Erythema papulosa semicircularis recidivans (EPSR) is a recently described entity characterized by the appearance of semicircular erythematous plaques with a centrifugal extension and of a clearly seasonal nature, starting in spring or summer and resolving spontaneously in colder seasons.1 The principal differential diagnosis is established with figurate erythema,2 especially erythema annulare centrifugum (EAC) and, specifically, its annually recurring subtype (AR EAC).3 We report the case of a patient with recurring annular lesions that oblige us to consider the differential diagnosis between these 2 entities.
A 70-year-old woman with a history of ischemic heart disease, hypothyroidism, thromboembolic disease, and chronic gastritis visited our department in the month of May with a large erythematous plaque in the abdominal region that had appeared 2 weeks earlier and had expanded centrifugally (Fig. 1). The patient stated that the lesion caused pruritus and moderate pain. She had no fever, joint pain, or any other symptoms. In total, the patient had had 6 independent episodes of lesions in a similar location and of similar clinical characteristics. The first episode had occurred 9 years earlier (Fig. 2). All the episodes had begun in the spring or summer months and had resolved spontaneously in the early autumn.
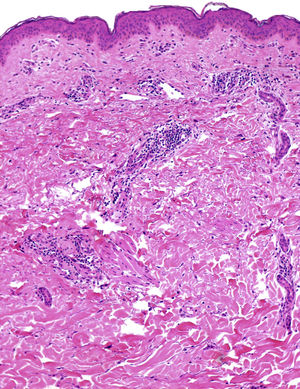
Physical examination revealed a semicircular erythematous plaque measuring 20×15cm, located on the abdomen, with a clearly demarcated papular margin and central lightening (Fig. 1). Histology showed only a perivascular inflammatory infiltrate composed mainly of lymphocytes, which involved the superficial and middle dermis. The epidermis and deep dermis showed no abnormalities (Fig. 3). Blood tests were performed with a full blood count and biochemistry, and an antibody titer was performed; results were normal.
Treatment with topical methylprednisolone and oral prednisone was prescribed (maximum dosage, 0.5mg/kg/d) for 15 days, with no clinical response. After the summer, the patient presented for a follow-up visit and showed complete spontaneous resolution of the lesions. The course of the previous episodes was similar.
EPSR was first described in 2012, when Song et al1 reported a series of 9 patients of Chinese nationality with papuloerythematous eruptions with a centrifugal growth pattern that typically recurred during the warm, humid months. Cases with similar seasonality were subsequently described in Western countries, one of which showed a possible link to a primary pancreas B cell lymphoma.4,5 The most frequently involved areas are the torso and proximal extremities; the face, palms and soles are not usually involved. Histology usually shows a perivascular lymphocytic inflammatory infiltrate and mild edema of the papillary dermis; all of these finding suggest superficial perivascular dermatitis. No leukocytoclasia or other vasculitic findings are observed.1
As mentioned, the principal differential diagnosis is with EAC. Both EAC and EPSR begin as plaques with centrifugal growth and central lightening. Desquamation at the edge of the lesion can be observed in the superficial form of EAC, whereas this phenomenon is not seen in EPSR. Moreover, the size of the plaques tends to be smaller in EAC than in EPSR. Histology of EAC is characterized by the distribution of the perivascular inflammatory infiltrate in a shirt-sleeve pattern; this pattern is not so clearly observed in EPSR.
Although EAC does not usually present as clearly seasonal, descriptions exist of cases in which, just like in EPSR, the lesions appear in the warm months and resolve spontaneously with the arrival of cold temperatures. This subtype is known as annually recurring EAC.3 Although the etiology of EPSR and EAC is unknown, both may be due to a hypersensitive reaction to different external or internal stimuli. Infectious diseases, hormone abnormalities or fluctuations, some drugs and foods, and even neoplasias have been linked to EAC lesions. Annually recurring EAC may also involve seasonal environmental factors such as increased temperature or insect bites. A clear causal agent, however, cannot be identified in most cases (idiopathic EAC).
With regard to treatment, topical and systemic corticosteroids may alleviate the pruritus, but they cannot halt the progress of the lesions, which may involve the entire chest, back or neck. Characteristic of EPSR and annually recurring EAC is the gradual and spontaneous regression of the lesions with the arrival of cooler seasons. Long-term follow-up has recorded recurrences in the first 2-5 years, with subsequent definitive resolution.1 Other publications, however, suggest a longer duration of the disease.5
Although EPSR has been described and subsequently reported in high-impact scientific journals, some authors question that it has sufficient clinical pathologic entity to be considered as an independent disease and they prefer to consider it as a peculiar variant of recurring figurate erythemas such as annually recurring EAC.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Bernia E, Requena C, Llombart B. Eritema papular semicircular recidivante: ¿nueva entidad o subtipo de eritema anular centrífugo? Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.04.012