The late development of symmetrical, ascending telangiectasias over an extensive area of the skin with no associated systemic manifestations is a common presentation of generalized essential telangiectasia (GET). It was recently suggested that cutaneous collagenous vasculopathy (CCV) is clinically identical to GET but that the 2 conditions can be distinguished by their distinctive histopathologic findings. We present 2 patients, both women, with multiple telangiectasias and describe the histopathologic findings that led to the diagnoses of GET and CCV. Dermoscopic findings in both cases were similar, except that the older telangiectasias in the patient with CCV were violaceous and distributed in a tortuous, serpentine pattern. During follow-up 12 years for the woman with GET and 42 years for the woman with CCV we saw that in GET the lesions remained stable in appearance whereas in CCV there was progressive darkening and morphological changes eventually resulting in superficial varicose veins.
La aparición tardía de telangiectasias cutáneas extensas de forma simétrica y ascendente, sin manifestación sistémica asociada, constituye la forma de presentación típica de la telangiectasia esencial generalizada (TEG). Estudios recientes sugieren que la vasculopatía colágena cutánea (VCC) tiene una presentación clínica idéntica pero los hallazgos histopatológicos son distintivos y permiten diferenciarla de la TEG. Presentamos 2 pacientes con múltiples telangiectasias cutáneas con hallazgos histopatológicos diagnósticos de TEG y de VCC. La dermatoscopia de las telangiectasias en ambos casos fue similar, excepto en las lesiones más antiguas de VCC que presentaba vasos de color violáceo y con una morfología tortuosa en serpentina. Durante el seguimiento de ambas pacientes de 12 y 42 años (TEG y VCC, respectivamente) hemos comprobado que en la TEG las telangiectasias mantienen su aspecto inicial mientras que en la VCC se observó un oscurecimiento progresivo de las lesiones y cambios en la morfología resultando en varicosidades superficiales.
The International Society for the Study of Vascular Anomalies classifies telangiectasias as a type of capillary malformation that includes hereditary hemorrhagic telangiectasia and other entities.1 Several conditions are associated with primary telangiectasia, as follows: (a) generalized essential telangiectasia (GET); (b) cutaneous collagenous vasculopathy (CCV); (c) hereditary hemorrhagic telangiectasia; (d) hereditary benign telangiectasia; (e) ataxia-telangiectasia; (f) unilateral nevoid telangiectasia; and (g) angioma serpiginosum.2,3
GET is an unusual clinical entity, with no known causes and no association with other pathologic signs. It mainly affects middle-aged women and is characterized by telangiectasias that usually appear on the lower limbs before ascending gradually and symmetrically. The telangiectasias can reach the trunk and upper limbs.4 Although infrequent, involvement of the conjunctiva and oral mucosa has been reported.5 In CCV, telangiectasias also start on the lower limbs before progressing identically to GET and can eventually affect most of the skin surface.6 However, the histologic and ultrastructural findings for both entities are different. In CCV, we find dilated vessels in the superficial dermis with wall thickening due to collagen deposition and reduplication of the basement membrane, which is observed in immunohistochemistry with antibodies against collagen IV, fibronectin, and laminin.7
We present 2 cases of multiple cutaneous telangiectasias observed during physical examination with no involvement of the mucosa or nail bed. No family history of similar lesions or personal or family history of bleeding was reported in either case.
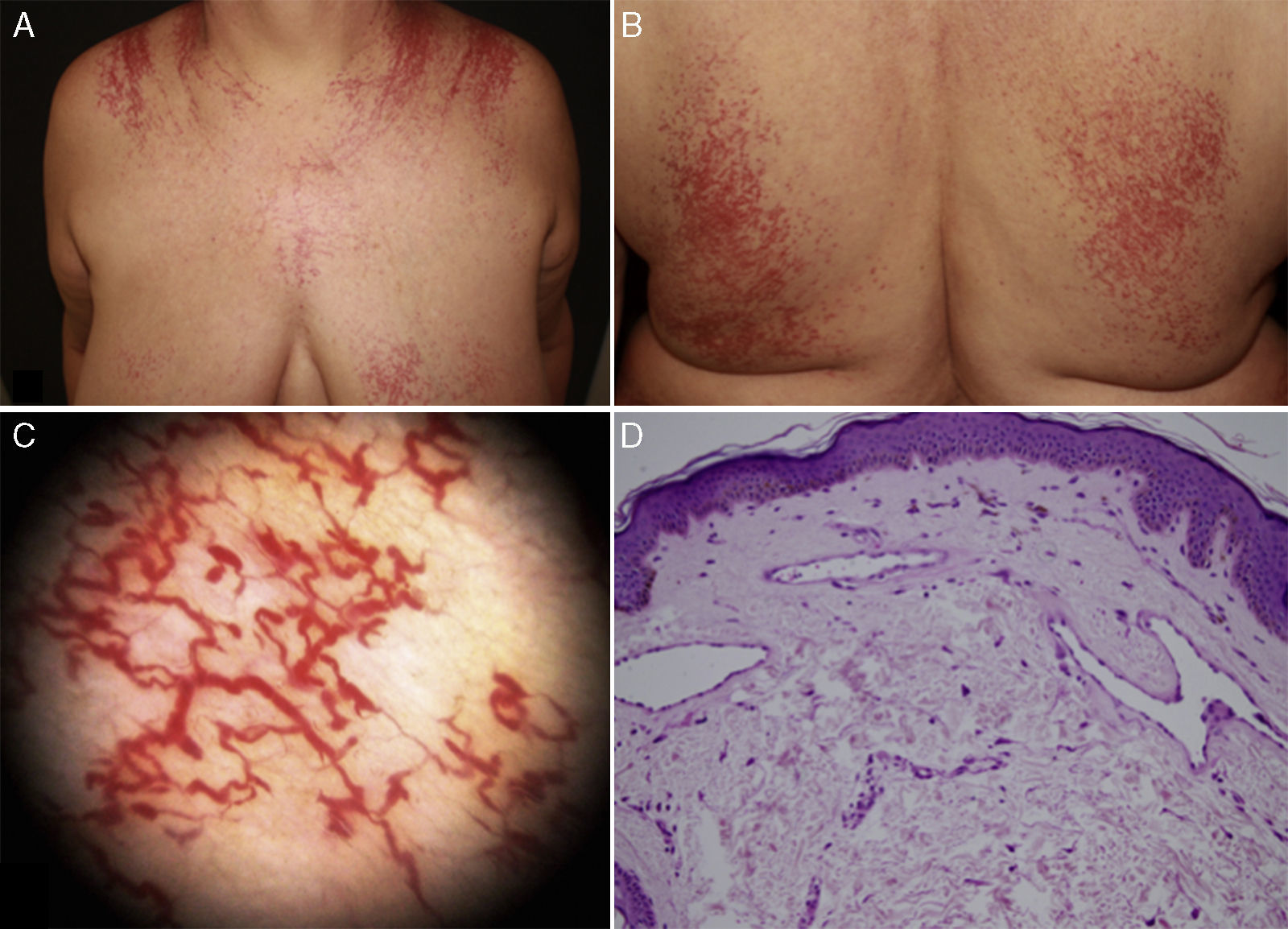
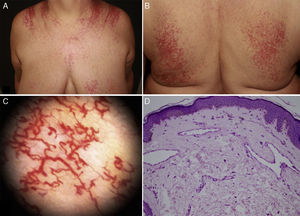
Case DescriptionPatient 1. The patient was a 62-year-old woman with a history of arterial hypertension and hypothyroidism under treatment with olmesartan and levothyroxine. During the previous 12 years she had presented multiple telangiectasias that extended symmetrically on the upper part of the trunk, chest, back, and both upper limbs (Fig. 1A and B). Dermoscopy revealed fine arborizing vascular dilations (fig. 1C). The patient reported intense pruritus that worsened with heat and stress. The additional tests performed included a complete blood count, biochemistry, serum tryptase, protein profile, antinuclear antibody staining, anti–extractable nuclear antigen antibody screening, rheumatoid factor test, complement test, and serology testing for human immunodeficiency virus, hepatitis C virus, hepatitis B virus, and syphilis. The results were normal. Histology of 2 biopsy specimens revealed telangiectasias, most of which were fine-walled with flattened endothelial cells and located mainly in the superficial dermis. There was no cellular atypia (Fig. 1D). Giemsa staining revealed <6 mastocytes/HPF. Histology findings were compatible with a clinical suspicion of GET.
Clinical presentation and dermoscopy and histology findings for Patient 1 (generalized essential telangiectasia). A and B, Multiple telangiectasias distributed symmetrically on the chest and back. C, Dermoscopy reveals arborizing vascular dilations. D, Histology reveals fine-walled telangiectatic vessels with flattened endothelial cells in the superficial dermis.
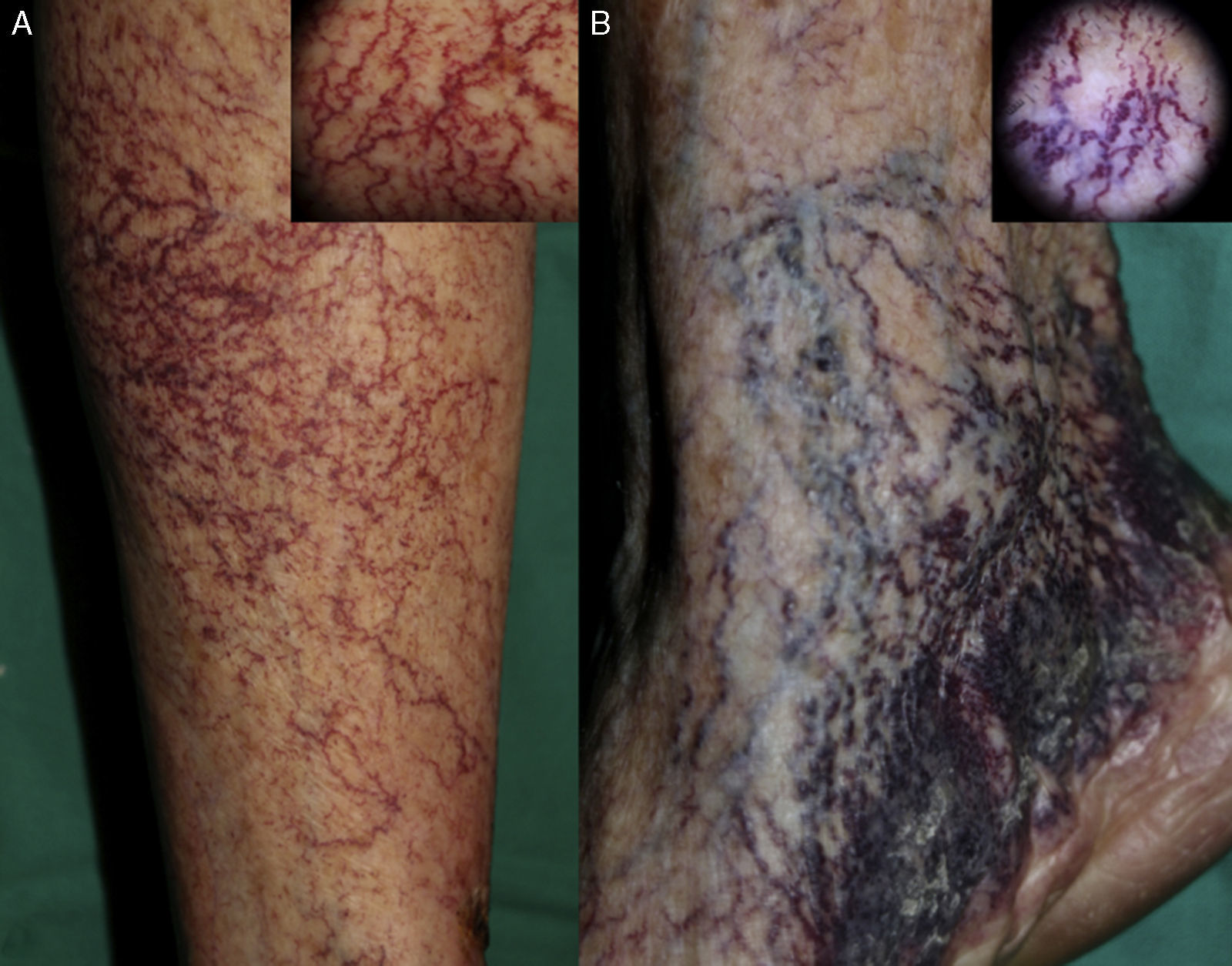
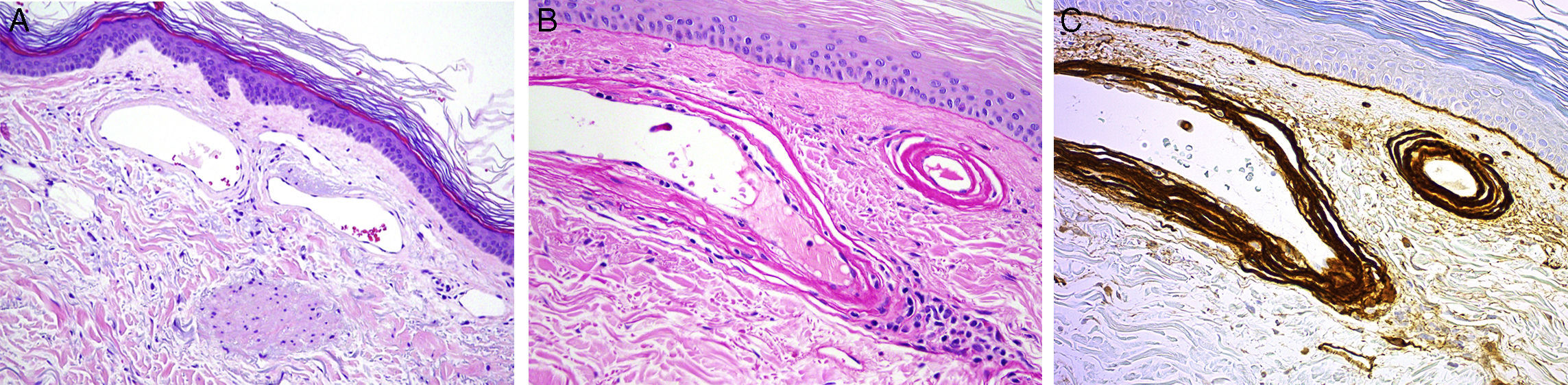
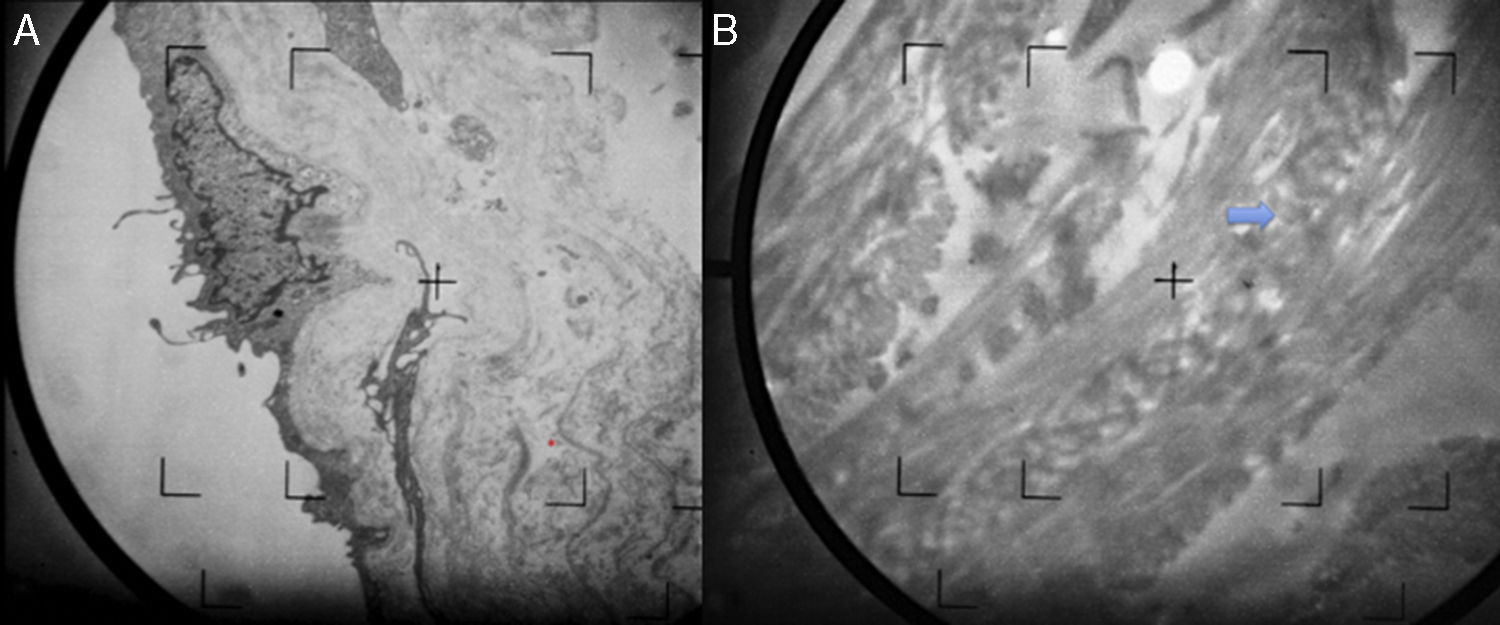
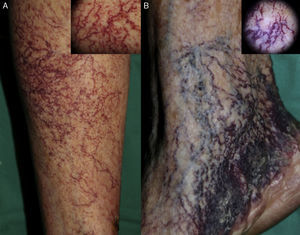
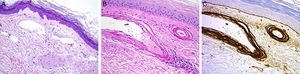
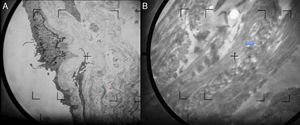
Patient 2. The patient was a 92-year-old woman with hypertension under treatment with chlortalidone/spironolactone who began to develop telangiectasias on both lower limbs at the age of 50 years (Fig. 2). The lesions were asymptomatic and gradually descended to the dorsum of the feet and soles. The telangiectasias were initially red in color (Fig. 3A) but became darker over time until they took on a violaceous tone, leaving hyperkeratotic lesions and microvarices (Fig. 3B). Dermoscopy of the oldest lesions revealed vascular dilations with a tortuous, serpentine pattern (Fig. 3B inset). The results of additional tests (complete blood count, coagulation tests, biochemistry, and screening for antinuclear antibody, anti–extractable nuclear antigen antibody, rheumatoid factor, hepatitis C virus, and cryoglobulins) were normal. Two skin biopsy samples were taken for routine histology, and another specimen was taken for electron microscopy. Histology of the red telangiectasias (proximal third of the leg) revealed dilated vessels in the papillary dermis with slight wall thickening. The vessels were surrounded by an amorphous eosinophilic material that stained with Masson trichrome and periodic acid–Schiff (PAS) diastase. Immunohistochemistry was positive for collagen IV, with reduplication of the basement membrane in the form of concentric layers (Fig. 4). Electron microscopy revealed reduplication and focal disruption of the basement membrane accompanied by deposition of collagen fibers with an anomalous pattern (Fig. 5). These histopathology findings are diagnostic of CCV.
Histology study for Patient 2 (cutaneous collagenous vasculopathy). A, Vessels with slightly thickened walls in the upper dermis (hematoxylin-eosin, original magnification, ×20). B, Perivascular deposition of material that stained with periodic acid–Schiff diastase (×40). C, Immunohistochemistry revealed strongly positive results for collagen IV, thus indicating reduplication of the basement membrane (×40).
The appearance of multiple symmetrical cutaneous telangiectasias on the lower limbs that subsequently extend to the rest of the body with no involvement of the mucosa or nail bed is very suggestive of GET.4,5 However, the clinical presentation considered characteristic of GET is also thought to be characteristic of CCV,6 a microangiopathy affecting the postcapillary venules that was first described in 2000. The histology findings of CCV are distinctive and diagnostic: the blood vessels of the superficial vascular plexus of the dermis are dilated, with wall thickening due to abundant deposition of collagen, which is highlighted with PAS, PAS diastase, and Masson trichrome; in addition, immunohistochemistry with collagen IV antibody reveals reduplication of the basement membrane. In a recent review of this entity, Salama et al.6 found that it affected middle-aged and elderly men and women (42-85 years) who were polymedicated and had comorbid conditions. The authors stress that the clinical presentation was indistinguishable from that of GET in most patients and that, in fact, this was the diagnosis in most cases.
In patient 2 (diagnosed with CCV), dermoscopy of the most recent telangiectasias revealed linear branching red vessels (Fig. 3A); dermoscopy of the oldest lesions, on the other hand, revealed violaceous vessels that were distributed in a tortuous, serpentine pattern (Fig. 3B). Bardazzi et al.8 recently reported a case of CCV in which the dermoscopy findings were similar to those we observed in patient 2. Furthermore, dermoscopy of the most recent lesions in this patient, ie, those on the trunk, revealed branching red vessels that were consistent with the dermoscopy findings for patient 1 (diagnosed with GET). In our opinion, dermoscopy cannot differentiate early between both entities. In addition, dermoscopy findings could be affected by the location of the telangiectasias.
CCV could be underdiagnosed, as only 28 cases have been reported.9–11 Its etiology and pathogenesis remain unknown and, to date, no associations have been found with systemic, vascular, or drug-related disorders. It has been postulated that chronic repeated endothelial damage in the microvasculature triggers a repair mechanism that is responsible for the histology findings observed.12,13
The most effective treatment for both entities is pulsed dye laser, which is indicated for resolution of symptoms or for cosmetic reasons.14,15 Both patients were offered laser therapy, although it was eventually decided not to administer treatment owing to the absence of symptoms and cosmetic effects.
We present clinical, dermoscopy, and histopathology findings for 2 women with extensive acquired telangiectasia that indicated a diagnosis of GET and CCV. We stress the importance of taking biopsy samples of the more extensive telangiectasias when attempting to reach a diagnosis and in order to increase our knowledge of CCV. The cases of CCV we report, in which follow-up was longer than 40 years, is especially interesting, since the changes can be seen over time, namely, darkening of the telangiectasias, development of microvarices, and hyperkeratosis, none of which are seen in long-standing GET.
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purposes of this study.
Confidentiality of dataThe authors declare that they have followed their institutional protocols on publication of patient data.
Right to privacy and informed consentThe authors declare that no private patient data appear in this article. The corresponding author holds the informed consent documents.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Knöpfel N, Martín-Santiago A, Saus C, Escudero-Góngora MM, del Pozo LJ, Gómez C. Telangiectasias extensas adquiridas: comparación entre telangiectasia esencial generalizada y vasculopatía colágena cutánea. Actas Dermosifiliogr. 2017;108:e21–e26.