The patient was a 36-year-old woman diagnosed with rheumatoid arthritis in 2008 and on treatment with chloroquine 250 mg/d and oral prednisone 5 mg/d since April 2008. In October 2009 the daily dose of chloroquine was increased to 500mg due to poor control of the symptoms of the underlying disease. The patient came to the outpatient clinic for hypopigmentation of the eyelashes present since February 2010.
Physical ExaminationThe patient had chestnut hair and skin phototype II but presented white eyelashes on the upper and lower eyelids of both eyes (Fig. 1). No hypopigmentation of the scalp hair was observed due to the use of hair dye, or of terminal hair on other parts of the body at the time of examination. Examination of the remaining skin surface revealed no associated hypopigmented macules.
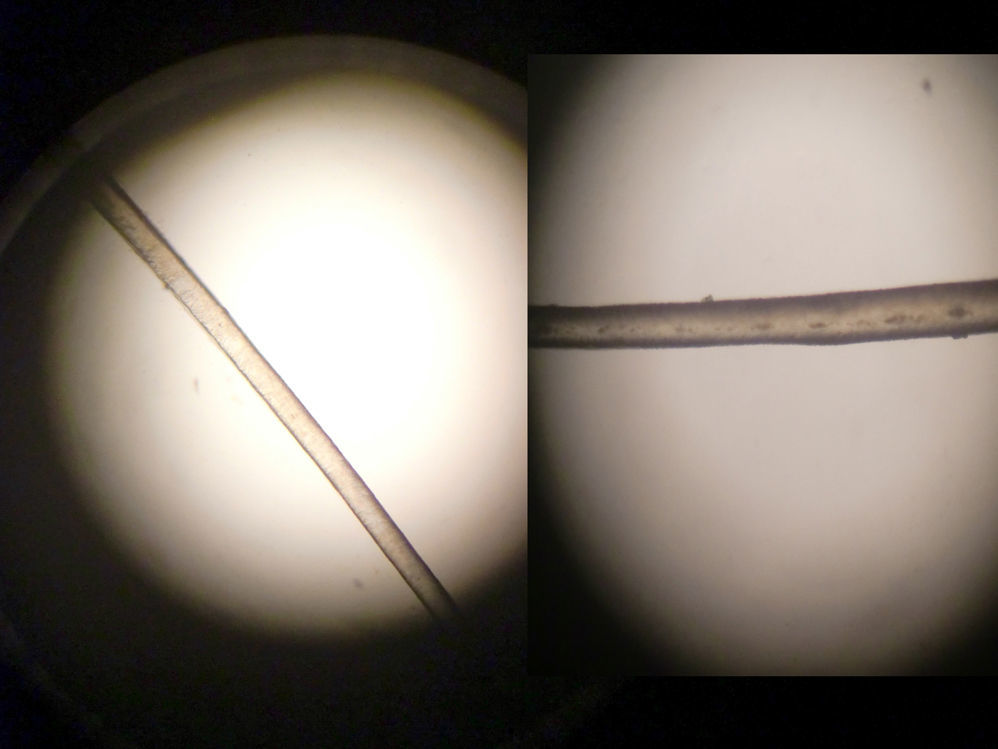
Additional TestsLight microscope examination of the hair showed an almost complete absence of melanin granules. Depigmentation affected the entire length of some eyelashes and only the distal portion of others, with a progressive increase in the number of granules to almost normal levels in the proximal portions (Fig. 2).
The blood count, biochemistry, and autoimmunity studies showed results typical of the underlying rheumatoid arthritis.
What Is Your Diagnosis?
DiagnosisChloroquine-induced depigmentation.
Clinical Course and TreatmentClinical suspicion of hypopigmentation due to the use of high doses of chloroquine prompted a change in treatment to leflunomide 10 mg/d with the prednisone maintained at the previous dosage.
CommentChloroquine induced hypopigmentation was first described in 19481 but only 50 new cases have been published since.2 In most of those cases the patients had received high doses of chloroquine (between 300 and 400 mg/d) and presented hypopigmentation with a preference for the eyebrows, eyelashes, moustache, and body hair.3 Hypopigmentation was more common in patients with light hair than dark hair.4
Most of the published cases show that depigmentation is reversible on interruption of treatment with chloroquine, dose reduction, or even substitution of chloroquine by hydroxychloroquine.3,5
The mechanism of action of chloroquine-induced depigmentation is not fully understood. Chloroquine-melanin interaction allows us to suggest that this drug may interfere with melanogenesis.6 The condition shows a preference for tissues rich in melanin, which is found in highest concentrations in the skin and eyes. In chloroquine-induced retinopathy there is irreversible fixation of the drug to the pigmentary epithelium, but the process is reversible over time in the skin as the chloroquine deposited in the melanocytes transfers to the keratinocytes and is later eliminated by desquamation.3 As the drug builds up in pigmented epithelia, the accumulation of melanin in the melanosomes in the prolongations of the hair bulb is partially or completely inhibited. This indicates that chloroquine exerts a toxic effect on melanocytes that blocks melanin production.3
Several authors have shown that chloroquine has a tendency to accumulate in the skin and that the amount of the drug detected is directly proportional to the dose administered and the duration of treatment. Depigmentation of fair or red hair is far more common than that of darker hair, suggesting the possibility of a greater interaction between chloroquine and pheomelanin than between chloroquine and eumelanin.4,6
In conclusion, chloroquine-induced hypopigmentation is similar to vitiligo, and although it is a rare collateral effect it represents one end of the spectrum of chloroquine-induced pigmentary disorders.
Please cite this article as: Gómez-Vázquez M, et al. Hipopigmentación de las pestañas. Actas Dermosifiliogr.2011;102:463-464.