This is the case of a Caucasian woman in her 3rd decade of life, with a past medical history of atopic dermatitis, who presented with a several-year history of pruritic lesions on her legs and arms that had become increasingly symptomatic over time.
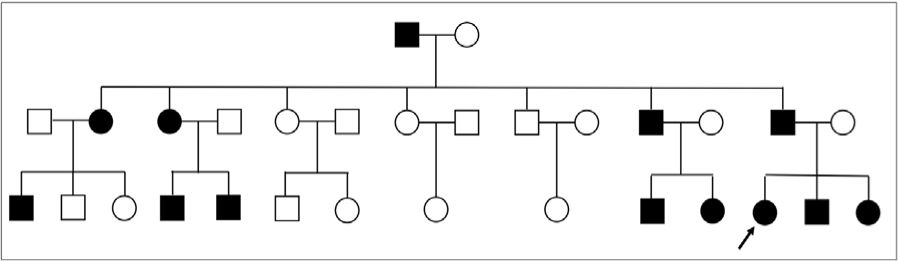
Her paternal uncle—who had skin lesions too—had been diagnosed with lichen, but our patient could not specify the exact type. In addition, another 11 1st- and 2nd-degree relatives from her paternal side of the family exhibited skin lesions similar to hers (figure 1: family tree showing affected relatives with black symbols, including our patient [proband]).
Physical examinationHyperkeratotic brownish papules with surface shine were observed on the legs, mainly on the pretibial areas rather than the thighs, with follicular hyperkeratosis and hypopigmented areas of reticular appearance (figure 2: clinical image). Only xerosis was observed on the arms.
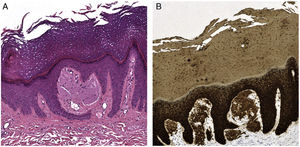
HistopathologyA punch biopsy of the patient's left leg revealed the presence of a vaguely verruciform epidermal papillomatous hyperplasia, with thick compact hyperkeratosis along with focal parakeratosis. Additionally, weakly eosinophilic globular deposits were observed in the dermal papillae (figure 3a: H-E ×15), which tested positive for Congo red and CK34betaE12 on immunohistochemical study (figure 3b: IHQ CK34betaE12 ×15).
What is your diagnosis?
DiagnosisFamilial lichen amyloidosis.
Course of the disease and treatmentTreatment with 0.1% tacrolimus ointment proved ineffective; although NBUVB phototherapy was initiated it did not eliminate the itching. Acitretin was not considered because of the patient's reproductive desires.
CommentaryThe most common forms of primary localized cutaneous amyloidosis are macular amyloidosis and lichen amyloidosis. The latter often affects individuals from South America, the Middle East, and Asia; in Europe it is not that common.1 Most cases are sporadic, but up to 10% are familial cases of autosomal dominant inheritance with variable penetrance.1-3 In some families, mutations have been identified in the OSMR gene encoding the oncostatin M receptor beta (OSMRβ), a component of 2 different cytokines: the OSM type II receptor and the IL-31 receptor.1-3 This mutation prevents signal transduction inside the cells after OSM or IL-31 stimulation at these extracellular receptors. However, how this signaling cascade failure triggers itching is still unknown; keratinocytes, cutaneous nociceptive nerves, and specific neurons in the dorsal root ganglion are directly involved in physiopathogenesis, suggesting that this disease could be classified as neurodermatitis.1,2 In other families, this type of mutation has not been found, suggesting that this disease is genetically heterogeneous.1,2 We did not find similar cases published in Spain. No genetic studies have been conducted either of sporadic cases of lichen amyloidosis attributed to repeated skin friction.2
Sporadically and probably coincidentally, associations of lichen amyloidosis with several entities have been described.2,4 The presence of a single plaque of lichen amyloidosis in the scapular or interscapular region should raise suspicion of a secondary etiology of amyloid deposition, as it has been reported in up to 35% of the patients with multiple endocrine neoplasia type 2A and may precede the development of medullary thyroid carcinoma by several years, making it an early marker of mutation in the RET gene.2,5 This genetic mutation does not seem to be related to primary localized cutaneous amyloidosis, even in familial cases.2,3,6
Treatment of familial lichen amyloidosis is similar to the sporadic form and includes topical corticosteroids, vitamin D derivatives, and tacrolimus, phototherapy, acitretin, and lasers (Nd:YAG and pulsed dye), although results are often unsatisfactory.2-4 Two cases treated with amitriptyline have been reported, with significant improvement in itching but not in skin lesions.7 Dupilumab has proven successful, with symptomatic and clinical improvement, in a case of generalized primary lichen amyloidosis and another case associated with atopic dermatitis, and could be considered a novel therapeutic option.8,9 Probably, improved genetic and pathophysiological understanding of this disease will lead to the development of new, more specific therapies in the future.2
Conflicts of interestNone declared.