Cutaneous squamous cell carcinoma (cSCC) constitutes a serious public health problem, as it is the 2nd most frequent skin cancer. Few studies have assessed epidemiological indicators of cSCC in Southern Europe. The objectives of this study were to analyze its incidence rate and estimate survival of cSCC cases from all Spanish population-based cancer registries that register this cancer.
Materials and methodsWe conducted a retrospective descriptive study of all incident first cSCC cases registered in Girona, Granada, Navarre and Tarragona (Spain) from 1994 to 2017. Crude and age-standardized (ASR-E) incidence rates were calculated. Incidence trends were analyzed using joinpoint regression. Observed survival was estimated using the Kaplan–Meier method and relative survival was estimated using the Ederer II method.
ResultsA total of 22,343 cSCC cases (61.5% men) were registered, accounting for 20.3% of all skin cancers. The most common anatomical site was the skin of face, scalp and neck (59.1%) and the incidence rate increased exponentially with age. The annual ASR-E per 100,000 inhabitants was 25.0 in women and 56.6 in men. Both sexes showed a significant upward incidence trend, with an annual percent change of +2.0% (95%CI, +1.6% to +2.4%). The 5-year relative survival rate was 93.5% (95%CI, 92.5–94.6%), slightly higher in women, and did not seem to increase over time.
ConclusionsThis study provides an updated description of cSCC incidence and survival, which are key indicators to frame the scenario of this cancer in Spain. Overall, results are consistent with former studies, showing a rising trend in the incidence rate alongside high survival rates. Further research is warranted to elucidate the causes underlying these findings.
Cutaneous squamous cell carcinoma (cSCC) is a type of non-melanoma skin cancer that originates from malignant proliferation of epidermal keratinocytes and arises in actinically damaged skin. After a prolonged latency period, cSCC progresses through local invasion, followed by systemic dissemination via perineural invasion, hematogenous metastasis or lymphatic metastasis 1. Its metastatic rate has been estimated at 1–5% 2. Invasive disease often manifests as a persistent ulcer, a non-healing wound, or a fast-growing tumor 3. The clinical presentation of cSCC, along with its prognosis, are influenced by tumor factors such as location, histological subtype and degree of differentiation, and host factors, such as immune status 3,4. Biopsy and histopathologic examination are considered the gold standard for definitive diagnosis. The therapeutic approach depends on the tumor aggressiveness—for low-risk cSCC, surgery is recommended as the first-line therapy and systemic therapy is generally not needed, whereas management of high-risk cSCC usually comprises surgical excision and/or radiotherapy, as well as lymph node dissection (besides, chemo- and immunotherapy may be required) 5.
From an epidemiological standpoint, cSCC constitutes a serious public health problem, as it is the 2nd most frequent skin cancer and the second cause of death among skin cancers. In 2022, the age-standardized incidence rate (ASR) of non-melanoma skin cancer, excluding basal cell carcinoma, was 10.4 cases per 100,000 population worldwide and 14.2 cases per 100,000 in Europe, according to the Global Cancer Observatory 6. The vast majority of such cases correspond to cSCC. In Spain, the incidence rate in the same year was reported to be well below the European average, with an estimated ASR of 9.1 cases per 100,000 6. Unlike incidence rates, neither global nor Europe-specific survival estimates are available, as nonmelanoma skin cancers are typically excluded from major international population-based cohort studies. Consequently, survival rates are generally estimated only at the national or subnational level. According to national estimates from European countries, the 5-year relative survival (RS) rate of cSCC is about 90% 7,8. The main risk factors for cSCC development are advanced age, lifetime exposure to ultraviolet radiation, sun-sensitive skin and immunosuppression, in particular solid organ transplantation 4. Additional risk factors include certain skin conditions, various groups of pollutants, tobacco smoking and therapeutic ionizing radiation 1,3.
Registration of cSCC is not common practice in cancer registries; international trends in incidence rate, albeit rising, may underestimate the true incidence rates 9. In addition, low generalizability is a common limitation of results obtained from hospital registries—to quantify valid estimates representative of the general population, information from population-based cancer registries should be used. However, in the Southern European context, literature on this topic is scarce. In fact, the only population-based study evaluating the incidence and survival of cSCC conducted in Spain was based on a single registry and analyzed non-melanoma skin cancer data up to 2012 10. Hence the need to address this evidence gap with updated population-based epidemiological indicators from Spain.
The objectives of this study were to analyze incidence rates and incidence trends, and to estimate survival rates of cSCC cases from all Spanish population-based cancer registries that register cSCC.
Materials and methodsPopulation, data sources and variablesWe conducted a retrospective descriptive study of all incident cases of cSCC registered in 4 Spanish provinces—Girona, Granada, Navarre and Tarragona (Supplementary data 1)—from 1994 through 2017. The following International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) skin cancer sites were included: face, scalp and neck (C44.0-4), trunk (C44.5), arm and shoulder (C44.6), leg and hip (C44.7) and overlapping lesion or not otherwise specified (NOS) (C44.8-9). Of note, we did not include cases of cSCC in the genital area, which includes the skin of vulva, penis or scrotum, as these cancer sites are classified elsewhere (ICD-O-3 codes C51, C60.9 and C63.2, respectively).
Incidence data were retrieved from the Girona, Granada, Navarre and Tarragona population-based cancer registries (PBCR), which began their activity in 1994, 1985, 1970 and 1980, respectively. The joint population covered by the four PBCR at the end of the study period represents 6.7% of the overall population residing in Spain. These PBCR apply standard cancer registry procedures and coding rules: for skin cancer, only the first tumor of a defined histological type per patient is counted as an incident cancer 11. Data from these PBCR is regularly published in the International Agency for Research on Cancer (IARC) monographs “Cancer Incidence in Five Continents” 12. In addition, these PBCR are members of the Spanish (REDECAN) and the European Network of Cancer Registries (ENCR). To study the incidence rate of cSCC, we included sex, age at diagnosis (categorized into 5-year intervals), anatomical site, histological subtype, most valid source for diagnosis, year of diagnosis and province.
Mortality data and population data were extracted from the Spanish National Institute of Statistics (http://www.ine.es). For each province, the population as of July 1st of each year was used. Passive and active follow-up of cases was conducted from the date of diagnosis to the date of last known vital status until December 31st, 2017. The former was conducted using the National Death Index of the Spanish Ministry of Health (https://www.sanidad.gob.es/) and mortality registries, while the latter was conducted through revision of health records and administrative databases. To study cSCC survival, sex, age at diagnosis (categorized into 5-year intervals 13), anatomical site, most valid source for diagnosis, date of diagnosis, date of last contact recorded, vital status and province were included.
Statistical analysisCrude incidence rates and age-standardized incidence rates (by the direct method) were estimated using the standard European population of 2013 (ASR-E) and the standard world population of 1960 (ASR-W) as reference. Age-specific rates were also calculated. To analyze trends in ASR-E, we used log-linear joinpoint regression models, which estimate the annual percent change (APC) alongside its 95% confidence interval (CI) 14.
Cases known to the registries only through death certificates (death certificate only [DCO] cases) and those diagnosed at autopsy were excluded from the survival analysis. Observed survival, which accounts for all causes of death, and relative survival, which estimates survival assuming cancer as the sole cause of death, were both calculated. The Kaplan–Meier method was used to estimate observed survival rates, and the Ederer II method15 was applied to estimate relative survival rates. The Ederer II method estimates cSCC survival in the theoretical absence of other causes of death by incorporating life tables for competing mortality probabilities in Spain (stratified by year, sex, age, and province), providing a clearer estimate of survival specifically attributable to cSCC.
All statistical tests were two-sided and p-values<0.05 were considered significant. Statistical analyses were performed using Stata software version 17 and R software version 4.3.3, with the exception of trend analysis, which was performed in Joinpoint software version 4.9. Figures were produced using the R package ‘ggplot2’.
ResultsBetween 1994 and 2017, a total of 22,434 individuals developed an index cSCC, accounting for 21.7% of all non-melanoma skin cancers and 20.3% of all skin cancers (for context, cutaneous basal cellular carcinoma accounted for 76.4% of all non-melanoma skin cancers and 71.3% of all skin cancers during the study period). In men (N=13,804, 61.5%), median age at diagnosis was 77 years (IQR, 69–83); in women (N=8630, 38.5%), it was 81 years (IQR, 73–86).
Incidence rate of cSCCTable 1 illustrates the distribution of cases by age group, anatomical site and histological subtype. Most cases occurred in subjects aged≥75 as the age group with the highest number of incident cases was 75–84 years, in which 8521 cases (38.0%) were diagnosed, followed by ≥85 years, with 5697 cases (25.4%). Most cancers (59.1%) were located in the skin of face, scalp and neck in both sexes, with a higher frequency observed in men (63.6%) compared to women (51.9%). Next, overlapping lesions of skin or not otherwise specified (NOS) accounted for 23.1% of all cancers. Among less common sites, it is noteworthy that the frequency of cSCC of the skin of leg and hip varied by sex, with women showing higher values (9.9%) than men (2.6%). The most frequent histological subtype was SCC, NOS (84.6%), followed by keratinizing SCC (7.3%) and microinvasive SCC (5.0%).
Description of cases of cutaneous squamous cell carcinoma registered in Girona, Granada, Navarre and Tarragona, 1994–2017.
| Characteristic | Both sexes | Women | Men |
|---|---|---|---|
| N=22,434 (100.0%) | N=8630 (38.5%) | N=13,804 (61.5%) | |
| Age, years | |||
| 15–24 | 12 (0.1%) | 4 (0.0%) | 8 (0.1%) |
| 25–34 | 52 (0.2%) | 29 (0.3%) | 23 (0.2%) |
| 35–44 | 241 (1.1%) | 95 (1.1%) | 146 (1.1%) |
| 45–54 | 770 (3.4%) | 275 (3.2%) | 495 (3.6%) |
| 55–64 | 1983 (8.8%) | 569 (6.6%) | 1414 (10.2%) |
| 65–74 | 5136 (22.9%) | 1544 (17.9%) | 3592 (26.0%) |
| 75–84 | 8521 (38.0%) | 3197 (37.1%) | 5324 (38.6%) |
| ≥85 | 5697 (25.4%) | 2903 (33.7%) | 2794 (20.3%) |
| Unknown | 22 (0.1%) | 14 (0.2%) | 8 (0.1%) |
| Anatomical site | |||
| Skin of face, scalp and neck (C44.0-4) | 13,262 (59.1%) | 4480 (51.9%) | 8782 (63.6%) |
| Skin of lip (C44.0) | 450 (2.0%) | 108 (1.3%) | 342 (2.5%) |
| Skin of eyelid (C44.1) | 481 (2.1%) | 218 (2.5%) | 263 (1.9%) |
| Skin of ear and external auricular canal (C44.2) | 1976 (8.8%) | 184 (3.1%) | 1792 (13.0%) |
| Skin of other and unspecified parts of face (C44.3) | 7610 (33.9%) | 3582 (41.5%) | 4028 (29.2%) |
| Skin of scalp and neck (C44.4) | 2745 (12.2%) | 388 (4.5%) | 2357 (17.1%) |
| Skin of trunk (C44.5) | 958 (4.3%) | 401 (4.6%) | 557 (4.0%) |
| Skin of arm and shoulder (C44.6) | 1808 (8.1%) | 819 (9.5%) | 989 (7.2%) |
| Skin of leg and hip (C44.7) | 1218 (5.4%) | 855 (9.9%) | 363 (2.6%) |
| Overlapping lesion of skin or NOS (C44.8-9) | 5188 (23.1%) | 2075 (24.0%) | 3113 (22.6%) |
| Overlapping lesion of skin (C44.8) | 137 (0.6%) | 52 (0.6%) | 85 (0.6%) |
| Malignant neoplasm of skin, unspecified (C44.9) | 5051 (22.5%) | 2023 (23.4%) | 3028 (21.9%) |
| Histological subtype | |||
| Verrucous SCC | 105 (0.5%) | 31 (0.4%) | 74 (0.5%) |
| SCC, NOS | 18,974 (84.6%) | 7240 (83.9%) | 11,734 (85.0%) |
| Keratinizing SCC | 1643 (7.3%) | 609 (7.1%) | 1034 (7.5%) |
| Non-keratinizing large cell SCC | 60 (0.3%) | 29 (0.3%) | 31 (0.2%) |
| Non-keratinizing small cell SCC | 4 (0.0%) | 1 (0.0%) | 3 (0.0%) |
| Spindle cell SCC | 108 (0.5%) | 37 (0.4%) | 71 (0.5%) |
| Acantholytic SCC | 252 (1.1%) | 82 (1.0%) | 170 (1.2%) |
| Microinvasive SCC | 1118 (5.0%) | 521 (6.0%) | 597 (4.3%) |
| SCC with horn formation | 70 (0.3%) | 31 (0.4%) | 39 (0.3%) |
| Adenosquamous carcinoma | 5 (0.0%) | 3 (0.0%) | 2 (0.0%) |
| Lymphoepithelioma-like carcinoma | 10 (0.0%) | 7 (0.1%) | 3 (0.0%) |
| Clear cell SCC | 85 (0.4%) | 39 (0.5%) | 46 (0.3%) |
Anatomical site codes refer to the International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3). NOS: not otherwise specified; SCC: squamous cell carcinoma.
The annual incidence rate of cSCC was estimated at a crude rate per 100,000 inhabitants of 25.5 cases in women and 41.1 cases in men. These rates underwent a substantial growth over the study period, especially in men, rising from 32.2 in the first sub-period (1994–2001) to 49.7 cases in the third sub-period (2010–2017), while they increased from 18.8 cases to 31.6 in women. In regard to age-standardized rates per 100,000, larger sex differences were observed, with a yearly ASR-E of 25.0 cases in women and 56.6 in men (male to female ratio, 2.3:1). Similar to the crude rates, ASR-E augmented over time, although to a lesser extent, from 20.3 to 28.2 and from 47.1 to 62.7 in women and men, respectively. Crude and age-standardized rates, overall and by period, are shown in Table 2. In addition, incidence rate showed some geographical variation, with ASR-E values ranging between 34.5 cases per 100,000 in Granada and 44.4 in Tarragona (Supplementary data 2). Supplementary data 2 displays crude and standardized rates by anatomical site, histological subtype and province.
Incidence rates of cutaneous squamous cell carcinoma per 100,000 in Girona, Granada, Navarre and Tarragona, 1994–2017.
| Period | Both sexes | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|---|
| CR | ASR-E | ASR-W | CR | ASR-E | ASR-W | CR | ASR-E | ASR-W | |
| 1994–2001 | 25.4 | 31.6 | 11.1 | 18.8 | 20.3 | 6.7 | 32.2 | 47.1 | 16.5 |
| 2002–2009 | 32.2 | 38.0 | 13.0 | 24.9 | 24.9 | 8.2 | 39.6 | 56.0 | 19.1 |
| 2010–2017 | 40.6 | 42.7 | 14.1 | 31.6 | 28.2 | 9.2 | 49.7 | 62.7 | 20.1 |
| Overall (1994–2017) | 33.3 | 38.2 | 12.9 | 25.5 | 25.0 | 8.2 | 41.1 | 56.6 | 18.8 |
Incidence rates are expressed per 100,000. ASR-E: age-standardized rates taking the 2013 European population as reference; ASR-W: age-standardized rates taking the 1960 world population as reference; CR: crude rates.
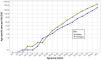
Incidence rate increased with age exponentially, according to age-specific rates (Fig. 1 and Supplementary data 3). The highest rates were found in the age group of 85+ years, with 313.8 cases per 100,000 in women and 612.1 in men. Although incidence rate was higher in men across the age spectrum, young adults were an exception, as age-specific rates were higher in women (30–34 years: 0.9 vs 0.4) or equal in both sexes (35–39 years: 1.4 vs 1.4).
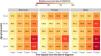
The trend analysis (Fig. 2 and Table 3) revealed that the upward incidence trend was statistically significant: the APC values of ASR-E were 2.1% (95%CI, 1.6–2.4) in women and 1.9% (95%CI, 1.7–2.6) in men. However, not all anatomical sites and histological subtypes followed this overall incidence trend. As shown in Table 3, a biphasic trend (i.e., with one joinpoint) was identified for several subtypes: overlapping lesions or not otherwise specified (NOS), the incidence of which stabilized after 2004; keratinizing cSCC, which showed a marked increase between 2013 and 2017; and microinvasive cSCC, for which a decrease was observed during the same period.
Incidence trends of cutaneous squamous cell carcinoma in Girona, Granada, Navarre and Tarragona, 1994–2017.
| Characteristic | Both sexes | Women | Men | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Period | APC | 95%CI | Period | APC | 95%CI | Period | APC | 95%CI | |
| Anatomical site | |||||||||
| Skin of face, scalp and neck (C44.0-4) | 1994–2017 | 1.4 | 1.0;1.8* | 1994–2017 | 1.1 | 0.6;1.7* | 1994–2017 | 1.5 | 1.0;1.9* |
| Skin of trunk (C44.5) | 1994–2017 | 4.4 | 3.2;5.7* | 1994–2017 | 6.3 | 4.4;8.2* | 1994–2017 | 3.1 | 1.7;4.5* |
| Skin of arm and shoulder (C44.6) | 1994–2017 | 2.0 | 1.2;2.9* | 1994–2017 | 1.9 | 0.8;2.9* | 1994–2017 | 2.0 | 0.9;3.1* |
| Skin of leg and hip (C44.7) | 1994–2017 | 2.8 | 1.8;3.9* | 1994–2017 | 3.1 | 1.8;4.3* | 1994–2017 | 1.9 | −0.1;4.1 |
| Overlapping lesion of skin or NOS (C44.8-9) | 1994–2004 | 8.8 | 5.2;12.5* | 1994–2004 | 8.6 | 5.1;12.2* | 1994–2000 | 16.4 | 4.8;29.3* |
| 2004–2017 | 0.3 | −1.2;1.8 | 2004–2017 | 0.5 | −1.0;2.0 | 2000–2017 | 1.1 | −0.3;2.5 | |
| Histological subtype | |||||||||
| SCC, NOS | 1994–2017 | 1.8 | 1.4;2.2* | 1994–2017 | 1.9 | 1.5;2.4* | 1994–2017 | 1.7 | 1.2;2.1* |
| Keratinizing SCC | 1994–2013 | −0.8 | −2.3;0.8 | 1994–2013 | −1.1 | −3.0;0.8 | 1994–2013 | −0.7 | −2.7;1.3 |
| 2013–2017 | 29.7 | 16.0;45.1* | 2013–2017 | 30.6 | 14.2;49.3* | 2013–2017 | 29.2 | 11.6;49.4* | |
| Microinvasive SCC | 1994–2012 | 5.4 | 2.0;8.9* | 1994–2012 | 6.0 | 1.5;10.7* | 1994–2013 | 4.3 | 1.2;7.4* |
| 2012–2017 | −16.8 | −30.7;−0.1* | 2012–2017 | −16.9 | −33.2;3.3 | 2013–2017 | −19.9 | −40.9;8.5 | |
| Overall | 1994–2017 | 2.0 | 1.6;2.4* | 1994–2017 | 2.1 | 1.7;2.6* | 1994–2017 | 1.9 | 1.5;2.3* |
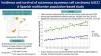
Median observed survival (OS) of cSCC cases was 7 years and 9 months, whereas the 5-year OS were 64.1% (95%CI, 63.0–65.3%) in women and 64.5% (95%CI, 63.6–65.5%) in men. OS seemed to decrease over time, as 5-year survival rates went from 66.4% (95%CI, 65.4–67.5) in 2002–2009 to 62.9% (95%CI, 61.9–63.8%) in 2010–2017. When disaggregating results by age, great differences in OS were noted: 5-year OS ranged from 52.4% (≥75 years) to 94.9% (15–44 years). Furthermore, it also pointed at sex differences, especially in the younger age groups. As expected, 5-year OS was higher in men aged 15–44 than in those aged 45–54. However, the opposite was true for women, with the 15–44 age group having a lower OS than the 45–54 group (93.2%; 95%CI, 88.2–98.6% vs 97.2%; 95%CI, 95.0–99.4%, respectively); of note, this difference was small and both 95%CI overlapped. Fig. 3 illustrates the OS curves by sex and age group, whereas the OS by anatomical site is shown in Supplementary data 4.
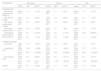
Regarding relative survival (RS), 5-year RS was estimated at 93.5% (95%CI, 92.5–94.6%) and was marginally higher in women (94.7%; 95%CI, 93.0–96.4%) vs men (92.8%; 95%CI, 91.5–94.1%). Although RS seemed to decline slightly in both sexes, as 5-year RS shifted from 95.6% (95%CI, 94.1–97.2%) between 2002 and 2009 to 92.0% (95%CI, 90.6–93.4%) between 2010 and 2017, this decrease vanished at 10 years. The age-stratified analysis found that RS was generally higher at earlier ages (in fact, rates below 90% were only observed in those ≥65 years) (Fig. 4). Nevertheless, the values of 2 age strata were similar to that of older individuals: women aged 15–44 years, who had a 5-year RS of 93.5% (95%CI, 88.4–98.9%), and men aged 45–54 years, whose 5-year RS was 93.4% (95%CI, 90.5–96.4%). Table 4 illustrates 1-, 3-, 5- and 10-year RS rates, overall, by period and by age group. The equivalent RS rates according to anatomical site are presented in Supplementary data 4.
Observed and relative survival of cutaneous squamous cell carcinoma in Girona, Granada, Navarra and Tarragona, 1994–2017.
| Characteristic | Time (years) | Both sexes (N=17,440) | Women (N=6767) | Men (N=10,673) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | OS (95%CI) | RS (95%CI) | N | OS (95%CI) | RS (95%CI) | N | OS (95%CI) | RS (95%CI) | ||
| Age group | ||||||||||
| 15–44 | 1 | 211 | 97.7 (95.7;99.7) | 97.8 (95.8;99.8) | 88 | 97.8 (94.7;100.0) | 97.8 (94.8;100.0) | 124 | 97.6 (95.0;100.0) | 97.7 (95.1;100.0) |
| 3 | 207 | 95.8 (93.2;98.5) | 96.1 (93.5;98.8) | 85 | 94.4 (89.7;99.3) | 94.6 (89.9;99.4) | 123 | 96.8 (93.8;99.9) | 97.0 (94.0;100.0) | |
| 5 | 193 | 94.9 (92.0;97.9) | 95.4 (92.5;98.4) | 82 | 93.2 (88.2;98.6) | 93.5 (88.4;98.9) | 112 | 96.0 (92.7;99.5) | 96.7 (93.4;100.0) | |
| 10 | 124 | 92.5 (88.9;96.2) | 93.8 (90.1;97.6) | 54 | 93.2 (88.2;98.6) | 94.0 (88.9;99.4) | 71 | 91.9 (86.9;97.2) | 93.5 (88.4;98.9) | |
| 45–54 | 1 | 557 | 98.2 (97.2;99.3) | 98.5 (97.4;99.6) | 215 | 100.0 (100.0;100.0) | 100.0 (100.0;100.0) | 342 | 97.2 (95.4;98.9) | 97.5 (95.8;99.2) |
| 3 | 539 | 95.1 (93.3;96.9) | 95.9 (94.1;97.7) | 213 | 98.6 (97.1;100.0) | 99.0 (97.5;100.0) | 327 | 92.9 (90.2;95.6) | 93.9 (91.3;96.7) | |
| 5 | 491 | 93.6 (91.6;95.7) | 95.2 (93.2;97.3) | 197 | 97.2 (95.0;99.4) | 98.1 (95.9;100.0) | 295 | 91.4 (88.6;94.4) | 93.4 (90.5;96.4) | |
| 10 | 286 | 88.4 (85.6;91.3) | 92.1 (89.2;95.2) | 111 | 94.9 (91.9;98.1) | 97.2 (94.1;100.0) | 176 | 84.4 (80.4;88.7) | 89.0 (84.7;93.5) | |
| 55–64 | 1 | 1424 | 97.8 (97.1;98.6) | 98.5 (97.8;99.3) | 434 | 98.0 (96.7;99.3) | 98.3 (97.0;99.6) | 991 | 97.7 (96.8;98.7) | 98.6 (97.7;99.5) |
| 3 | 1372 | 94.2 (93.0;95.4) | 96.4 (95.2;97.6) | 422 | 95.2 (93.3;97.3) | 96.3 (94.3;98.3) | 951 | 93.8 (92.3;95.3) | 96.5 (94.9;98.0) | |
| 5 | 1233 | 91.1 (89.6;92.6) | 94.9 (93.4;96.5) | 385 | 94.3 (92.2;96.5) | 96.3 (94.1;98.5) | 849 | 89.7 (87.8;91.6) | 94.4 (92.4;96.4) | |
| 10 | 725 | 83.5 (81.5;85.6) | 92.6 (90.3;94.9) | 231 | 91.6 (88.8;94.4) | 96.4 (93.5;99.4) | 495 | 80.2 (77.6;82.9) | 91.0 (88.0;94.0) | |
| 65–74 | 1 | 3658 | 97.3 (96.8;97.9) | 99.1 (98.5;99.6) | 131 | 98.3 (97.5;99.0) | 99.2 (98.4;99.9) | 2529 | 96.9 (96.3;97.6) | 99.0 (98.3;99.7) |
| 3 | 3411 | 90.8 (89.8;91.7) | 96.1 (95.1;97.0) | 120 | 93.5 (92.1;94.9) | 96.4 (94.9;97.8) | 2337 | 89.6 (88.4;90.8) | 95.9 (94.6;97.1) | |
| 5 | 2913 | 84.4 (83.2;85.6) | 93.6 (92.3;94.9) | 107 | 89.0 (87.2;90.8) | 94.4 (92.5;96.3) | 1975 | 82.4 (80.9;83.8) | 93.3 (91.6;95.0) | |
| 10 | 1413 | 65.9 (64.2;67.7) | 86.9 (84.7;89.2) | 57 | 75.3 (72.6;78.2) | 89.4 (86.1;92.8) | 929 | 61.8 (59.7;63.9) | 85.7 (82.8;88.7) | |
| ≥75 | 1 | 10,251 | 89.5 (89.0;90.1) | 99.2 (98.6;99.8) | 4371 | 89.8 (88.9;90.6) | 99.2 (98.3;100.0) | 5880 | 89.4 (88.7;90.1) | 99.1 (98.3;100.0) |
| 3 | 7901 | 69.0 (68.2;69.9) | 95.4 (94.2;96.5) | 3394 | 69.7 (68.4;71.0) | 95.7 (93.9;97.5) | 4508 | 68.6 (67.5;69.7) | 95.1 (93.6;96.7) | |
| 5 | 5476 | 52.4 (51.5;53.3) | 93.1 (91.4;94.7) | 2378 | 53.5 (52.1;54.9) | 94.4 (92.0;96.9) | 3099 | 51.5 (50.3;52.8) | 92.0 (89.9;94.2) | |
| 10 | 1425 | 23.0 (22.1;23.9) | 88.8 (85.3;92.3) | 654 | 24.6 (23.2;26.1) | 92.9 (87.8;98.4) | 772 | 21.7 (20.6;22.9) | 85.5 (81.0;90.2) | |
| Period | ||||||||||
| 2002–2009 | 1 | 6791 | 92.5 (91.9;93.1) | 99.3 (98.6;99.9) | 2610 | 92.1 (91.1;93.1) | 99.4 (98.3;100.0) | 4182 | 92.7 (92.0;93.5) | 99.2 (98.4;100.0) |
| 3 | 5750 | 78.3 (77.4;79.3) | 97.2 (96.1;98.4) | 2191 | 77.3 (75.8;78.9) | 97.4 (95.5;99.4) | 3560 | 78.9 (77.8;80.1) | 97.0 (95.6;98.5) | |
| 5 | 4879 | 66.4 (65.4;67.5) | 95.6 (94.1;97.2) | 1845 | 65.1 (63.4;66.9) | 96.0 (93.4;98.6) | 3035 | 67.3 (65.9;68.7) | 95.4 (93.5;97.4) | |
| 10 | 3121 | 42.5 (41.4;43.7) | 89.3 (87.0;91.7) | 1189 | 42.0 (40.2;43.9) | 91.1 (87.3;95.1) | 1933 | 42.8 (41.4;44.3) | 88.2 (85.3;91.3) | |
| 2010–2017 | 1 | 9306 | 92.2 (91.6;92.7) | 98.9 (98.4;99.5) | 3626 | 92.2 (91.4;93.0) | 99.0 (98.1;99.9) | 5680 | 92.1 (91.5;92.8) | 98.9 (98.1;99.6) |
| 3 | 7676 | 76.0 (75.2;76.9) | 94.6 (93.5;95.6) | 2995 | 76.1 (74.8;77.5) | 94.9 (93.3;96.6) | 4682 | 76.0 (74.9;77.1) | 94.3 (93.0;95.7) | |
| 5 | 5425 | 62.9 (61.9;63.8) | 92.0 (90.6;93.4) | 2133 | 63.4 (61.9;65.0) | 93.8 (91.6;96.1) | 3292 | 62.5 (61.3;63.7) | 90.9 (89.1;92.7) | |
| 10 | 850 | 38.3 (37.0;39.6) | 89.7 (86.7;92.8) | 343 | 39.2 (37.2;41.4) | 95.6 (90.6;100.0) | 508 | 37.7 (36.0;39.4) | 86.0 (82.3;89.9) | |
| Overall | 1 | 16,097 | 92.3 (91.9;92.7) | 99.1 (98.6;99.5) | 6235 | 92.2 (91.5;92.8) | 99.2 (98.5;99.9) | 9862 | 92.4 (91.9;92.9) | 99.0 (98.5;99.5) |
| 3 | 13,426 | 77.0 (76.4;77.6) | 95.7 (94.9;96.5) | 5185 | 76.6 (75.6;77.7) | 96.0 (94.8;97.3) | 8242 | 77.2 (76.4;78.0) | 95.5 (94.5;96.5) | |
| 5 | 10,302 | 64.4 (63.7;65.1) | 93.5 (92.5;94.6) | 3977 | 64.1 (63.0;65.3) | 94.7 (93.0;96.4) | 6327 | 64.5 (63.6;65.5) | 92.8 (91.5;94.1) | |
| 10 | 3970 | 40.5 (39.7;41.3) | 88.9 (87.2;90.8) | 1531 | 40.8 (39.5;42.2) | 92.7 (89.7;95.7) | 2440 | 40.3 (39.3;41.4) | 86.6 (84.4;88.9) | |
Survival estimates are expressed as percentages (%). CI: confidence interval; OS: observed survival; RS: relative survival.
We found that cSCC mainly occurred in patients aged≥75 years and the anatomical site of most cases was the skin of face, scalp and neck. The ASR-E in men doubled that of their female counterparts, and a significant upward trend in incidence was found. In addition, cSCC incidence rate varied by province, with Tarragona showing an ASR-E almost 30% greater than Granada's. Within-country geographical variation in cSCC has been documented previously and could be related to factors such as social deprivation, education and population density 16–18. Our work is not the first attempt to report on the incidence rate of cSCC in Spain 19. An analysis of non-melanoma skin cancer incidence trends in Spain has been published recently 20, but estimates from the Global Burden of Disease study constituted the sole source of information. Given the aforementioned limitations of cSCC data availability and quality, the discussion focuses on studies based on cancer registries.
Incidence rate of non-melanoma skin cancer was previously studied in a PBCR from Spain—Girona Cancer Registry, one of the 4 registries included in this study. Vilar-Coromina et al. analyzed incidence trends between 1994 and 2007 21. Yearly incidence rates of cSCC were slightly below that in our study and a significant increasing trend in both sexes (APC, +4.2% in women; APC, +3.8% in men) was reported. Later, Rubió-Casadevall et al. provided a detailed description of this phenomenon and extended the study up to 2012 10. Among cases of cSCC, the most common site was the skin of face, scalp and neck. In addition to finding similar incidence rates, a rising trend that reached statistical significance in men (APC, +1.6%) was identified. Of note, this increasing trend in the incidence rate of cSCC in Spain mirrors that of cutaneous malignant melanoma, although the latter seems to vary to a greater extent by geographical area 22,23.
With a broader scope, Olsen et al. examined trends in the incidence rate of cSCC across 7 countries between 1989 and 2020 9. Incidence rate of cSCC in our study was relatively similar to that of Nordic countries, most notably Finland in recent years, where the ASR-E per 100,000 was 26.3 cases in women and 49.1 in men. A mean APC for the overall study period in Nordic countries ranging from +1.8% to +6.1% in women and from +2.4% to +4.4% in men was reported. Besides, a study analyzed trends of keratinocyte skin cancers in the UK between 2013 and 2018 24. The ASR-E per 100,000 person-years was more than double in men than in women, whereas the mean APC for both sexes shifted from +6.7% to +3.3%. Beyond the European context, Sella et al. studied incidence trends of keratinocyte skin cancers in Israel (2006–2011) 25. Compared to our findings, they reported a lower median age at diagnosis and higher incidence rates in both sexes.
The incidence trends observed in this study may reflect improvements in diagnosis, treatment (the only subtype that shifted to a decreasing trend was microinvasive cSCC, possibly due to the adoption of non-surgical treatment modalities) and registration over time. On the other hand, changes in exposure to ultraviolet radiation are considered a salient cause of the increase in cSCC incidence. These are in turn influenced by several factors, including outdoor occupations, tanning-related risk behaviors and population aging 1,26,27. Occupational exposure deserves a special mention as a major determinant of incidence that could explain sex differences 28. Besides, changes in health care, social and environmental factors might play an ancillary role.
Regarding survival, we found that OS was highly dependent on age; surprisingly, women aged 15–44 years had a slightly lower OS than those aged 45–54. RS was 93.5% at 5 years, with slightly higher values in women. It did not seem to increase over time; in fact, 5-year RS in our study decreased slightly from 2010 onwards. Rubió-Casadevall et al. 10 reported a 5-year RS of cSCC in Girona of 90.1%, without clear differences according to sex. The evolution of RS over time was not reported. Survival of non-melanoma skin cancer between 1997 and 2011 was analyzed in a large study including data from 12 PBCR throughout Germany 7. 5-Year RS was estimated at 93.6%, with slightly higher values in women vs men. An interesting finding was that RS was found to increase with age. However, the authors acknowledged that the underreporting of deaths likely caused an overestimation of RS, especially in older age groups. In England, van Bodegraven et al. found that 5-year net survival was 89.8%, comparable to that of cutaneous melanoma (including melanoma in situ) 8; survival rates by sex were not reported. Additionally, a nationwide population-based study calculated survival rates of primary cutaneous malignancies in South Korea up to 2019 29. For cSCC, 5-year RS showed a steady increase over time, increasing from 77.3% (1996–2000) to 89.3% (2016–2019); survival rates by sex were not reported.
Although survival in patients with cSCC from this study was high and age-dependent, the plateau observed since 2010 and the lower rates in women aged 15–44 suggest the importance of early diagnosis. This is particularly relevant for patients with risk factors such as immunosuppression and for young patients with diagnostic delay. Yet, an added challenge that increases the burden of cSCC for health care professionals is that patients at risk for aggressive disease are difficult to identify: current staging systems to predict metastasis show positive predictive values between 4.5% and 13.2% 30. Hence the need to implement strategies to improve early diagnosis, including patient health education 31, screening in high-risk individuals, use of dermoscopy in primary care 32 and teledermatology 33.
Strengths and limitationsThe strengths of our study include the use of PBCR as data source, which ensure that the population studied is highly representative of the inhabitants of each province, and its multicenter design, covering areas from various autonomous communities. However, this study also has some limitations. First, data on clinical variables (e.g., stage at diagnosis) 34 and social characteristics (e.g., occupation) 35 were not available, limiting the depth of the epidemiological description. Since only the first tumor is counted as an incident cancer and cases of cSCC in certain anatomical sites are not recorded as such in cancer registries, this also leads to a likely underestimation of the clinical relevance and associated costs 36. Second, poor data quality on histological subtype (>80% of cases were classified as SCC, NOS) prevented us from conducting survival analyses stratified by subtypes with known prognostic relevance. For example, spindle cell (sarcomatoid), adenosquamous, and acantholytic cSCC subtypes are associated with a higher risk of aggressive disease, whereas verrucous and clear cell cSCC are considered low-risk variants.37 Third, although we analyzed the influence of age and period on incidence and survival, we did not assess the potential cohort effect (e.g., the interaction between age and period) using age–period–cohort models.
ConclusionsThis population-based study from 4 cancer registries provides an updated description of cSCC incidence rate and survival, which are key epidemiological indicators to frame the scenario of this cancer in Spain. Overall, our results are fairly consistent with previous studies, showing a rising trend in cSCC incidence alongside high survival rates. Further research is warranted to elucidate the causes underlying these findings.
Conflict of interestThe authors declare that they have no conflict of interest.