia, episodes of partial bowel obstruction) and improving survival rates and quality of life in these patients.9
Please cite this article as: Muiños-Ruano L, et al. Invaginación intestinal en el adulto secundaria a metástasis de melanomsa cutáneo. Actas Dermosifiliogr.2012:441-2.