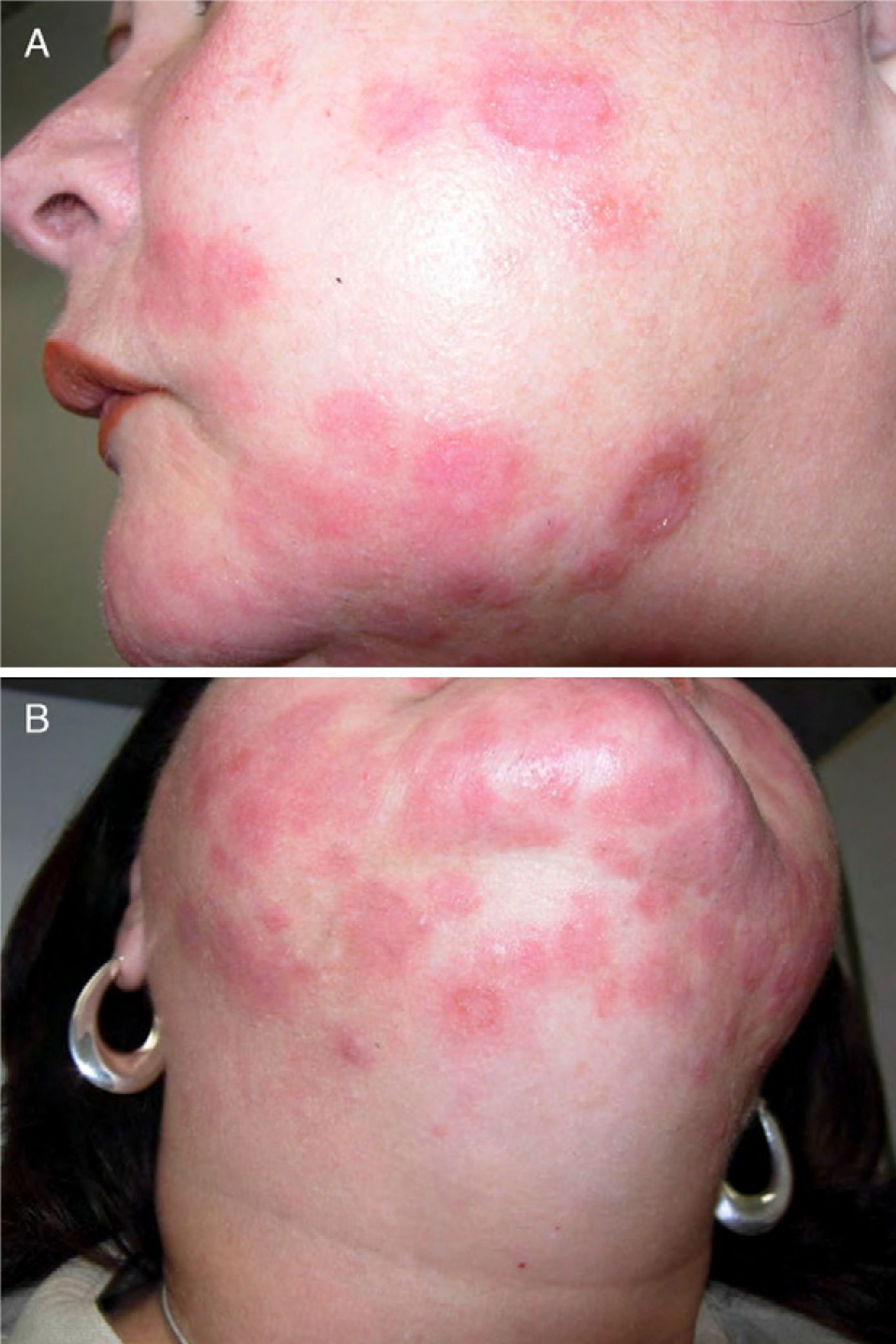
A 53-year-old female with a 2-month history of a painful pruritic eruption on the face. The patient had previously presented with abrupt onset of multiple edematous pseudovesicular papules on the face and shoulders preceded by a febrile upper respiratory infection (Fig. 1A and B). A diagnosis of Sweet's syndrome had been presumed pending pathologic confirmation. Initially, the condition was treated empirically with triamcinolone 0.1% cream twice daily and prednisone starting with 60mg daily and gradual tapering. No improvement was observed and new lesions developed. Therefore, and after receipt of the pathology report (see below), hydroxychloroquine 200mg twice daily was added to the corticosteroid regimen with suspicion of either Jessner lymphocytic infiltrate, lupus tumidus, or polymorphic light eruption. No response was observed after one-month of treatment.
Physical examinationPhysical examination revealed multiple well-defined edematous pseudovesicular papules and plaques symmetrically distributed on the chin and both cheeks with underlying erythema and a few scattered lesions on the shoulders.
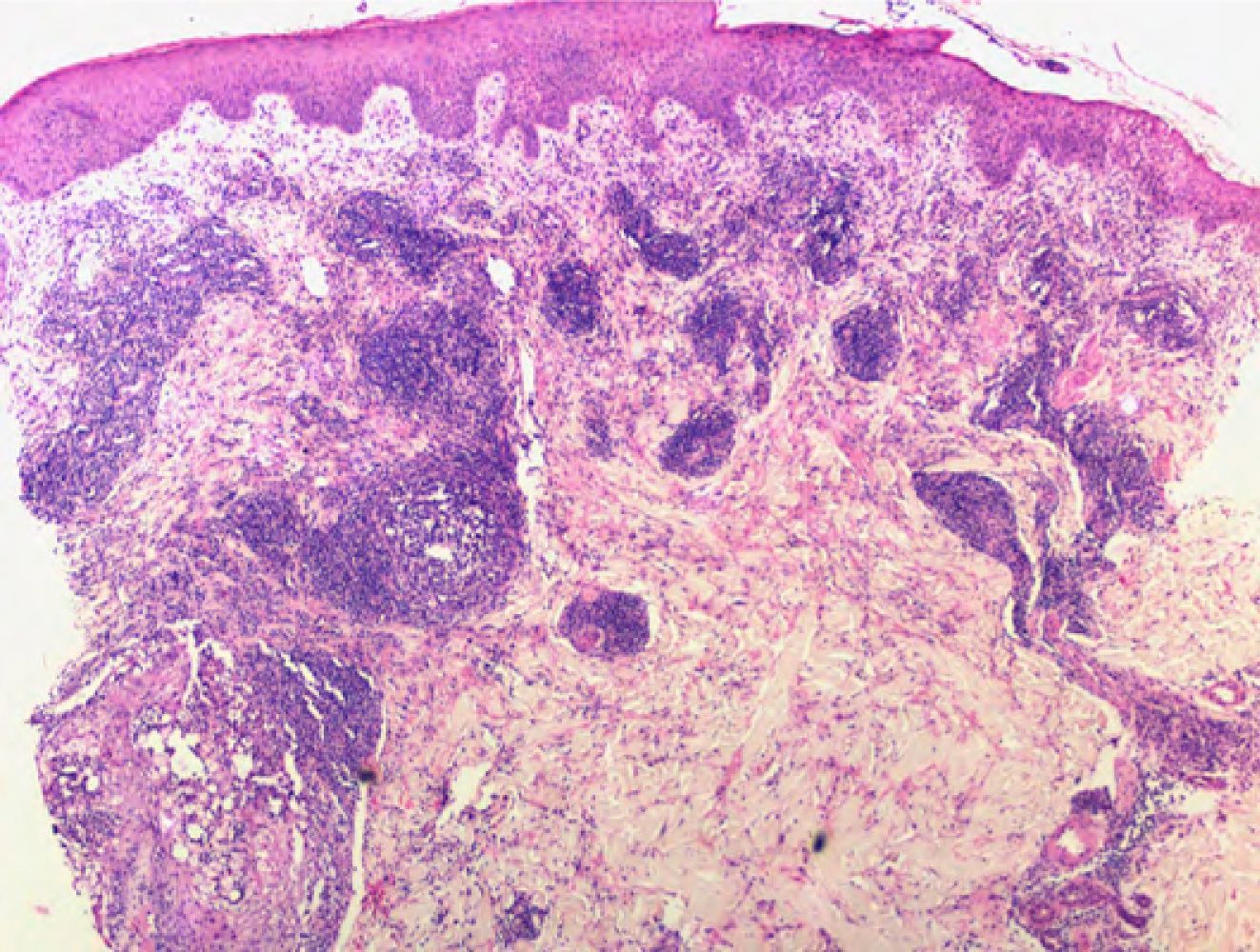
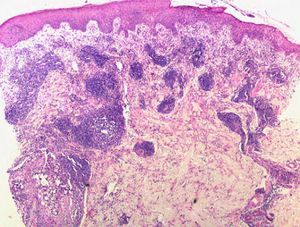
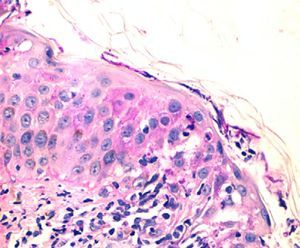
Microscopic examinationMicroscopic examination revealed perivascular and periadnexal lymphocytic infiltrate with papillary edema. A biopsy from lesional skin was submitted for direct-immunofluorescence with negative results. Examination of a biopsy obtained 1 month later revealed the above-mentioned changes, together with a mixed inflammatory infiltrate containing neutrophils in the hair follicle (Fig. 2).
What is Your Diagnosis?
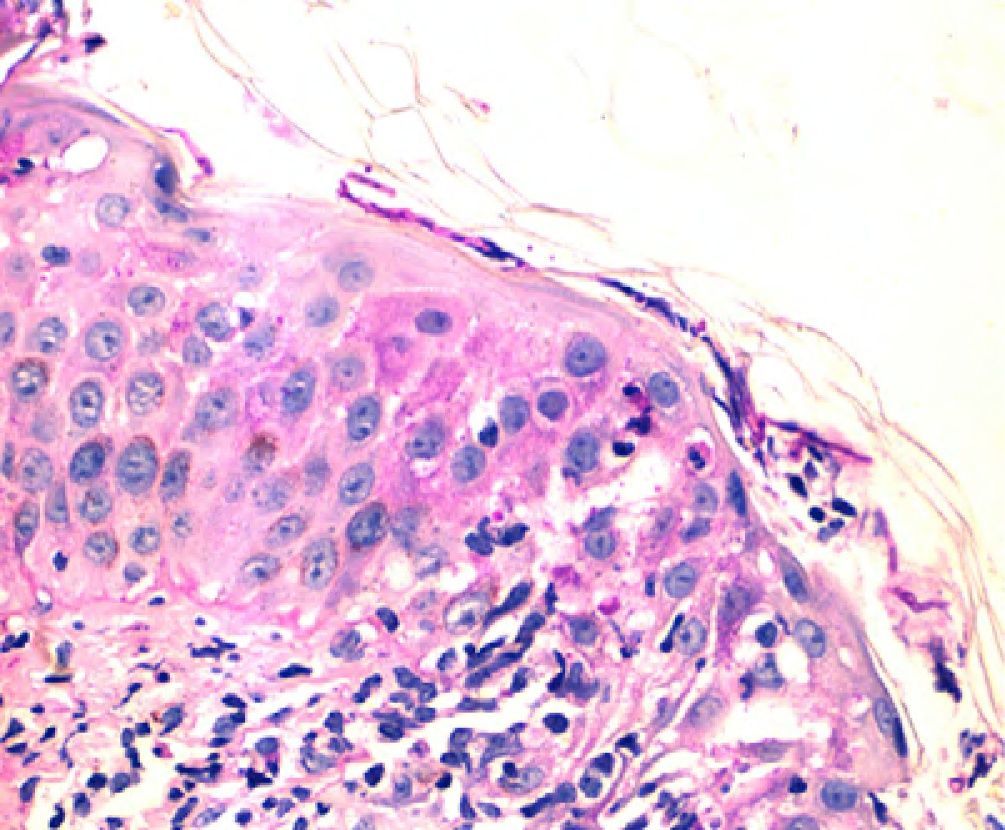
DiagnosisThe diagnosis was inflammatory tinea faciei caused by Microsporum canis. Periodic acid–Schiff staining revealed the presence of a small number of hyphae in the stratum corneum and hair follicles (Fig. 3). Culture identified these as M. canis.
TreatmentTreatment with griseofulvin 500mg/d resulted in complete resolution of the lesions within 1 month.
CommentTinea faciei is a superficial dermatophyte infection localized to the glabrous skin of the face. M. canis is an organism that causes dermatophytosis (ringworm) mostly in dogs and cats. In humans, it is an infrequent zoonosis, usually associated with severe inflammatory reactions. Our patient was cohabiting with a dog at the time of presentation. Falahati et al. isolated M. canis in 6.5% of patients with dermatophyte infections in a study in Iran.1 In the USA, Trichophyton tonsurans is the predominant dermatophyte isolated and only a few cases of tinea faciei caused by M. canis have been reported in American schools.2 The prevalence differs depending on the geographic area. In Italy, M. canis is the main causal organism in children with dermatophyte infections of the face. In Mexico, it was isolated in 38.2% of patients with tinea capitis, but only a few cases of tinea faciei caused by this organism have been reported.3,4 The clinical presentation of tinea faciei can closely resemble that of other dermatoses, leading to misdiagnoses and delayed treatments as occurred in the present case.5 It can mimic atopic dermatitis, impetigo, lupus erythematosus, and periorificial dermatitis. Steroid-modified tinea (tinea incognito) may be observed when the condition has been misdiagnosed and the lesions have been erroneously treated with topical corticosteroids. Our patient initially presented with abrupt onset of a facial skin eruption. The acute onset of the lesions and their association with a febrile respiratory infection was clinically suggestive of Sweet's syndrome. Several authors have reported cases of inflammatory tinea masquerading as reactive dermatoses. For instance, tinea barbae caused by Trichophyton mentagrophytes can mimic contact dermatitis or acneiform dermatitis. Inflammatory tinea capitis has been reported to induce lupus erythematous-like eruptions.6 Shanon et al. reported 3 patients with tinea faciei simulating discoid lupus erythematosus.7 Dermatophytosis usually follows a chronic non-inflammatory clinical course and is mostly limited to the superficial keratin structures. Subcutaneous involvement is rare and involves atypical clinical manifestations such as pustular psoriasiform trichophytia, trichophytosis mimicking pseudolymphoma or Sweet's syndrome, and impetiginized herpetiform trichophytosis in which a definitive diagnosis is generally confirmed by biopsy. Exceptional cases have been reported of tinea corporis bullosa caused by M. canis in which the clinical presentation was characterized by multiple annular bullous lesions.
In the present case, the clinical picture resembled Sweet's syndrome, but subsequent treatment with oral and topical corticosteroids only worsened the condition. Despite repeated biopsies, diagnosis was challenging, and only appropriate histopathological examination with special stains and tissue cultures allowed the diagnosis to be confirmed, isolating M. canis as the pathogenic organism. The lesions resolved completely after 1 month of treatment with griseofulvin.
This case illustrates the need to consider an infectious etiology in what would otherwise be presumed to be cases of reactive dermatosis refractory to corticosteroid therapy.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Viera MH, et al. Inflammatory tinea faciei mimicking Sweet's syndrome. Actas Dermosifiliogr. 2013;104:75-6.