Infantile hemangioma (IH) is the most common benign tumor of infancy, affecting 1% up to 10% of children younger than 1 year.1–3 IHs can occur anywhere on the body but are most frequently found on the head and neck.1 Approximately 1% of cases develop in the genital area.4
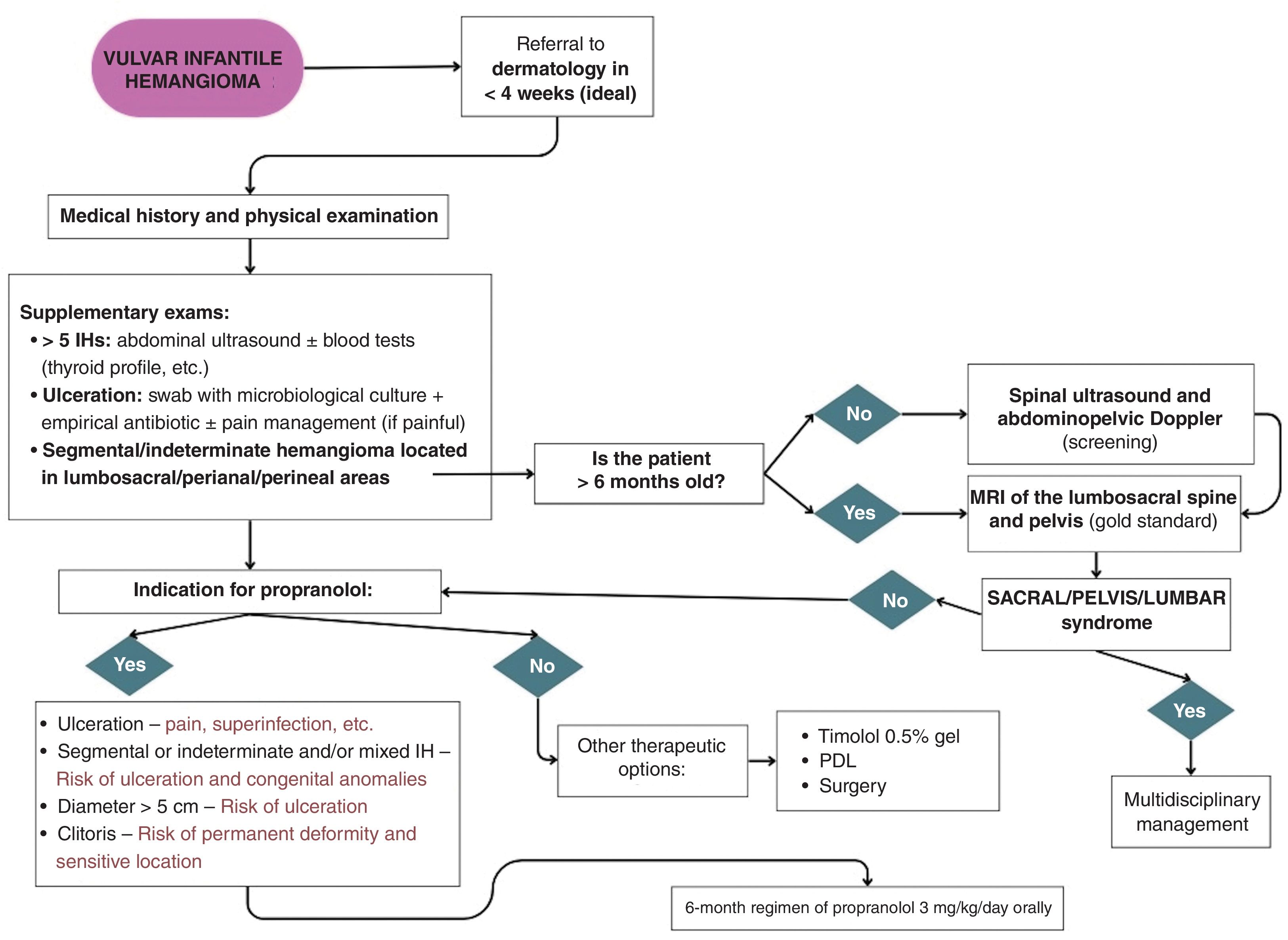
When managing vulvar IHs, several factors should be considered, including their natural history, location, involvement of functionally significant structures, ulceration, symptoms, and the potential for long-term sequelae.1–3 Most IHs are small and tend to regress spontaneously, allowing for an expectant management approach.1–3 However, 5% up 10% require early active therapy to prevent anatomical distortion.2,3,5,6
The objective of this study is to describe the clinical and evolutionary characteristics and treatment of vulvar IHs, proposing a diagnostic-therapeutic algorithm. We conducted a retrospective review of vulvar IHs seen at a tertiary referral center dermatology department from 2016 to 2023, including cases with clinical images and a 6-month minimum follow-up.
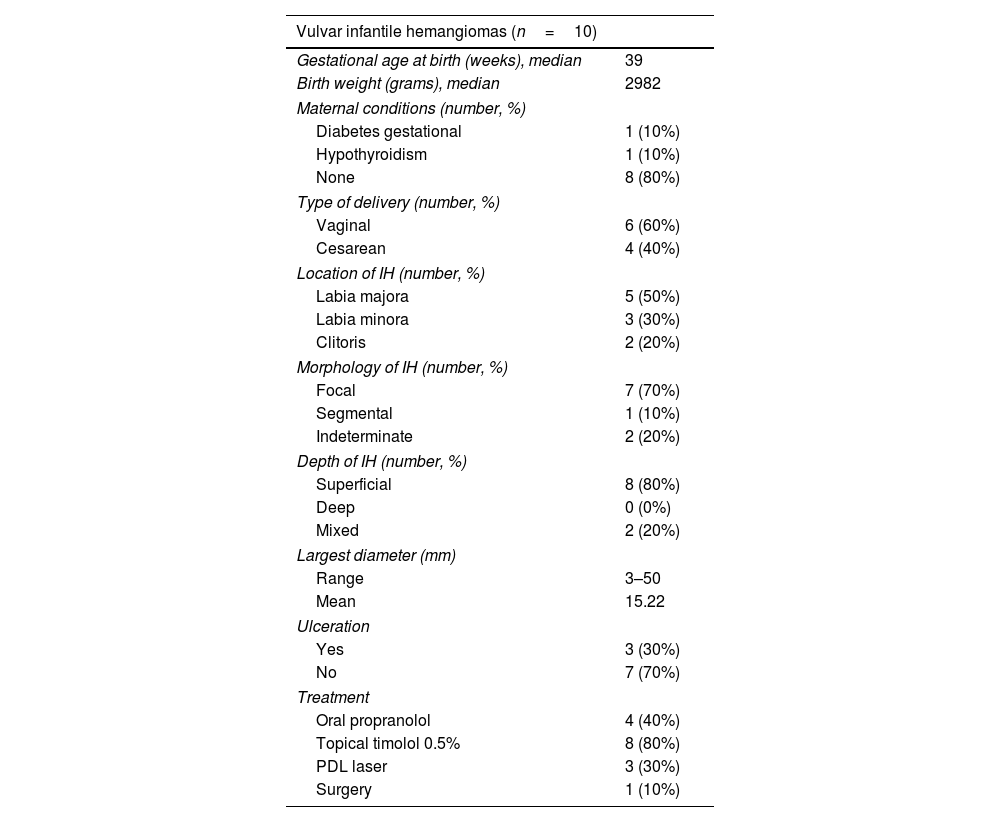
A total of 10 patients were included, whose clinical characteristics are shown in table 1. All had appropriate birth weights for their gestational age, with a median weight of 2982g (range, 2600–4000g). A total of 90% were born at term, with a median gestational age of 39 weeks, except for 1 preterm birth on week 36. Pregnancies were uneventful, except for 1 uncontrolled pregnancy requiring C-section delivery due to the risk of neonatal infection by Streptococcus agalactiae.
Characteristics of the patients, hemangiomas, and treatment received.
| Vulvar infantile hemangiomas (n=10) | |
|---|---|
| Gestational age at birth (weeks), median | 39 |
| Birth weight (grams), median | 2982 |
| Maternal conditions (number, %) | |
| Diabetes gestational | 1 (10%) |
| Hypothyroidism | 1 (10%) |
| None | 8 (80%) |
| Type of delivery (number, %) | |
| Vaginal | 6 (60%) |
| Cesarean | 4 (40%) |
| Location of IH (number, %) | |
| Labia majora | 5 (50%) |
| Labia minora | 3 (30%) |
| Clitoris | 2 (20%) |
| Morphology of IH (number, %) | |
| Focal | 7 (70%) |
| Segmental | 1 (10%) |
| Indeterminate | 2 (20%) |
| Depth of IH (number, %) | |
| Superficial | 8 (80%) |
| Deep | 0 (0%) |
| Mixed | 2 (20%) |
| Largest diameter (mm) | |
| Range | 3–50 |
| Mean | 15.22 |
| Ulceration | |
| Yes | 3 (30%) |
| No | 7 (70%) |
| Treatment | |
| Oral propranolol | 4 (40%) |
| Topical timolol 0.5% | 8 (80%) |
| PDL laser | 3 (30%) |
| Surgery | 1 (10%) |
All IHs were found on external genitalia (5 on the labia majora, 3 on the labia minora, and 2 on the clitoris), with a median diameter of 8mm (range, 3–50mm). A precursor lesion was noted at birth in 50% of the cases. Most IHs were focal (70%), with a smaller proportion being indeterminate (20%) or segmental (10%) (Fig. 1). A total of 8 lesions were superficial, and 2 were mixed. In 1 segmental IH, magnetic resonance imaging (MRI) of the lumbosacral spine and pelvis ruled out the presence of any associated malformations. The IH of 1 of the patients occurred in the context of benign neonatal hemangiomatosis, with 4 additional lesions on the left leg, trunk (2), and face. Visceral IHs were ruled out via abdominal ultrasound. Three cases (30%) developed ulceration at the follow-up.
Clinical images of vulvar IHs. Mixed ulcerated IH in a 2-month-old girl (A). Three months into propranolol 3mg/kg/day (B) and at the end of treatment (9 months) (C). Segmental vulvar and perianal IH in a 7-month-old girl (D). Five months into propranolol 3mg/kg/day (E) and at the end of treatment (7 months) (F). Superficial focal IH in the clitoris of a 6-month-old girl (G). At 12 months of age, on timolol 0.5% gel and PDL (H). One month into propranolol with decreased volume and erythematous component (I) – lost to follow-up.
All patients received treatment, either monotherapy (n=7) or combination therapy (n=3), including oral propranolol (n=4), topical timolol (n=8), pulsed dye laser (PDL) (n=3), and excision with electrocautery for one pedunculated IH. Patients treated with oral propranolol started at a median age of 5 months and were dosed at 3mg/kg/day for a median duration of 7 months. At the follow-up, 50% achieved complete resolution, 20% showed partial regression, and 30% had stable lesions, with a median follow-up of 12 months.
Anogenital IHs are considered high risk due to their greater tendency to ulcerate and associate with various congenital anomalies.5
The most common complication is ulceration, which can affect 53% of cases vs 11.54% globally for IHs.5 Predictors of ulceration include segmental or indeterminate morphology, mixed IHs, location on buttocks or perianal area, and ≥5cm diameters.5,7 In these cases, early treatment with oral propranolol should be considered, before the 5th month of life, with a therapeutic dose of 3mg/kg/day for, at least, 6 months.1–3
Perineal or lumbosacral IHs, especially if large and segmental, may be associated with congenital anomalies (pelvic or sacral or lumbar syndrome).1,2 In these cases, an MRI of the lumbosacral spine and pelvis is recommended to rule them out. In children under 6 months, lumbar canal and abdominal-pelvic ultrasound can be considered as oart of the initial screening.2 In the largest series of anogenital IHs, congenital anomalies were found in 6.4% of cases, with the most common ones being urogenital anomalies and myelopathy.5 These associations were more common in penile, sacral, and perianal IHs vs vulvar IHs.5
The location of the clitoris is especially sensitive due to its functionality and the risk of permanent deformity. In our series, it affected 20% of patients, representing a significant therapeutic challenge. Initially, they were treated with timolol and PDL with little response, so in 1 case, propranolol was initiated. It is recommended to consider propranolol treatment at this location from the beginning.
Alternatively, topical timolol 0.5% gel applied twice daily could be used for fine and superficial non-ulcerated IHs, with an adequate safety and efficacy profile.8 PDL is also useful for improving the texture of residual lesions and treating telangiectasias.9
The above-mentioned description is illustrated in Fig. 2 where we propose the management algorithm for vulvar His.
In conclusion, vulvar IHs, although rare, can present a high complication rate. They should be considered high risk and referred to a specialist early. Ulcerated, segmental, mixed IHs, those with diameters≥5cm, and those located in the clitoris require treatment with propranolol to minimize complications.
Informed consentAll patients provided informed consent for the publication of their case details.
Conflicts of interestNone declared.