A 48-year-old man with no relevant past medical history was examined during regular follow-up in the digital dermoscopy clinic. He exhibited a light brown macule on his right shoulder—measuring 1cm2 in diameter—without evident changes at the follow-up with digital dermoscopy body mapping (Fig. 112). The patient reported having undergone laser hair removal sessions up to 1 year and a half prior to the consultation.
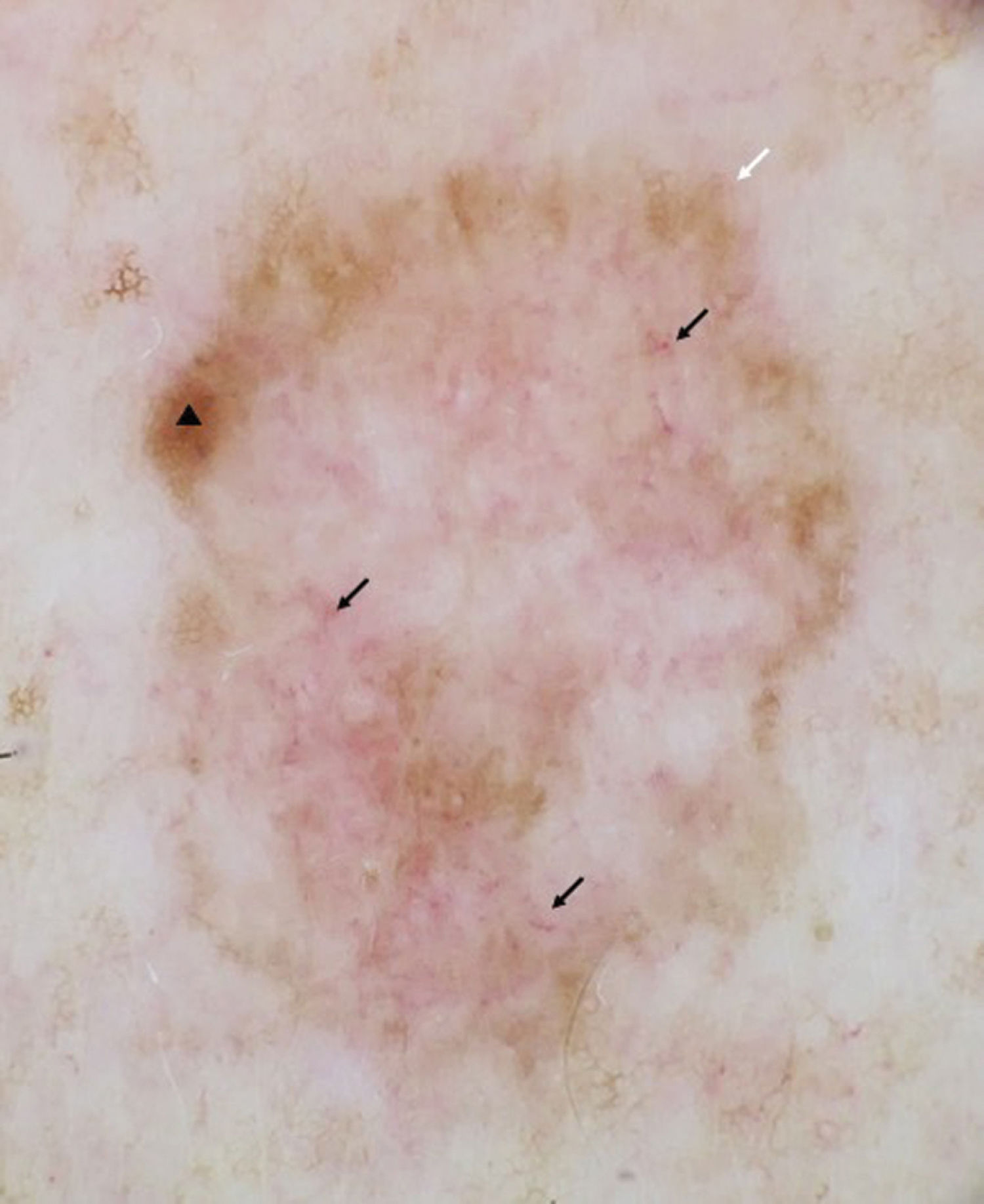
Presentation of the 2 images followed by this question: what is your diagnosis?Dermoscopy only showed blurred central areas with atypical vascularization and a typical fine reticular pattern at the periphery (Fig. 2). What is your diagnosis?
CommentaryConfocal microscopy of the lesion revealed the presence of epidermis with abundant dendritic cells and a disorganized dermoepidermal junction where atypical cells were also seen (Fig. 3). Lesion was excised with the histological diagnosis of extrafacial lentigo maligna (LME).
LMEs are lentiginous-pattern melanomas associated with chronic sun damage whose incidence has been on the rise.1–3 A model of clinical progression and dermoscopic representation of these lesions has been described.2,4 The first event is disruption of the reticular pattern, followed by the appearance of blurred areas with surrounding pigment dots and triangular structures, progressing to angled and “zigzag” lines. Finally, the lesion progresses into an almost complete erasure, showing only central atypical vascularization and short white lines.2,4
The greatest diagnostic difficulty occurs in incipient lesions, which retain many areas of typical reticular pattern with minimal reticular distortion, and in more advanced cases, showing an almost complete loss of the reticular pattern, with a preserved peripheral reticular pattern. Back in 2022, we described a case of LME very similar to this one, with the entire lesion almost completely blurred under dermoscopy, with short white lines, atypical vascularization, and a preserved peripheral reticular pattern.5 Lentigo maligna (Figure 2) did not exhibit central white lines, only atypical vascularization and a peripheral reticular pattern which confirmed the melanocytic origin of the lesion.
Early detection of lentigo maligna is crucial to prevent its progression to invasive melanoma.6 Since cases have been reported with very subtle features, we recommend paying special attention to lesions with remnants of a pigmented reticular pattern and central atypical vascularization, with or without short white lines inside.