Skin cancer is a common cause for referral to dermatology, but it may also be an incidental finding during examination of patients referred for other reasons. The objective of the study was to compare the characteristics of skin cancer lesions (squamous skin carcinoma, basal cell carcinoma, melanoma) diagnosed at a dermatology department over 1 year between patients referred for suspected skin cancer and those referred for another reason but in whom skin cancer was detected as an incidental finding. Pearson’s χ2 test was used to compare different study variables between the 2 groups.
ResultsData were collected from 433 patients with a mean age of 72 years; 233 (51.3%) of the patients were female. The most common skin types were Fitzpatrick types II and III. Basal cell carcinoma was the most frequent cancer in all the analyses and accounted for 68.4% of all cancers diagnosed (296/433). Twenty-six percent of the malignant skin tumors were detected incidentally. Statistical analysis revealed that these tumors tended to be located in nonvisible areas and were smaller and of more recent onset than tumors initially suspected to be malignant.
ConclusionsThe high rate of skin cancer diagnosed incidentally by dermatologists highlights the need to carry out thorough examinations of patients in order to facilitate early detection and treatment.
El cáncer de piel es un motivo frecuente de derivación a dermatología, pero también puede ser un hallazgo incidental durante la exploración por otro motivo de consulta. El objetivo del estudio fue comparar las características de las lesiones diagnosticadas de un cáncer cutáneo de forma incidental y compararlas con aquellas que constituían el motivo de derivación con pacientes diagnosticados de cáncer de piel (carcinoma espinocelular, carcinoma basocelular y melanoma) durante un año en una consulta de dermatología. Se recogieron diferentes variables y se realizó el análisis estadístico mediante la prueba de la Ji cuadrado de Pearson comparando el grupo en el que el diagnóstico era el motivo de derivación frente al grupo en el que el diagnóstico fue hallazgo incidental.
ResultadosSe recogieron datos de 433 pacientes, con una mediana de edadde 72 años, con 233 (51,3%) pacientes del sexo femenino y un predominio de fototipos II y III. El carcinoma basocelular fue en todos los análisis la neoplasia más frecuente, representando un 68,4% (296/433). Un 26% de los tumores cutáneos malignos diagnosticados no estaban relacionadas con el motivo de derivación. El análisis estadístico demostró que las diagnosticadas de forma incidental estaban localizadas en zonas no visibles, tenían un menor tamaño y menor tiempo de evolución.
ConclusionesLa alta tasa de cáncer de piel diagnosticado de forma incidental por el dermatólogo resalta la necesidad de realizar exploraciones exhaustivas a nuestros pacientes para facilitar la detección temprana y el tratamiento precoz.
Dermatologic disease is one of the main reasons for primary care (PC) visits, accounting for approximately between 7% and 8% of all visits, making it the 6th or 7th most frequent specialization seen in PC.1 Family physicians, therefore have a major role to play in the evaluation of their patients’ skin problems and referral to the dermatologist when necessary.
In particular, consultations relating to skin cancer, due to its high prevalence, are a frequent reason for referral. According to the meta-analysis by Tejera-Vaquerizo et al,2 the raw global rates of basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma in Spain were 113.05, 38.16, and 8.82 per 100,000 persons per year, respectively.
Despite the increasing use of dermatoscopy in PC, the appropriate training is not always available. When this is added to the fact that lesions may be asymptomatic or with little clinical expression, they may be missed by the patients themselves, their family members, and even health care professionals.
At the same time, dermatologists may have the feeling that we diagnose malignant skin tumors “accidentally” in patients referred to us for other reasons, with no relation to the reason for the consultation. The main objective of this study, therefore, was to determine the proportion of “incidental” diagnoses of skin cancer in patients referred for other reasons, and to compare the clinical, demographic, and epidemiological differences with patients referred with that diagnosis.
Materials and MethodsWe performed a cross-sectional, prospective, descriptive observational study of all skin cancers diagnosed in referred patients on the first visit to the dermatology department of Hospital Universitario Son Llàtzer between February 1, 2018 and January 31, 2019. The study recorded the study variables in a database of anonymized and dissociated data. The study was approved by the research ethics committee of the Balearic Islands.
A total of 8 dermatologists took part in the study. All 8 were attached to the department according to their usual clinical practice and therefore carried out skin examinations oriented toward the reason for the consultation but which might vary depending on the dermatologist responsible, the age of the patient, and/or the patients personal and family history, but without any established protocol that included a full examination of all patients. This study only included melanoma, BCC, SCC, keratoacanthoma and Bowen disease; other types of skin cancer were excluded from the analysis because they are rare, such as Merkel cell carcinoma, dermatofibrosarcoma protuberans, cutaneous metastases, and porocarcinoma.
The study’s main variable was the manner in which the skin cancer was diagnosed: if it was diagnosed by the physician who referred the patient for evaluation by the dermatologist, it was classified in the “reason for consultation” group; if it was diagnosed during the dermatology examination carried out due to another diagnosis in the initial visit, it was classified in the “incidental” group.
The other variables recorded were date of consultation (day/month/year), gender (male or female), age (continuous variable in years), skin Fitzpatrick type (I-VI, with subsequent categorization into light Fitzpatrick types I-III vs. dark Fitzpatrick types IV-VI), prior personal history of skin cancer (yes vs. no), referral priority (urgent, preferent, or normal), who first observed the lesion (patient, family member, family doctor, or other health care professional), time since onset (continuous variable in months, with subsequent categorization into more or less than 6 months), location (head/neck, upper and lower extremities, back and, anterior torso), size (continuous variable in cm, with subsequent categorization into greater or smaller than 1 cm and greater than 2 cm), suspected diagnosis of referring physician, symptoms (pruritus, bleeding, ulceration, pain), and final diagnosis (melanoma, BCC, SCC, keratoacanthoma, or Bowen disease). Although diagnosis was confirmed by histology in the vast majority of cases, in some superficial BCC, the diagnosis was clinical and dermatoscopic.
A descriptive analysis of all the data was performed (frequency and percentage of the qualitative variables, centralization and dispersion measures of the quantitative variables) and descriptive study of all the variables analyzed in these groups and a statistical analysis of the distribution differences of those variables according to the defined groups were then performed. To this end, the Pearson χ2 test was used and statistical significance was set at P < .05. The SPSS statistical package, v. 23 was used.
ResultsOverall Analysis of Patients Diagnosed With Skin CancerA total of 433 patients were included in the analysis, with a slight predominance of women (222/433, 51.3%) and a median age of 71 years (range, 26-101 years). The most common Fitzpatrick skin type was type II (46.9%), followed by type III (44.6%), IV (7.4%), V (0.9%), and just 1 patient with Fitzpatrick type VI (0.2%). A total of 27.7% (120/433) presented a past history of skin cancer (Table 1).
General Characteristics of Patients Diagnosed With Skin Cancer. Summary of Characteristics of the Patients by Sex, Age, Fitzpatrick Type, and Personal History of Skin Cancer.
| [0,1,2]Total number of patients | 437 | |
| [0,1,2]Age, x ± SD (range) | 70 ± 0.6 (26-101) | |
| [0,1,2]Sociodemographic variables | n (%) | |
| [1,0]Sex | Female | 222 (51.3) |
| Male | 211 (48.7) | |
| [4,0]Fitzpatrick type | II | 203 (46.9) |
| III | 193 (44.6) | |
| IV | 32 (7.4) | |
| V | 4 (0.9) | |
| VI | 1 (0.2) | |
| [1,0]History of skin cancer | Yes | 120 (27.7) |
| No | 313 (72.3) | |
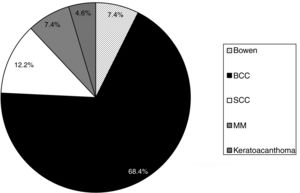
BCC was the most frequently diagnosed tumor, at 68.3% (296/433) of cases, followed by SCC with 12.2%, (53/433), Bowen disease with 7.4% (32/433), melanoma with 7.4% (32/433), and keratoacanthoma with 4.6% (20/433) (Fig. 1).
In terms of clinical signs and symptoms, 63.27% (274/433) of the lesions were asymptomatic, with no pruritus, bleeding, ulceration, or pain. However, 28.4% (123/433) of patients reported bleeding on at least one occasion, 27.9% (121/433) reported ulceration, 21.5% (93/433) reported pruritus, and 7.6% (33/433) reported pain.
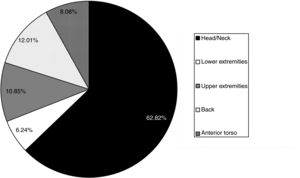
Time since onset was longer than 6 months in 62.4% (270/433) of cases and only 1.6% of lesions had appeared less than 1 month earlier. With regard to location, 62.8% (272/433) of the lesions were on the head and neck, 12% (52/433) on the back, 10.9% (47/433) on the upper extremities, 8.08% (35/433) on the anterior torso, and 6.23% (27/433) on the lower extremities (Fig. 2). In terms of size, 52.9% (229/433) of the lesions measured less than 1 cm and 12% (52/433) exceeded 2 cm.
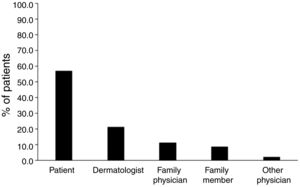
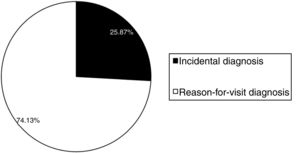
With regard to who first observed the lesion, in 57% (247/433) of cases, it was the patient, followed by the dermatologist in 23.3% (101/433) of cases, the family physician in 11.1% (48/433) of cases, a family member in 8.5% (37/433) of cases, and other physicians in last place, with 2.07% (9/433) of cases (Fig. 3). A total of 25.9% (112/433) of the malignant skin tumors diagnosed were not linked to the reason for which the patients had been referred to the dermatologist, i.e., the referral form made no mention of this suspicion; these were therefore considered to be an incidental diagnosis (Fig. 4).
No differences were observed between the 2 groups in terms of sex or personal history of skin cancer. The mean age for the reason-for-referral group was 70 ± 0.4 years (range, 26-101 years), slightly higher than in the incidental group, which was 68 ± 0.6 years (range, 30-67 years). No significant differences were detected in terms of Fitzpatrick skin types.
With regard to detection of the lesion, significant differences were found (P ≤ .05); the lesion was detected slightly more often by the dermatologist in the incidental group and by the patient in the reason-for-referral group. In this variable, the data were distributed as follows: in the incidental group, in 70% (79/112) of cases, the dermatologies was the main person responsible, followed by the patient in 24.1% (27/112) of cases, and family members in 3.6% (2/112) of cases. In the reason-for-referral group, however, the patient was the main person responsible for detecting the lesion in 68.5% (220/321) of cases, followed by the family physician in 14.3% (46/321) of cases and a considerable percentage of family members, at 10.3% (33/321) of cases.
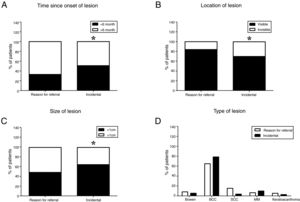
Significant differences (P < .05) were also found in time since onset (Fig. 5A), location of lesions in visible areas 5B), and size (Fig. 5C). No between-group differences were found in terms of symptoms of pruritus, pain, ulceration, or bleeding.
Characteristics of the lesions by reason for consultation. A) Time since onset of lesion. B) Location of lesion. C) Size of lesion. D) Type of lesion. The χ2 statistical test was performed to compare the reason-for-referral group with the incidental group (*P < .05 when analyzing both groups).
Finally, BCC was the most frequently diagnosed skin tumor in both the reason-for-referral group and the incidental group, with 64.8% (208/321) and 78.6% (88/112), respectively. In both groups, SCC was the second most commonly diagnosed tumor, with 15.3% (49/321) and 3.6% (4/112) in the reason-for-referral and incidental groups, respectively (Fig. 5D). Melanoma accounted for 9.8% (11/112) of tumors diagnosed in the incidental group compared to 6.5% (21/321) in the reason-for-referral group.
DiscussionTo our knowledge, this is the first study of this type carried out in Spain. A notable finding is that approximately 1 out of every 4 (25.9%) patients diagnosed with skin cancer in the dermatology consultation had been referred for another reason (incidental diagnosis) and the tumor was not linked to the reason indicated in the referral by the referring physician. This result differs from that obtained in the study by Viola et al.,3 which analyzed lesions individually (not by patient, as in our study) of the total number of visits referred to dermatology due to suspected malignant lesions and found 40.9% of malignant skin tumors diagnosed incidentally. The results of that study are therefore not comparable to those of our study, as, although those authors detected a total of 149 malignant lesions in 98 patients, with 40.9% (61/149) of incidental lesions, we must take into account the fact that if the lesions had been counted individually by patient, the percentage would be smaller, as many of those patients presented multiple lesions. It should also be noted that the study by Kingsley-Loso et al.,4 which analyzed 2257 patients who presented a total of 3328 incidental biopsied lesions over a period of 8 years and 3 months. The results of that study indicated that 50.8% of histologically confirmed incidental lesions were malignant skin tumors, with 6.9% of incidental malignant skin tumors confirmed by biopsy individually for each patient.
The mean age of approximately 70 years and the predominance of clear Fitzpatrick skin types are factors that may predispose to a higher risk of developing skin cancer, despite the fact that only 27.7% had a personal history of skin cancer.
With regard to detection of the lesions, the results place the dermatologists as the main person involved in 70% of incidental findings, highlighting the importance of complete physical skin examinations in the consultation, regardless of the reason for referral and especially when the patient has a personal history of skin cancer. This fact agrees with the study by Oliveria et al.,5 which found that dermatologists had a higher rate of detection of skin cancer compared to PC physicians and internal-medicine specialists.
Furthermore, in our study, the patient was aware of the presence of the lesion in only 24% of the incidental skin tumors. This fact highlights the need to promote skin-cancer detection campaigns, aimed at patients and family members, with the aim of achieving early diagnosis. Moreover, the studies show that screening for skin cancer is associated with lower mortality and better long-term results.6 However, factors such as the low priority given to preventing skin cancer in PC and/or the low rate of detection of malignant lesions may make this process more difficult.7 Other factors such as the short amount of time in PC consultations and the presence of other patient comorbidities also contribute to this.
With regard to the different types of skin cancer, as in other studies,3,8 BCC was the most frequently diagnosed tumor and melanoma the least frequently diagnosed, accounting for 9.8% of incidental diagnoses in our series—a value that coincides with the results obtained by Viola et al.3 Nevertheless, some studies have found different results, such as that by Cherian et al.,9 which performed a retrospective analysis over 12 months of complete skin examinations compared to those oriented only toward the reason for referral. In that study, the results indicated that of the total of 94 melanomas, 60.6% (57/94) were diagnosed incidentally and most of them (71.9%) were in situ melanomas.9 Moreover, another study confirmed that greater access to the dermatologist (defined as 1 additional dermatologist per 10,000 inhabitants) was associated with a 39% increase in melanomas diagnosed in the initial stages.10 All these results show again the benefits and results of good screening for skin cancer.11
Looking at both comparison groups, we found that the incidental group had a higher percentage of BCC (78.6% compared to 64.8% in the reason-for-referral group) and a smaller percentage of SCC and melanoma. This is probably due to the fact that dermatologists have greater experience in diagnosing BCC, which may go unnoticed by other non-dermatologist physicians, as the lesions are sometimes less clinically expressive, unlike squamous cell carcinoma or melanoma, which are usually fast-growing lesions or lesions with clinical alarm signs that lead patients to visit the physician because of them.
The data in our study show that 66.4% of the tumors for which patients were referred were located predominantly on the head and neck, revealing a tendency also observed in other studies3,8 to consult due to lesions located in easily visible areas. On the other hand, in the incidental group, tumors had a greater tendency to be located in nonvisible areas, such as the back.
It was also observed that, in the incidental group, a greater percentage of the lesions (51% compared to 33% of those that were the reason for the referral) showed a time since onset of less than 6 months and were also smaller, probably due to the fact that patients tend to consult a physician due to larger lesions and smaller lesions tend to go unnoticed. In those diagnosed by the dermatologist alone, however, it was not possible to determine the time since onset. Moreover, the delay between the referral and the visit to the specialist may have contributed to the fact that the skin tumors diagnosed in the reason-for-referral group showed a greater time since onset than the other group.
Also of interest, though with a different objective than our study, is a study by Tejera et al.,12 in which 22.7% of patients presented an additional reason for consultation, where eczema was the most common, at 17.2%, followed by alopecia at 11.5%, and evaluation of melanocytic nevus at 10.3%. Surprisingly, in that study, only 2.3% of patients requested additional evaluation of BCC.
Finally, it should be mentioned that this study was carried out based on the routine clinical practice of each dermatologist, and no special and/or more detailed skin examinations were carried out because it was an observational study. In this regard, the study carried out by Helm et al.13 is worth mentioning. In that study, those authors propose an outline for performing complete skin examinations in an orderly manner, with the goal of improving efficiency and thus reducing the probability of missing a part of the body.
ConclusionsSkin cancer is a common cause for referral to dermatology. The high rate of skin cancer diagnosed incidentally by the dermatologist highlights the need to carry out thorough examinations of our patients to facilitate early detection and treatment. This fact also highlights the importance of promoting skin-cancer prevention programs and greater training of PC professionals in detecting this type of lesion and in the use of the dermatoscope.
Conflicts of InterestThe authors declare that they have no conflicts of interest and that no funding was required for this study.
The authors would like to thank Maria Fiorella Sarubbo and Khaoulah El Hayi (Research Unit of Hospital son Llàtzer- Idisba) for their assistance in the statistical analysis of the data and revision of the article. They would also like to thank Alex Llambrich, Antonia Vila, Elisabet Parera, Ignacio Torné, Antoni Nadal and Vicenç Rocamora for taking part in collecting the data during the study period.
Please cite this article as: Vila-Payeras A, Domínguez C, Solà A, Nadal C, Taberner R. Evaluación de la tasa de detección incidental de cáncer cutáneo: estudio prospectivo en un servicio hospitalario. Actas Dermosifiliogr. 2020;111:496–502.