The search for practical approaches in medical education is fundamental in undergraduate medical teaching, especially in dermatology, where visual inspection is key.1,2 Case-based learning is a methodology that exposes students to real-world scenarios, promoting a practical approach. This fosters the acquisition and application of knowledge without endangering patients, making the implementation of virtual resources essential.3–9
Technology aims to support and optimize teaching through the use of the internet and various devices.10 While this transformation from conventional to digital education systems takes time to develop, its advancement became a training priority during the COVID-19 pandemic.4–9
Currently, there is limited evidence on the effectiveness of digital learning in dermatology. This led us to design and evaluate the impact on learning of a virtual tool called the “dermatological league” (DL).
This project involved 5th-year medical students from the 2020 to 2021 academic year. The curriculum consisted of a daily case including clinical images and 3 multiple-choice questions with 4 options, a single correct answer, and a penalty for errors. Cases were published online after the corresponding theoretical explanation, and students had 24h to answer them remotely via the virtual campus, accessible through smartphones, tablets, and other digital devices. After this time, they were notified of their score and received a ranking that ordered them in descending classification. The cases remained accessible on the website as review material along with a brief explanation. To encourage participation, a series of incentives were established for the top-ranked students, including cosmetic kits, dermatology books, or extra points towards the final exam grade. To avoid disadvantaging students who chose not to participate, the DL score was not included as a percentage of the final grade. The course grade was based entirely on a final exam comprising a theoretical part and a practical part with images similar to the DL cases.
To evaluate the impact on learning, questionnaires of 10 case reports were administered before and after the competition, and anonymous surveys were conducted to assess student satisfaction with the activity.
For statistical analysis, parametric methods such as the Student t test for paired and independent samples and Spearman's correlation were used via the SPSS.v.20 software.
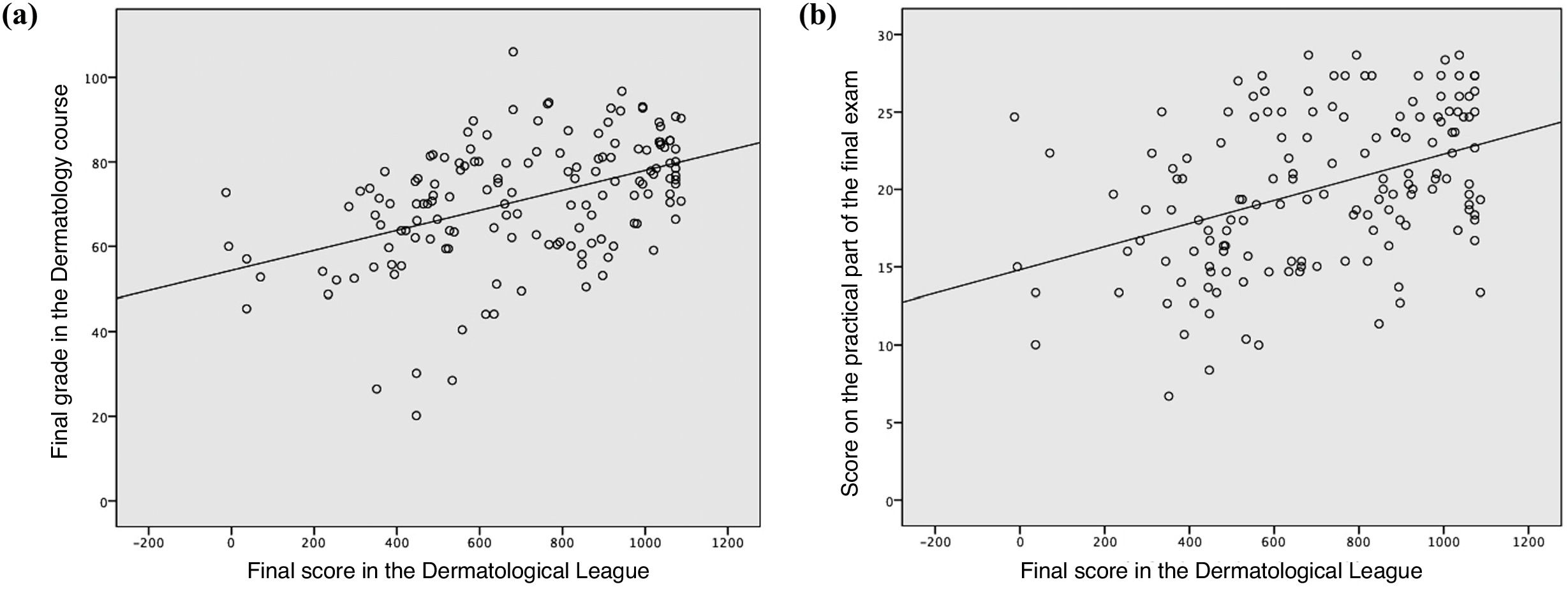
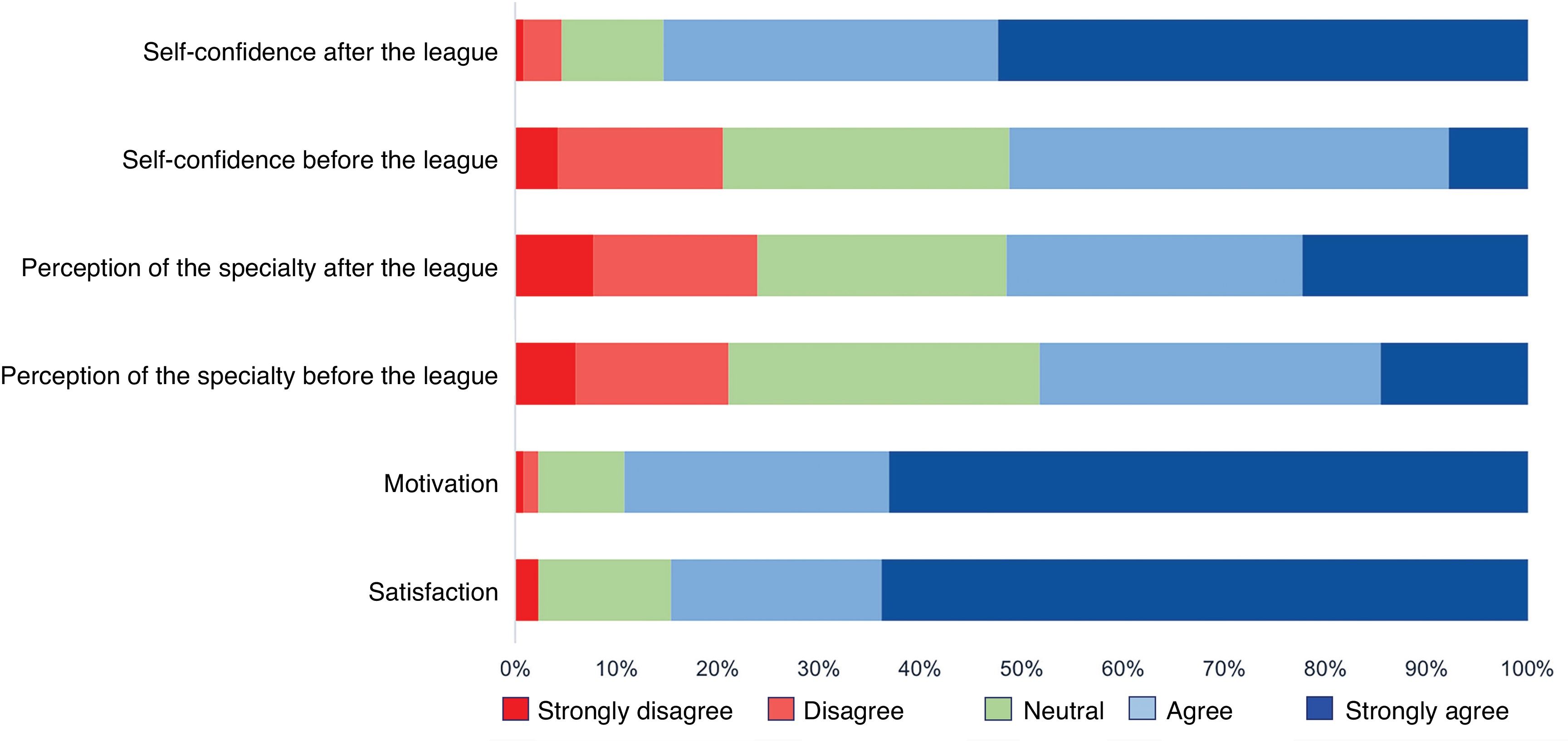
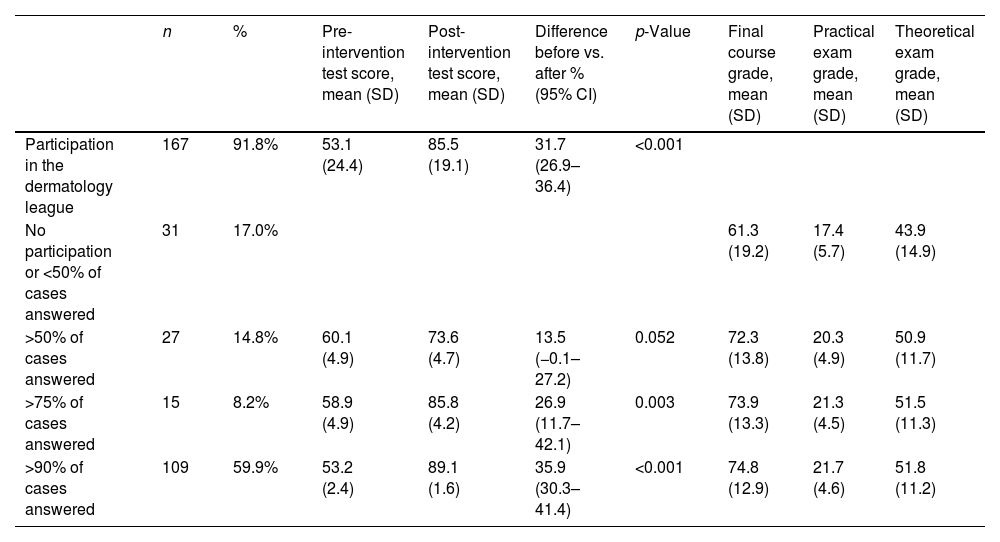
A total of 167 (91.8%) of the 182 students in the course participated in the project (Table 1). The mean score on the case report questionnaires prior to the intervention improved from 53.1% to 85.5% after completing the competition (p<0.001). Academic grades for the course were higher among students who participated in the virtual tool and, within this group, were better among those with greater adherence to the activity (p=0.0001). Furthermore, grades positively correlated with the score obtained in the DL, with this correlation being stronger for the practical part of the final exam (p=0.001) (Fig. 1). A total of 85% of students reported feeling comfortable solving case reports after completing the DL. A total of 51% expressed interest in the specialty of dermatology, and up to 89% reported increased motivation to study (Fig. 2).
Participation rates and final outcomes after the implementation of the “dermatology league”.
| n | % | Pre-intervention test score, mean (SD) | Post-intervention test score, mean (SD) | Difference before vs. after % (95% CI) | p-Value | Final course grade, mean (SD) | Practical exam grade, mean (SD) | Theoretical exam grade, mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|
| Participation in the dermatology league | 167 | 91.8% | 53.1 (24.4) | 85.5 (19.1) | 31.7 (26.9–36.4) | <0.001 | |||
| No participation or <50% of cases answered | 31 | 17.0% | 61.3 (19.2) | 17.4 (5.7) | 43.9 (14.9) | ||||
| >50% of cases answered | 27 | 14.8% | 60.1 (4.9) | 73.6 (4.7) | 13.5 (−0.1–27.2) | 0.052 | 72.3 (13.8) | 20.3 (4.9) | 50.9 (11.7) |
| >75% of cases answered | 15 | 8.2% | 58.9 (4.9) | 85.8 (4.2) | 26.9 (11.7–42.1) | 0.003 | 73.9 (13.3) | 21.3 (4.5) | 51.5 (11.3) |
| >90% of cases answered | 109 | 59.9% | 53.2 (2.4) | 89.1 (1.6) | 35.9 (30.3–41.4) | <0.001 | 74.8 (12.9) | 21.7 (4.6) | 51.8 (11.2) |
Students’ experience and perception regarding participation in the DL activity. Multiple items were evaluated (confidence, perception of the specialty, motivation, and degree of satisfaction). Students’ confidence regarding their ability to tackle practical cases was assessed using the following questions: “Did you improve your confidence in solving practical clinical cases?” “Did the virtual curriculum activity develop other skills, such as research or clinical–pathological concepts?”. The perception of the dermatology specialty was assessed through these questions: “Did the virtual teaching activity generate interest in you in the field of dermatology?” “Do you find dermatology an appealing specialty?” Student motivation was assessed with the following questions: “The competitive format of the Dermatological League motivated my participation and teamwork with my classmates.” “The Dermatological League in the virtual curriculum motivated me to study dermatology daily.” Finally, the degree of satisfaction with the activity was assessed through these questions: “Would you like to participate again in a teaching activity with a similar format?” “Would you recommend the activity to other students who will follow the curriculum in the next academic year?”.
The observed positive impact of the DL on student learning has also been reported in other studies that evaluated other virtual learning modalities, such as “flipped classrooms.” In this teaching method, students review material before class and then have a more personalized conversation with the professor.4–6
Increasing student motivation has been one of the main objectives of research on learning outcomes in medical education. A positive correlation between the 2 has been described in studies conducted with university students in various fields outside of Medicine.10 In our study, participants reported feeling more motivated to study due to the practical and competitive approach of our tool. They also showed greater self-confidence and a stronger preference for the specialty of dermatology. By fostering participation in the learning process, these teaching strategies based on gamification formats have been increasing considerably in recent years.2
The results obtained suggest that the DL is an effective didactic strategy for acquiring practical knowledge among students.
Virtual education modalities could provide easy access to medical content with a wide variety of information, which is key in training the new generation of digital natives, especially in situations of mobility restriction or social distancing, as occurred during COVID-19.
Conflicts of interestNone declared.
We thank the students for their commitment to the project and their authorization to publish the data collected in this manuscript.