Atopic dermatitis (AD) affects both children and adults. The main symptom of this disease is pruritus, which impacts health-related quality of life (HRQOL). The aim of this study was to evaluate the impact of AD on the lives of children and adults with this disease.
Patients and methodsThis was a multicenter prospective epidemiological study of children (2-17 years) and adults (≥ 18 years) with AD selected from dermatology offices in Spain. The patients had all had AD for at least a year and had no other chronic inflammatory skin diseases.
In addition to sociodemographic information, the data collected included the clinical features of AD and the results of patient-centered questionnaires: the Itch Severity Scale (ISS), the Dermatology Life Quality Index (DLQI), and the children's version of this questionnaire (cDLQI).
ResultsWe studied 151 children and 172 adults. The mean (SD) age of the children was 9.4 (4.5) years and 51.7% were boys. In the case of adults, the mean age was 32.3 (13.4) years and 58.7% were women.
Among the children, the ISS score increased with disease severity and in the adults, both the frequency and intensity of pruritus increased with disease severity (P<.05 in both cases); 79% of the children and 87.1% of the adults reported difficulty sleeping.
In both populations, overall and subscale DLQI and cDLQI scores varied according to disease severity.
ConclusionsAD affects HRQOL in both children and adults and its impact is correlated with the presence and intensity of pruritus.
La dermatitis atópica (DA) puede afectar tanto a niños como a adultos. Su principal síntoma es el prurito, afectando la calidad de vida relacionada con la salud (CVRS) de los pacientes. El presente manuscrito pretende evaluar el impacto de la DA en la vida de los pacientes, tanto pediátricos como adultos.
Pacientes y métodosEstudio epidemiológico, prospectivo, multicéntrico, en consultas de Dermatología. Se seleccionaron pacientes pediátricos (2-17 años) y adultos (≥18 años) con DA de más de un año de evolución, sin otra patología inflamatoria crónica dermatológica.
Se recogieron variables sociodemográficas, clínicas de la DA y centradas en el paciente (cuestionarios Itch Severity Scale [ISS] y Children's Dermatology Life Quality Index [cDLQI] o Dermatology Life Quality Index [DLQI]).
ResultadosSe incluyeron 151 pacientes pediátricos y 172 pacientes adultos. Los pediátricos tenían una edad media (DE) de 9,4 (4,5) años y el 51,7% eran niños; los adultos tenían una edad media (DE) de 32,3 (13,4) años y el 58,7% eran mujeres.
Entre los pediátricos la puntuación del ISS aumenta con la gravedad (p<0,05); el 79% presentaban dificultad para conciliar el sueño.
En adultos la frecuencia e intensidad del prurito fue superior, presentando más diferencias según la gravedad (p<0,05); el 87,1% presentaba dificultades para conciliar el sueño.
En ambas poblaciones se observaron diferencias en la puntuación global y por dimensiones del DLQI/cDLQI según la gravedad de la enfermedad.
ConclusionesLa DA afecta la CVRS de los pacientes, tanto pediátricos como adultos, correlacionándose con la presencia e intensidad del prurito.
Atopic dermatitis (AD) is a chronic inflammatory skin disorder that mainly affects children, although it also occurs in adults. A recent study of patients presenting at dermatology clinics in Spain reported an estimated prevalence of AD of 3.4%, with rates of 16.9% in patients under 5 years of age, 7.9% in those aged between 6 and 15 years, and 1.5% in patients older than 15 years.1 The results are very similar to those reported in other studies.2,3 It has been calculated that between 2% and 15% of primary care patients in Spain4 and between 1% and 3% of the general population5 have AD.
Patients with AD (both adults and children) generally report worse health-related quality of life (HRQOL) than the general population and they also experience greater psychological stress.6 HRQOL has been seen to decrease with increasing disease severity,7 although independently of the site of the lesions.8 Children with AD often have behavioral problems, such as greater dependency, fear, limited participation in sports (with repercussions on social life), and sleep disorders, which can cause daytime sleepiness and difficulties at school.6,9 Furthermore, it has been seen that children with infant eczema have an increased risk of hyperactivity and attention-deficit disorders at the age of 10 years.10 The same children are also more prone to developing emotional and behavioral disorders when they experience sleep problems. There is no doubt that pruritus, the main symptom of AD, can affect HRQOL,11 causing considerable loss of energy, sleep disruption, and psychiatric morbidity, and at times restricting patients’ social life.12,13 Pruritus can also be a source of frustration for both physicians and patients and have a pronounced impact on HRQOL.11
The aim of the present study was to evaluate the impact of AD on the lives of children and adults by analyzing disease severity, pruritus frequency and severity, and the impact of AD and its symptoms on the HRQOL of pediatric and adult patients.
Material and MethodsThe data presented are from the PSEDA study, whose main objective was to validate the Spanish version of the Itch Severity Scale (ISS). The results of the validation study have been described elsewhere.14 The PSEDA study was a multicenter, observational, prospective epidemiological study conducted with the participation of 115 dermatology specialists from throughout Spain between October 2007 and November 2008. In the article, we describe the characteristics of the patients at the baseline visit.
The inclusion criteria for the PSEDA study were an age of over 2 years and AD diagnosed at least a year earlier according to the criteria of Hanifin and Rajka.15 Exclusion criteria were the presence of other inflammatory disorders characterized by pruritus and participation in a clinical trial at the time of enrolment. Informed consent was obtained from all patients prior to their participation in the study, which was approved by the clinical research ethics committee at Hospital Universitario de La Princesa in Madrid, Spain.
Information was collected on sociodemographic variables (age, sex, level of education, and occupational status in the case of adults); clinical variables related to AD (severity, duration, personal and family history of asthma, dry skin and/or hay fever) and concomitant conditions; and patient-centered variables based on the ISS,16 the Dermatology Life Quality Index (DLQI),17 and the children's version of this questionnaire, the cDLQI. The ISS is designed to evaluate and measure pruritus severity. It consists of 7 items covering the frequency, intensity, and characteristics of pruritus, the areas of the body affected, the degree of pruritus in its normal state, and its effect on mood, sleep, and sexual desire and function. The maximum possible score ranges from 0 (no pruritus) to 21 (very severe pruritus). In the case of children, the questionnaire was completed by the patients’ parents or guardians, with omission of question 6, which assesses the effect of pruritus on sexual desire and function.
The DLQI has also been validated in the Spanish population and can be self-administered. The questions refer to the previous 7 days. The DLQI and the children's version, the cDLQI, consist of 10 questions, which are rated on a 4-point scale ranging from 3 (very much) to 0 (not at all). The questionnaire consists of 6 domains: symptoms and feelings, daily activities, leisure, work and school, personal relationships (including sexuality), and treatment. The total possible score ranges from 0 (no effect at all on the patient's life) to 30 (extremely large effect on the patient's life).
AD severity was assessed using the modified Eczema Area and Severity Index (mEASI)18 and the investigator's global assessment (IGA). The mEASI is a modified index for evaluating the severity of eczema based on body surface area affected by lesions, morphology of lesions (erythema, papules, excoriation, and lichenification), severity of lesions (0-3), and pruritus. The scores range from 0 to 72 for the main symptoms of AD and from 0 to 18 for pruritus, giving a maximum possible score of 0 (no involvement) to 90 (maximum involvement).
The IGA was based on 6 categories, with scores ranging from 0 (no disease, no inflammatory signs of AD) to 5 (very severe disease, with intense erythema and papules/intense infiltration with crusting/exudation).
Statistical AnalysisThe SPSS software package version 9.1 for Windows was used for statistical analysis. The level of significance was set at a P value of less than .05 for all statistical tests.
We performed a descriptive analysis of the sociodemographic and clinical characteristics of the patients stratified by age group: 2 to 17 years (children) and 18 years and above (adults). Considering the differences between the 2 populations, we did not perform between-group comparisons. The impact of AD on the patients’ lives, assessed using the ISS and the DLQI or cDLQI, was analyzed following stratification of disease severity according to the IGA. Given the small number of patients in the extreme IGA categories, disease severity was classified into 3 categories: mild (no disease, almost clear, mild disease), moderate, and severe (severe and very severe disease). DLQI and cDLQI scores were classified into 5 groups according to the effect of AD on HRQOL: no effect (0-1), a small effect (2-5), a moderate effect (6-10), a very large effect (11-20), and an extremely large effect (21-30).
To investigate the characteristics and intensity of pruritus more thoroughly, each of the questions on the ISS was analyzed individually. For the first question, which assesses the frequency of pruritus (never, occasional, frequent, constant) throughout the day (morning, middle of the day, afternoon, and night), we calculated the percentage of time during which the patients had each type of pruritus. To do this, we considered that the 4 periods of the day had the same duration. Hence, if a patient had constant itching for 2 periods of the day, he or she was considered to have this type of itching for 50% of the time. Likewise, if constant itching was reported for 3 periods, the patient was considered to have this type of itching for 75% of the time.
The χ2 test was used to analyze associations between pairs of categorical variables and the Pearson correlation coefficient was used to analyze correlations between pairs of continuous variables. Relationships between continuous and categorical variables were examined by analysis of variance.
ResultsWe analyzed the results for 323 patients (151 children and 172 adults), all of whom had had AD for at least a year.
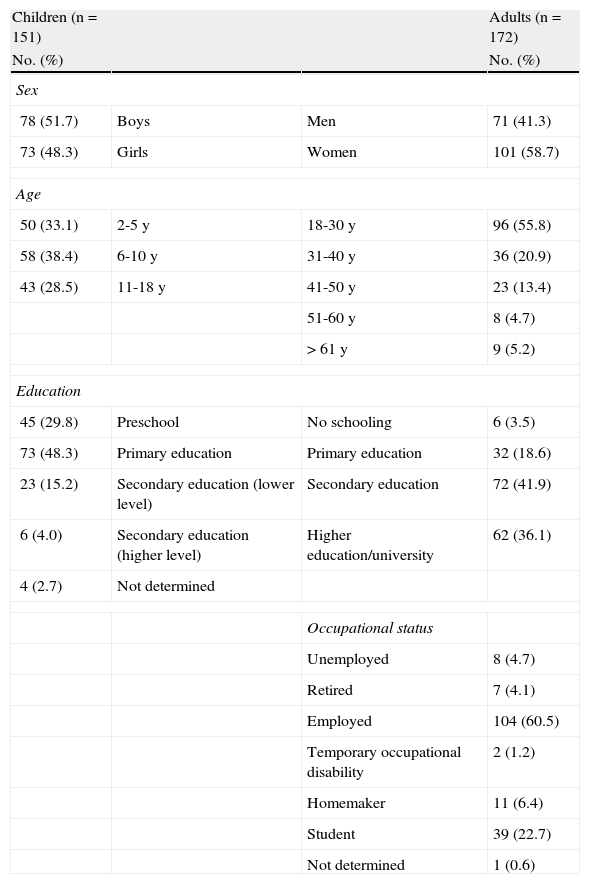
Sociodemographic CharacteristicsChildren aged 6 to 10 years accounted for the largest proportion (38.4%) of patients in the pediatric group and 51.7% were boys. The mean (SD) age of the patients in the adult group was 32.3 (13.4) years and 58.7% were women. It is noteworthy that over half of the adults (55.8%) were aged between 18 and 30 years. Table 1 shows the sociodemographic characteristics of the patients by age group (children or adults).
Sociodemographic Characteristics of Children and Adults Included in the Study.
| Children (n=151) | Adults (n=172) | ||
| No. (%) | No. (%) | ||
| Sex | |||
| 78 (51.7) | Boys | Men | 71 (41.3) |
| 73 (48.3) | Girls | Women | 101 (58.7) |
| Age | |||
| 50 (33.1) | 2-5 y | 18-30 y | 96 (55.8) |
| 58 (38.4) | 6-10 y | 31-40 y | 36 (20.9) |
| 43 (28.5) | 11-18 y | 41-50 y | 23 (13.4) |
| 51-60 y | 8 (4.7) | ||
| >61 y | 9 (5.2) | ||
| Education | |||
| 45 (29.8) | Preschool | No schooling | 6 (3.5) |
| 73 (48.3) | Primary education | Primary education | 32 (18.6) |
| 23 (15.2) | Secondary education (lower level) | Secondary education | 72 (41.9) |
| 6 (4.0) | Secondary education (higher level) | Higher education/university | 62 (36.1) |
| 4 (2.7) | Not determined | ||
| Occupational status | |||
| Unemployed | 8 (4.7) | ||
| Retired | 7 (4.1) | ||
| Employed | 104 (60.5) | ||
| Temporary occupational disability | 2 (1.2) | ||
| Homemaker | 11 (6.4) | ||
| Student | 39 (22.7) | ||
| Not determined | 1 (0.6) | ||
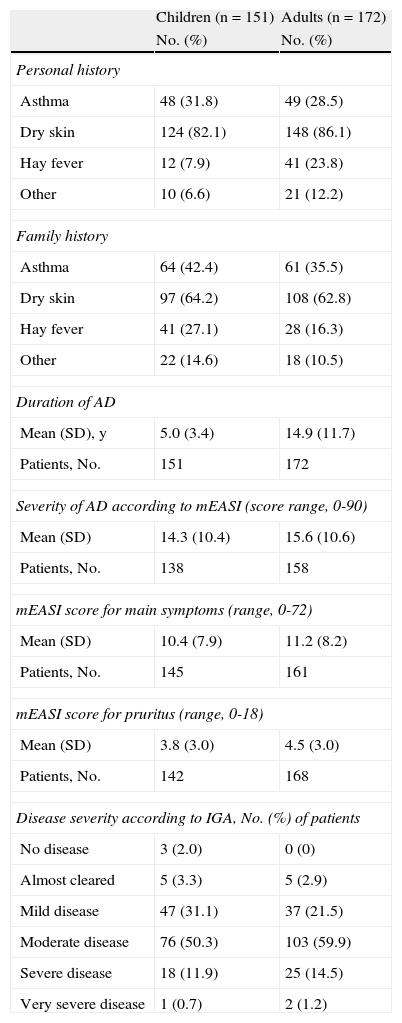
Concomitant disease was observed in 43.7% of the children and 57.6% of the adults; the most common disorders were allergies, with a prevalence of 28.5% in children and 40.1% in adults. A high percentage of patients had a personal and/or family history of asthma, dry skin, or hay fever (Table 2). The mean duration of AD was 5.0 (3.4) years in children and 14.9 (11.7) years in adults. According to the IGA, 62.9% of the children and 75.6% of the adults had moderate, severe, or very severe disease (Table 2).
Clinical Characteristics of Atopic Dermatitis (AD) of Children and Adults Included in the Study.
| Children (n=151) | Adults (n=172) | |
| No. (%) | No. (%) | |
| Personal history | ||
| Asthma | 48 (31.8) | 49 (28.5) |
| Dry skin | 124 (82.1) | 148 (86.1) |
| Hay fever | 12 (7.9) | 41 (23.8) |
| Other | 10 (6.6) | 21 (12.2) |
| Family history | ||
| Asthma | 64 (42.4) | 61 (35.5) |
| Dry skin | 97 (64.2) | 108 (62.8) |
| Hay fever | 41 (27.1) | 28 (16.3) |
| Other | 22 (14.6) | 18 (10.5) |
| Duration of AD | ||
| Mean (SD), y | 5.0 (3.4) | 14.9 (11.7) |
| Patients, No. | 151 | 172 |
| Severity of AD according to mEASI (score range, 0-90) | ||
| Mean (SD) | 14.3 (10.4) | 15.6 (10.6) |
| Patients, No. | 138 | 158 |
| mEASI score for main symptoms (range, 0-72) | ||
| Mean (SD) | 10.4 (7.9) | 11.2 (8.2) |
| Patients, No. | 145 | 161 |
| mEASI score for pruritus (range, 0-18) | ||
| Mean (SD) | 3.8 (3.0) | 4.5 (3.0) |
| Patients, No. | 142 | 168 |
| Disease severity according to IGA, No. (%) of patients | ||
| No disease | 3 (2.0) | 0 (0) |
| Almost cleared | 5 (3.3) | 5 (2.9) |
| Mild disease | 47 (31.1) | 37 (21.5) |
| Moderate disease | 76 (50.3) | 103 (59.9) |
| Severe disease | 18 (11.9) | 25 (14.5) |
| Very severe disease | 1 (0.7) | 2 (1.2) |
Abbreviations: IGA, investigator's global assessment; mEASI, modified Eczema Area and Severity Index.
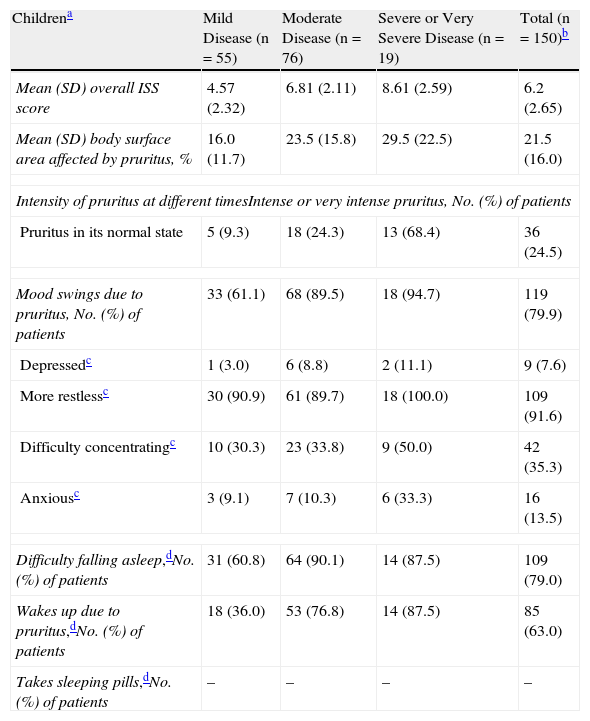
Table 3 and Figure 1 show the scores obtained by the children on the ISS, including the total score and the scores for each question, classified according to the IGA. The total ISS score increased significantly with an increase in IGA score (P<.05), indicating that more severe disease was associated with more intense pruritus. The high intensity and frequency of pruritus reported by the patients interfered with activities of daily living, with 79% of children stating that they frequently or nearly always had difficulties falling asleep and 63% stating that their itching frequently or nearly always woke them up.
Description of Characteristics and Intensity of Pruritus in Children and Adults With Atopic Dermatitis According to the Itch Severity Scale (ISS) and Classified by the Investigator's Global Assessment of Disease Severity.
| Childrena | Mild Disease (n=55) | Moderate Disease (n=76) | Severe or Very Severe Disease (n=19) | Total (n=150)b |
| Mean (SD) overall ISS score | 4.57 (2.32) | 6.81 (2.11) | 8.61 (2.59) | 6.2 (2.65) |
| Mean (SD) body surface area affected by pruritus, % | 16.0 (11.7) | 23.5 (15.8) | 29.5 (22.5) | 21.5 (16.0) |
| Intensity of pruritus at different timesIntense or very intense pruritus, No. (%) of patients | ||||
| Pruritus in its normal state | 5 (9.3) | 18 (24.3) | 13 (68.4) | 36 (24.5) |
| Mood swings due to pruritus, No. (%) of patients | 33 (61.1) | 68 (89.5) | 18 (94.7) | 119 (79.9) |
| Depressedc | 1 (3.0) | 6 (8.8) | 2 (11.1) | 9 (7.6) |
| More restlessc | 30 (90.9) | 61 (89.7) | 18 (100.0) | 109 (91.6) |
| Difficulty concentratingc | 10 (30.3) | 23 (33.8) | 9 (50.0) | 42 (35.3) |
| Anxiousc | 3 (9.1) | 7 (10.3) | 6 (33.3) | 16 (13.5) |
| Difficulty falling asleep,dNo. (%) of patients | 31 (60.8) | 64 (90.1) | 14 (87.5) | 109 (79.0) |
| Wakes up due to pruritus,dNo. (%) of patients | 18 (36.0) | 53 (76.8) | 14 (87.5) | 85 (63.0) |
| Takes sleeping pills,dNo. (%) of patients | – | – | – | – |
| Adultsa | Mild Disease (n=42) | Moderate Disease (n=103) | Severe or Very Severe Disease (n=27) | Total (n=172) |
| Mean (SD) overall ISS score | 5.75 (2.87) | 8.33 (2.94) | 11.88 (3.36) | 8.27 (3.54) |
| Mean (SD) body surface area affected by pruritus, % | 20.2 (15.0) | 28.2 (19.0) | 42.3 (29.8) | 28.5 (21.2) |
| Intensity of pruritus at different timesIntense or very intense pruritus, No. (%) of patients | ||||
| Pruritus in its normal state | 6 (14.3) | 28 (27.7) | 21 (77.8) | 55 (32.4) |
| Mood changes due to pruritus, No. (%) of patients | 30 (71.4) | 93 (90.3) | 26 (96.3) | 149 (86.6) |
| Depressedc | 2 (6.7) | 17 (18.3) | 8 (30.8) | 27 (18.1) |
| More restlessc | 23 (76.7) | 73 (78.5) | 22 (84.6) | 118 (79.2) |
| Difficulty concentratingc | 6 (20.0) | 41 (44.1) | 15 (57.7) | 62 (41.6) |
| Anxiousc | 7 (23.3) | 32 (34.4) | 15 (57.7) | 54 (36.2) |
| Impaired sexual desire, No. (% of patients) | 4 (9.8) | 23 (23.2) | 12 (46.2) | 39 (23.5) |
| Impaired sexual function, No. (% of patients) | 2 (5.0) | 18 (18.0) | 10 (38.5) | 30 (18.1) |
| Difficulty falling asleep,dNo. (%) of patients | 32 (76.2) | 89 (88.1) | 27 (100.0) | 148 (87.1) |
| Wakes up due to pruritus,dNo. (%) of patients | 23 (54.8) | 77 (76.2) | 25 (92.6) | 125 (73.5) |
| Takes sleeping pills,dNo. (%) of patients | 4 (9.5) | 21 (21.2) | 8 (30.8) | 33 (19.8) |
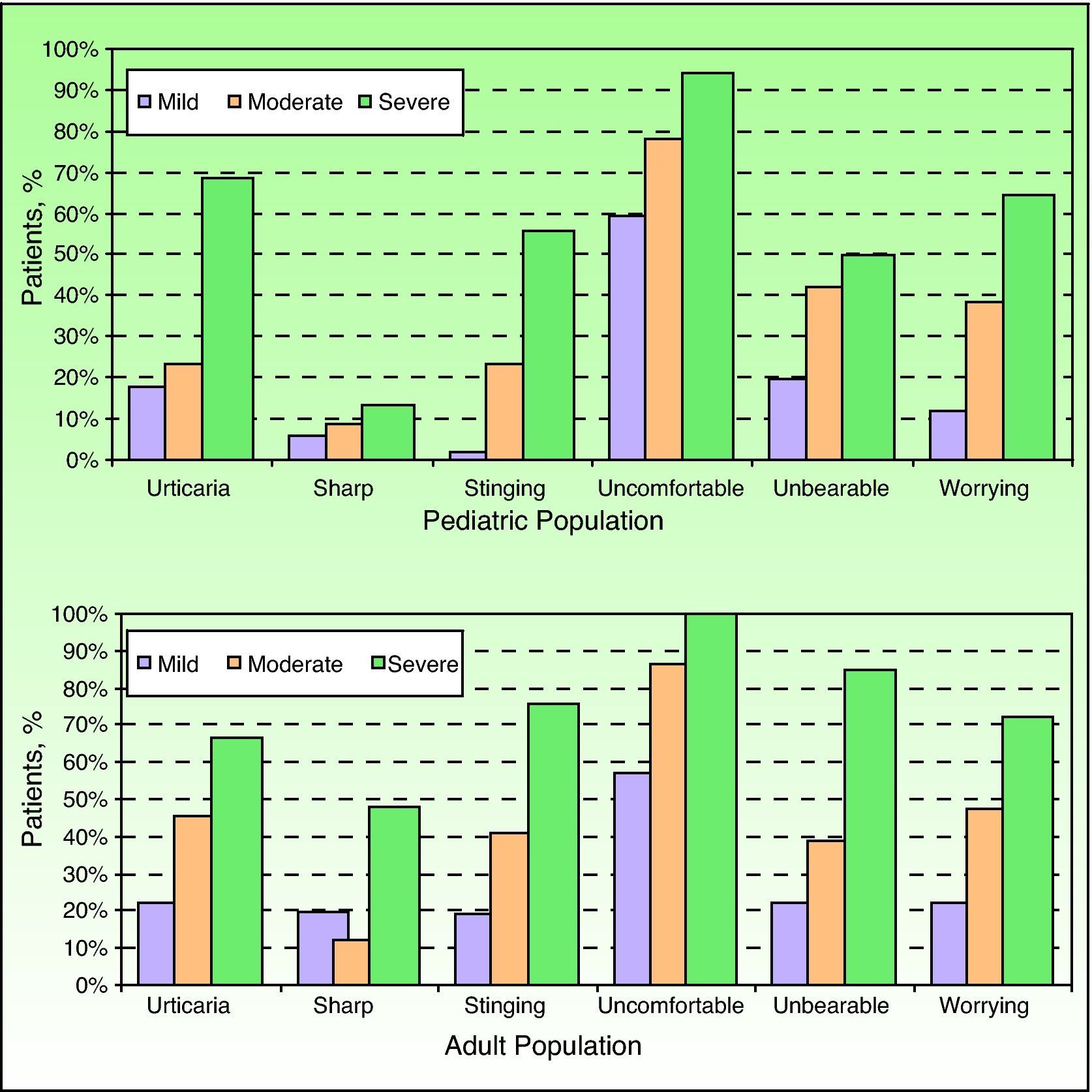
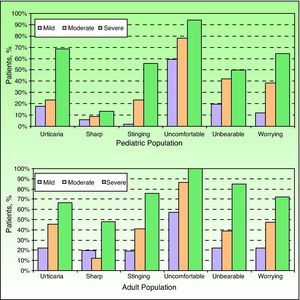
Characteristics of pruritus assessed using the Itch Severity Scale in children and adults with atopic dermatitis classified according to the investigator's global assessment of disease severity. Data are shown as the percentage of patients who answered “a little”, “moderately well”, or “very well” to the question about how well certain terms described their pruritus.
The frequency and intensity of pruritus was slightly higher in adult patients, in whom more significant differences were observed according to disease severity graded according to the IGA (P<.05) (Table 3). In the adult group, pruritus caused everyday problems related to sleep and sexual function; 87.1% of the patients stated that they frequently or nearly always had difficulties falling asleep while 73.5% stated that their itching frequently or nearly always woke them up. In addition, 19.8% said that they took sleeping pills. Finally, pruritus was reported to interfere with sexual desire in 23.5% of patients and with sexual function in 18.1%.
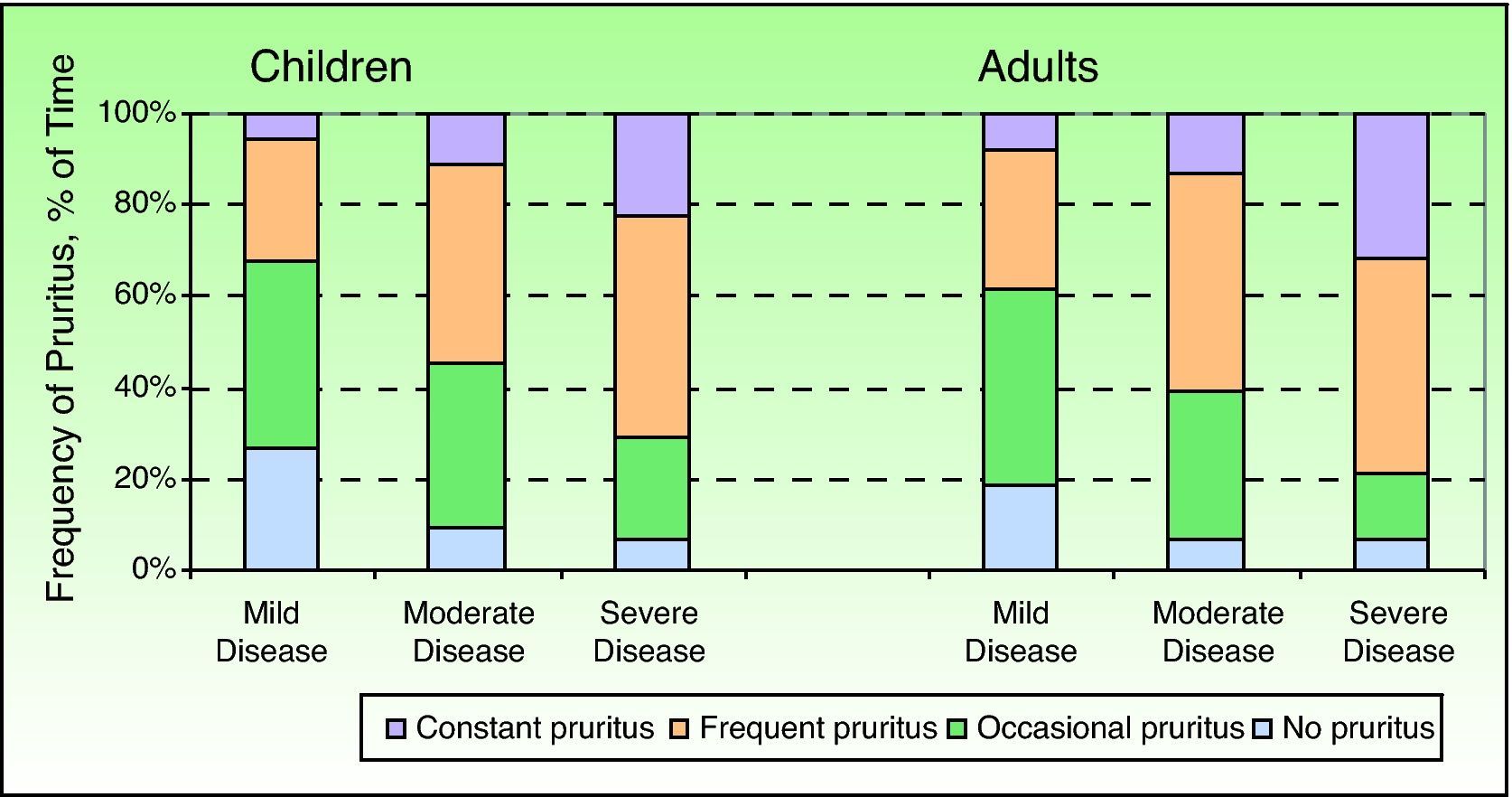
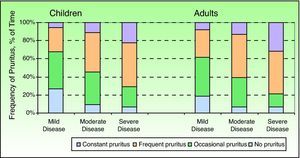
Using the answers to the first question on the ISS, we calculated the percentage of the time during which patients experienced pruritus at a given frequency. Children had no pruritus 15.5% (27.4%) of the time, occasional pruritus 36.3% (28.2%) of the time, frequent pruritus 37.5% (31.4%) of the time, and constant pruritus 10.7% (22.5%) of the time. Adults, in turn, had no pruritus 9.6% (23.1%) of the time, occasional pruritus 32.2% (30.8%) of the time, frequent pruritus 43.4% (35.8%) of the time, and constant pruritus 14.8% (26.8%) of the time. Figure 2 shows the frequency of pruritus reported by children and adults according to the IGA. In both groups, the frequency increased with disease severity, progressing from occasional or no itching in a majority of patients with mild AD to frequent or constant itching in a majority of those with severe AD.
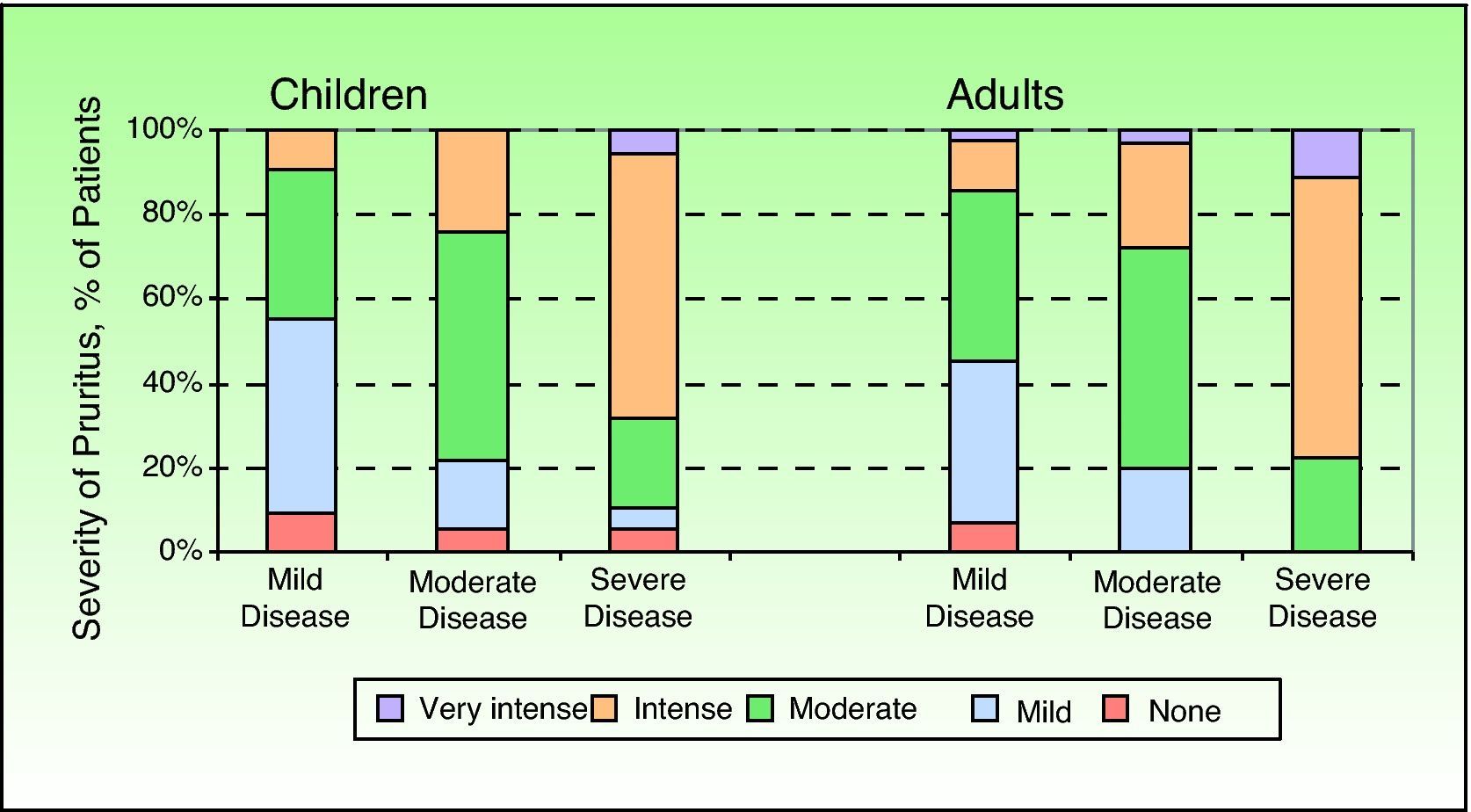
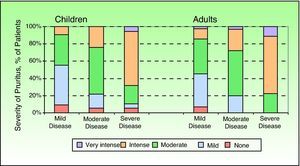
Question 4 of the ISS deals with the intensity of pruritus in its normal, minimal, or maximum state, and Figure 3 shows the results according to disease severity.
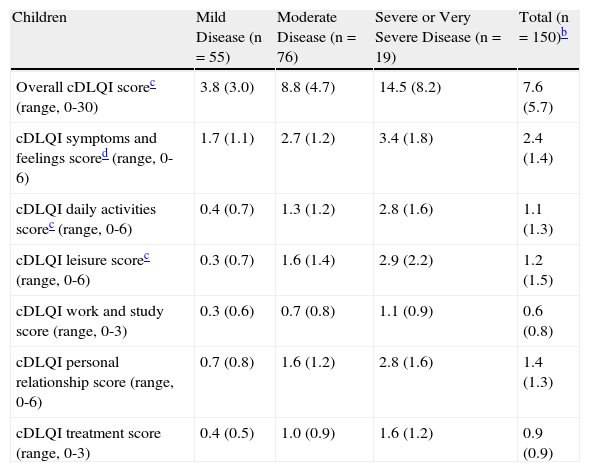
Table 4 shows the total and section scores obtained by patients on the DLQI or the cDLQI. Significant differences according to disease severity were observed in both the pediatric and the adult group for the total score and for the symptoms and feelings, daily activity, and leisure sections. On analyzing the different section scores of the DLQI, it was seen that patients scored highest in the section of symptoms and perceptions, indicating that this aspect of their lives was most affected by AD.
Overall Score and Section Scores on the Dermatology Life Quality Index in Children and Adults With Atopic Dermatitis According to Investigator's Overall Assessment of Disease Severity.a
| Children | Mild Disease (n=55) | Moderate Disease (n=76) | Severe or Very Severe Disease (n=19) | Total (n=150)b |
| Overall cDLQI scorec (range, 0-30) | 3.8 (3.0) | 8.8 (4.7) | 14.5 (8.2) | 7.6 (5.7) |
| cDLQI symptoms and feelings scored (range, 0-6) | 1.7 (1.1) | 2.7 (1.2) | 3.4 (1.8) | 2.4 (1.4) |
| cDLQI daily activities scorec (range, 0-6) | 0.4 (0.7) | 1.3 (1.2) | 2.8 (1.6) | 1.1 (1.3) |
| cDLQI leisure scorec (range, 0-6) | 0.3 (0.7) | 1.6 (1.4) | 2.9 (2.2) | 1.2 (1.5) |
| cDLQI work and study score (range, 0-3) | 0.3 (0.6) | 0.7 (0.8) | 1.1 (0.9) | 0.6 (0.8) |
| cDLQI personal relationship score (range, 0-6) | 0.7 (0.8) | 1.6 (1.2) | 2.8 (1.6) | 1.4 (1.3) |
| cDLQI treatment score (range, 0-3) | 0.4 (0.5) | 1.0 (0.9) | 1.6 (1.2) | 0.9 (0.9) |
| Adults | Mild Disease (n=42) | Moderate Disease (n=103) | Severe or Very Severe Disease (n=27) | Total (n=172) |
| Overall DLQI scorec (range, 0-30) | 5.5 (5.3) | 7.5 (4.8) | 12.0 (5.0) | 7.8 (5.3) |
| DLQI symptoms and feelings scored (range, 0-6) | 2.0 (1.1) | 2.7 (1.2) | 3.6 (1.0) | 2.7 (1.3) |
| DLQI daily activities scorec (range, 0-6) | 1.3 (1.4) | 1.5 (1.2) | 2.4 (1.5) | 1.6 (1.4) |
| DLQI leisure scorec (range, 0-6) | 0.9 (1.5) | 1.0 (1.2) | 2.2 (1.6) | 1.2 (1.4) |
| DLQI work and study score (range, 0-3) | 0.5 (0.9) | 0.8 (1.1) | 1.2 (1.1) | 0.8 (1.1) |
| cDLQI personal relationship score (range, 0-6) | 0.4 (0.9) | 0.7 (1.1) | 1.2 (1.1) | 0.7 (1.1) |
| DLQI treatment score (range, 0-3) | 0.5 (0.8) | 0.8 (0.8) | 1.4 (1.0) | 0.8 (0.9) |
a Results are shown as mean (SD).
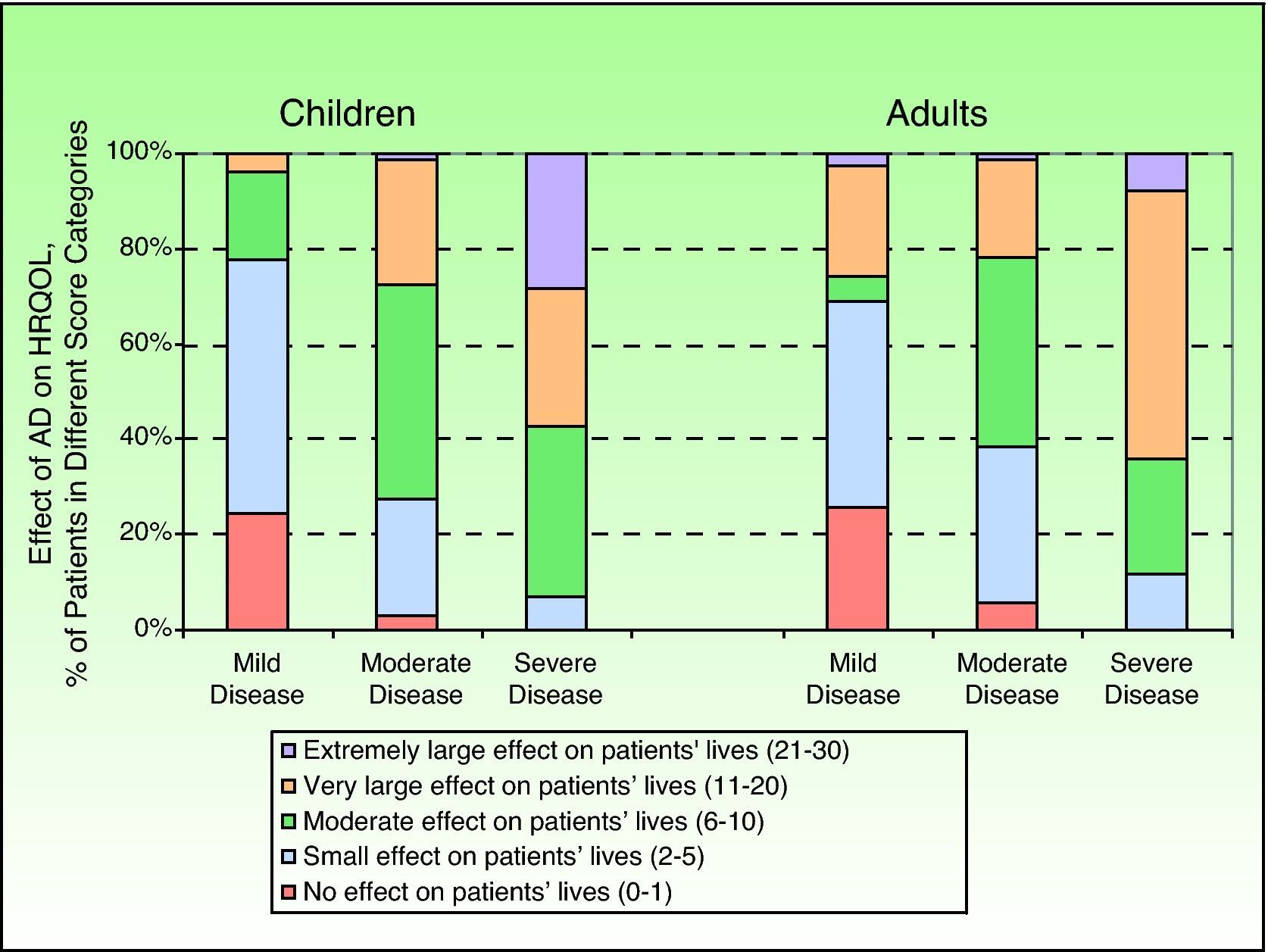
On analyzing the cDLQI scores by section, it was seen that AD had no effect on the lives of 10.6% of children, a small effect in 33.3%, a moderate effect in 34.1%, a very large effect in 18.2%, and an extremely large effect in 3.8%. In adults, it had no effect in 9.7% of patients, a small effect in 32.3%, a moderate effect in 28.4%, a very large effect in 27.1%, and an extremely large effect in 2.6%. As can be seen in Figure 4, which shows how AD affects patients’ lives according to disease severity, AD has a significantly larger effect on the lives of both children and adults with more severe disease (P<.05).
The presence and intensity of pruritus was very closely related to HRQOL, with a high Pearson correlation coefficient between overall ISS score and overall DLQI score, both in the case of children (0.69) and adults (0.72). There was also a correlation between ISS score and IGA score: 0.25 in adults (P<.001) and 0.23 in children (P<.001).
DiscussionAD had a clear effect on the HRQOL of the patients in our study, with over 50% of those with moderate or severe disease reporting that their disease had a very large or an extremely large effect on their lives. The fact that AD has a marked impact on HRQOL has been shown in previous studies, which have reported worse HRQOL in AD patients than in patients with other chronic skin disorders, such as psoriasis.19 The greater impact seen in patients with more severe disease is also consistent with findings of previous studies, which have shown a positive, statistically significant correlation between AD severity and DLQI scores.19
Both pruritus (evaluated by the ISS) and HRQOL worsened with increasing disease severity. It is noteworthy that while pruritus intensity (ISS score) correlated significantly with disease severity (mEASI) and HRQOL (cDLQI or DLQI) in both children and adults,14 the correlation was higher with HRQOL than with disease severity (moderate correlation). This is, however, to be expected as, like HRQOL, pruritus (the main symptom of AD) is self-rated by patients. Greater pruritus frequency and intensity was associated with worse HRQOL in both pediatric and adult patients. In fact, chronic pruritus has been reported to be inversely related to HRQOL, in a manner similar to that seen with chronic pain.20 It is therefore important to assess the degree of pruritus experienced by patients with AD when implementing therapeutic strategies aimed at improving HRQOL.
Carers of children with AD have reported that a high percentage of these children (79.9%) experience mood swings. AD has also been seen to cause more sleep disorders in children with AD than in healthy children.21 Moore et al.22 observed that sleep loss in patients with AD was closely correlated with the frequency and intensity of pruritus. Sleep disorders in AD are an important factor and contributor to decreased overall HRQOL as insufficient sleep results in increased sleepiness during the day, mood swings, poor performance at school and work, and problems with social functioning.23 Sleep disorders have an impact on all domains of the DLQI (symptoms and feelings, daily activities, leisure, study and work, and personal relationships. This is consistent with observations in patients with eczema caused by allergy to house dust mites.24 Sleep disorders are one of the most widely studied causes of decreased HRQOL in patients with AD.25,26 Furthermore, a lack of sleep affects not only the patients themselves but also their families,27 who may experience mental health problems such as anxiety and depression.22 In Spain, no studies to date have specifically analyzed the effect of AD on the HRQOL of children or indeed adults and their relatives.
Based on ISS scores, pruritus severity was slightly lower in children than in adults in our series. On analyzing the results by disease severity according to the IGA, the differences were slightly greater in the adult group than in the children's group. This is possibly because in the latter case, the questionnaire was completed by the children's parents or guardians. Although the correlation between ISS and IGA scores was weak in both groups, it was significant, suggesting that the 2 variables are related.
AD also affects sexual function in adults, and particularly so in those with severe or very severe disease. While AD only had a slight impact on the personal relationships section of the DLQI (which includes questions on sexual function) in our series, sexual desire and sexual function were reported to be affected by 23.5% and 18.1% of adults, respectively. Misery et al.,28 observed that impairment of sex life in patients with AD was similar to that seen in other chronic skin disorders, and they also reported that AD had a considerable impact on mental health.
The fact that the ISS was completed by the children's parents or guardians in our series may have introduced bias regarding the intensity and characteristics of pruritus in the pediatric group, and it is possible that this bias was more pronounced in very young children, in whom it is more difficult to assess these aspects. Nonetheless, nobody is in a better position to do so than the children's patients or guardians.
ConclusionsIn our series, pruritus frequency and severity, as measured by the ISS, increased with disease severity according to the IGA. AD caused sleep disorders in 2 of every 3 children and in 3 of every 4 adults. It also affected HRQOL in both children and adults and was strongly correlated with the presence and intensity of pruritus.
FundingThis study was funded by Astellas Pharma S.A.
Conflicts of InterestDr J Sánchez Pérez is participating or has participated in clinical trials with the following pharmaceutical companies: Abbott, Astellas, Biogen, Galderma, Pfizer, Shering-Plough, and Wyeth Pharmaceuticals.
Dr E Daudén has been an advisory board member, received grants and research support, participated in clinical trials, and received speaker's fees from the following pharmaceutical companies: Abbott, Astellas, Biogen, Centocor Ortho Biotech Inc., Galderma, Glaxo, Janssen-Cilag, Leo Pharma, Merck-Serono, Pfizer, Novartis, Schering-Plough, Stiefel, Wyeth Pharmaceuticals, 3M, and Celgene.
The authors would like to thank all the researchers who participated in the PSEDA study.
Please cite this article as: Sánchez-Pérez J, et al. Impacto de la calidad de vida relacionada con la salud en población pediátrica y adulta española con dermatitis atópica. Estudio PSEDA. Actas Dermosifiliogr.2013;104:44-52.

![Dermatitis Quality of Life Index Scores (DQLI) (effect of atopic dermatitis [AD] on health-related quality of life [HRQOL]) shown by percentage of children and adults and classified by the investigator Dermatitis Quality of Life Index Scores (DQLI) (effect of atopic dermatitis [AD] on health-related quality of life [HRQOL]) shown by percentage of children and adults and classified by the investigator](https://static.elsevier.es/multimedia/15782190/0000010400000001/v1_201304241547/S1578219012003563/v1_201304241547/en/main.assets/thumbnail/gr4.jpeg?xkr=ue/ImdikoIMrsJoerZ+w9/t1/zx4Q/XH5Tma1a/6fSs=)



