Diagnosis of vibratory urticaria/angioedema is established after performing the vortex provocation test. There is current consensus on measuring the forearm perimeter after running such test to define a positive response to it.
Material and methodWe evaluated the frequency of prior symptoms following vibratory stimuli in volunteers using a questionnaire, response to the vortex provocation test in the same volunteers (increase in forearm perimeter, erythema, localized edema, heat, and pruritus), inter-rater reliability, and correlation between the scores obtained in the questionnaire and response to the test.
ResultsA total of 40 volunteers participated in this survey, 17 of whom were excluded due to dermographism. A total of 59% out of 123 without dermographism responded positively to ≥1 items of the questionnaire. Localized erythema, heat or localized edema were reported in 58.5%, 38.2%, and 32.5%, respectively. A total of 73.6% of volunteers presented with itch. The mean intensity of itch was 3.44, 95% CI, 2.94–3.94. Inter-rater agreement was low regarding the increase in forearm circumference at three levels (intraclass correlation coefficient, 0.477, 95% CI: 0.253–0.634; 0.496, 95% CI: 0.280–0.647; and 0.370, 95% CI: 0.100–0.559, respectively) and optimal regarding erythema, heat and localized edema (kappa index, 0.868; 0.756; and 0.757, respectively). A significant correlation was identified between the questionnaire score and the altered response to the test in its different variables.
ConclusionsWe propose the following variables: erythema; localized edema; heat; and the intensity/speed of onset/duration of pruritus to define a positive response to the vortex provocation test given their ease of execution and optimal inter-observer agreement.
En la urticaria o los angioedemas vibratorios se ha consensuado que la respuesta positiva a la prueba de provocación del vórtice se defina en función del aumento del perímetro del antebrazo.
Material y métodoSe evalúan la frecuencia de síntomas previos ante estímulos vibratorios mediante un cuestionario, la respuesta (aumento de perímetro del antebrazo, eritema, edema, calor y prurito) a la prueba de provocación del vórtice en una población de voluntarios sanos en 12 centros llevada cabo por 2 evaluadores independientes en cada centro, la fiabilidad interevaluador y la correlación entre síntomas previos y la reacción a la prueba de provocación.
ResultadosParticiparon 140 voluntarios; 17 se excluyeron por dermografismo. La prueba del vórtice desencadenó eritema, calor o urticaria o edema localizados en el 58,5, 38,2 y el 32,5%, de los casos, respectivamente. La concordancia entre evaluadores fue baja respecto del aumento del perímetro del antebrazo a 3 alturas, con un coeficiente de correlación intraclase (CCI) de 0,477 e IC 95%: 0,253-0,634; CCI de 0,496 e IC 95%: 0,280-0,647 y CCI de 0,370 e IC 95%: 0,100-0,559, respectivamente) y óptima respecto del eritema, el calor y el edema localizado (índice kappa: 0,868, 0,756 y 0,757, respectivamente). Se identificó una correlación significativa entre la puntuación del cuestionario y la respuesta a la pueba en sus distintas variables (eritema, calor o edema localizado).
ConclusionesProponemos que el eritema, la urticaria o el edema localizados y el calor sustituyan a la variable de aumento de perímetro del antebrazo como requisitos de respuesta positiva a la prueba del vórtice, dadas su mayor facilidad de ejecución y el óptimo acuerdo entre evaluadores.
Vibratory urticaria and angioedema are a group of conditions characterized by transient localized edema following a vibratory stimulus. A significant increase in histamine and other markers of mast cell degranulation in serum has been identified during episodes.
They can be categorized1 as acquired (more common) or hereditary (exceptional).
Hereditary vibratory angioedema was originally described in 1972 by Patterson et al.2 in a family whose members developed angioedema in response to vibratory stimuli shortly after birth. Forty-four years later, Boyden et al.3 described three Lebanese families in which the Adhesion G Protein-Coupled Receptor E2 (ADGRE2) mutation was identified. Although both are hereditary, the cases reported by Patterson et al.2 affected patients who developed angioedema lesions with a history of a few hours to a few days, whereas Boyden's cases3 exhibited <1-h history transient urticaria lesions (wheals). Therefore, although the ADGRE2 mutation has not been studied in the patients of Patterson et al., it has been suggested that these represent two different entities, leading to the proposal of subcategorizing hereditary variants1 into two subtypes: “Patterson-type hereditary vibratory angioedema”2 and “Boyden-type hereditary vibratory urticaria”3 both ADGRE2-related.
Acquired cases can also be subcategorized1 into two categories: the more common type of “acquired vibratory angioedema”,1 which affects patients with a month-or-year history of sporadic angioedema triggered by vibratory stimuli,4–16 and the exceptional form of “secondary acquired vibratory urticaria”,1 a transient condition presenting as wheals triggered by a vibratory stimulus in the context of a primary trigger (e.g., Candida infection17 or hymenoptera sting18).
Most cases are triggered by the vibration inherent in certain occupational or recreational activities,4 which can lead to significant work performance impairment.16 When avoiding vibratory stimuli is not feasible – as in working environments – a good response to treatment with oral antihistamines or omalizumab has been described.16
Clinical history and response to the vortex test are essential for diagnosis confirmation purposes. According to the guidelines agreed upon by EAACI/GA2LEN/EDF/UNEV on the management of inducible urticaria,19 it is recommended to expose the volar surface of the forearm to the vibration induced by a laboratory vortex mixer for 5min (780–1380° rpm) and then assess the test results 10min later. The vortex test is considered positive if edema of the exposed area is observed (quantified as an increase in forearm circumference). Vibratory urticaria and angioedema can be misdiagnosed as other forms of inducible urticaria – dermographism or delayed pressure urticaria – if a thorough history and specific provocation tests are not performed.16
According to a recent review4 on acquired vibratory angioedema, there is notable heterogeneity in the literature regarding running and interpreting the vortex provocation test. This test was performed in 8 out of 12 reports on acquired vibratory angioedema, and forearm circumference before and after the test was reported in only two of them. These findings highlight the need to standardize the protocol for the vortex provocation test.
Moreover, it has been found that a past personal history of symptoms in response to vibratory stimuli is significantly associated with altered responses to the vortex provocation test in a high proportion of individuals in healthy volunteer populations (41.3–43%)20,21 according to questionnaire-based studies.
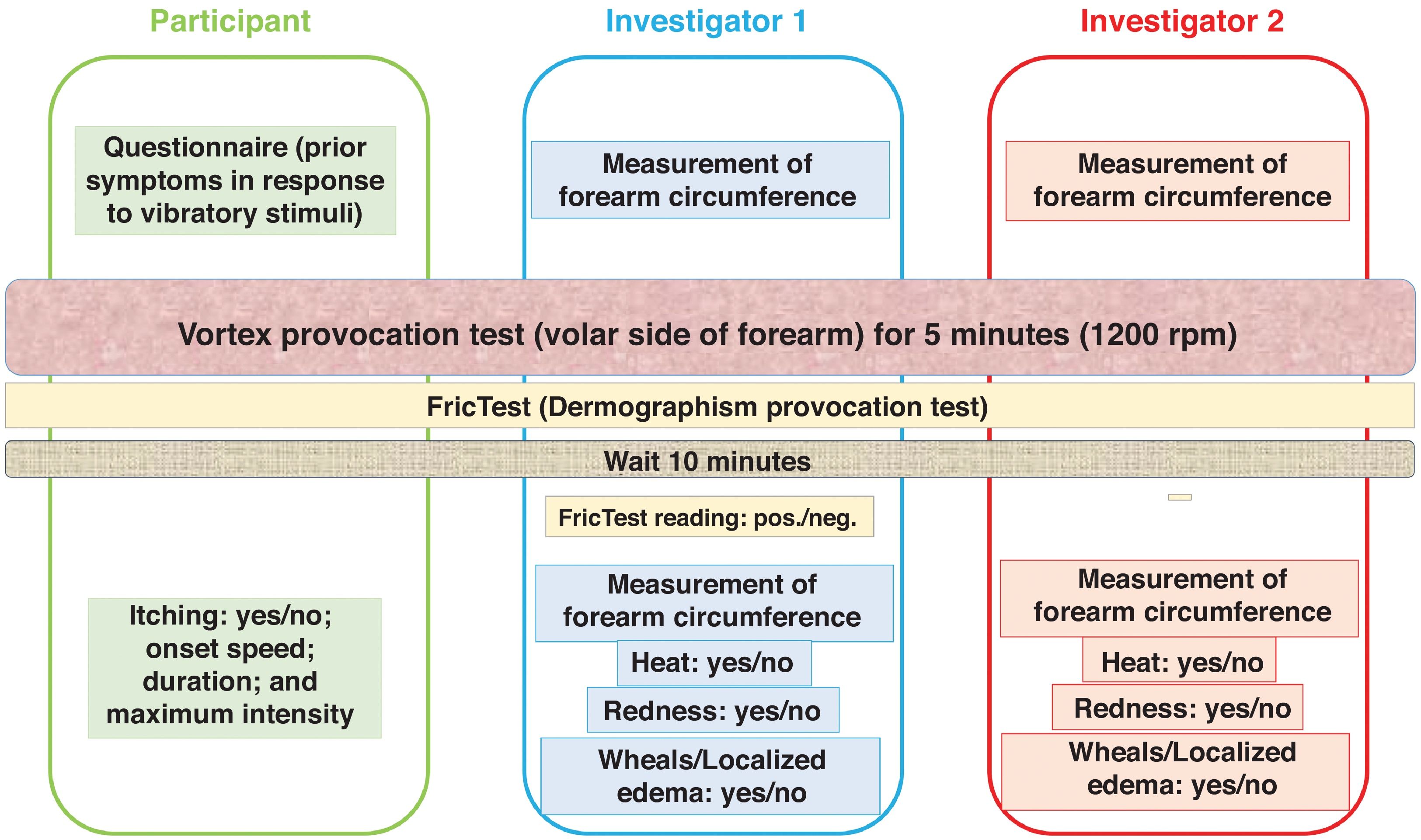
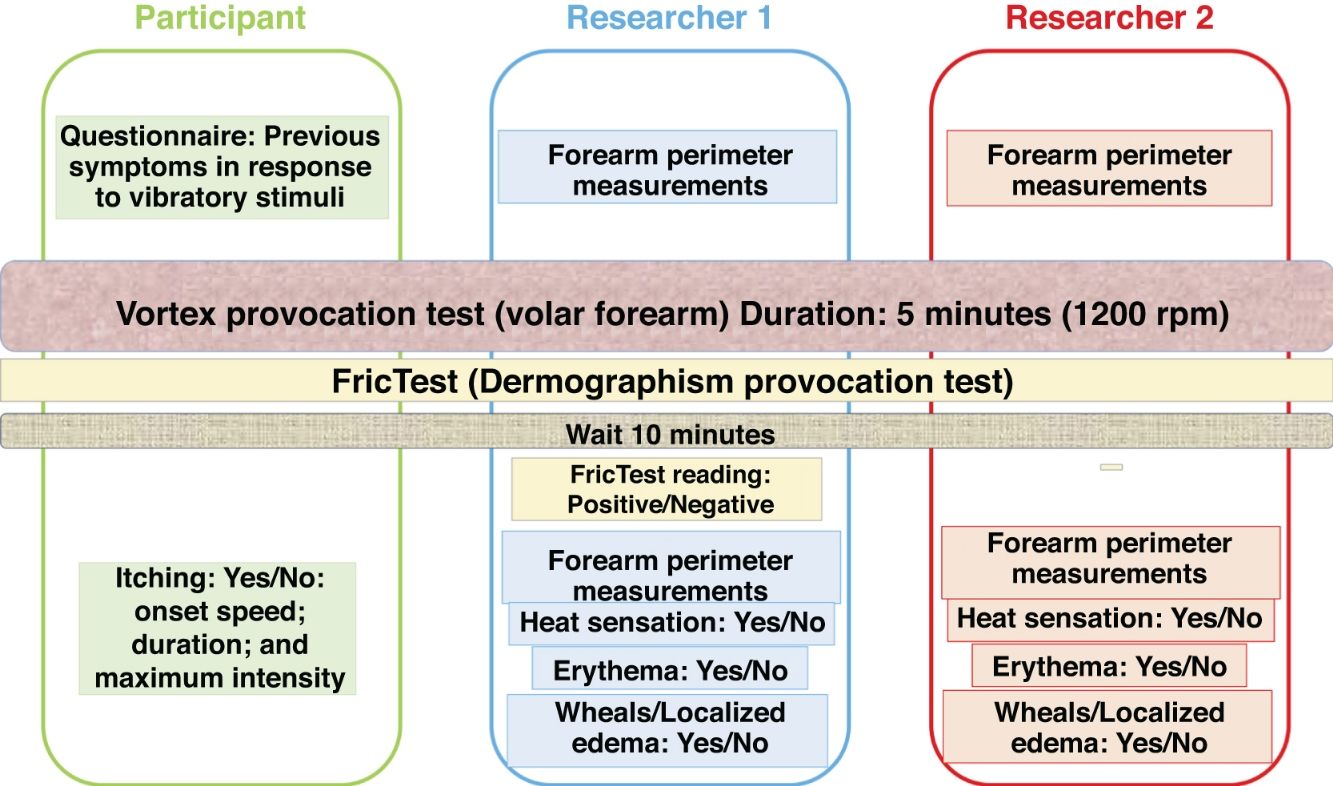
Material and methodsWe designed a study (Fig. 1) to evaluate: descriptive statistics on the prior personal history of symptoms in response to vibratory stimuli in a population of volunteers; descriptive statistics of altered responses to the vortex provocation test (with respect to the following variables: erythema, urticaria or localized edema, warmth, forearm circumference increase, and the onset, intensity, speed of onset, and duration of pruritus); inter-rater reliability of the response to the test (comparing observations made by two independent researchers at each center); and the correlation between prior symptoms due to vibratory stimuli and the response variables of the vortex test (erythema, urticaria or localized edema, warmth, forearm circumference increase, and pruritus onset, intensity, speed of onset, and duration).
Study population, involved centers, inclusion period, and inclusion/exclusion criteriaThe study population included volunteers who were health care professionals who worked in 12 Dermatology Departments in Spain (Hospital Universitario de Toledo; Hospital Universitario Infanta Leonor; Hospital Universitario Infanta Sofía; Hospital Universitario de Móstoles; Hospital Rey Juan Carlos; Hospital Universitario de Fuenlabrada; Hospital Universitario Doce de Octubre; Hospital Universitario La Paz; Hospital Universitario Fundación Alcorcón; Hospital Universitario Puerta de Hierro-Majadahonda; Hospital Universitario Gregorio Marañón; and Hospital Universitario de Guadalajara) between January and July 2021. A minimum of 10 participants were included per hospital, including physicians, nurses, nursing assistants, and administrative staff.
Inclusion criteria: Adults capable of understanding and signing informed consent.
Exclusion criteria: Dermographism defined as the presence of a wheal or linear hive appearing 10min after applying friction with a blunt object (FricTest®, pen, or dermographometer).
Tools used- 1.
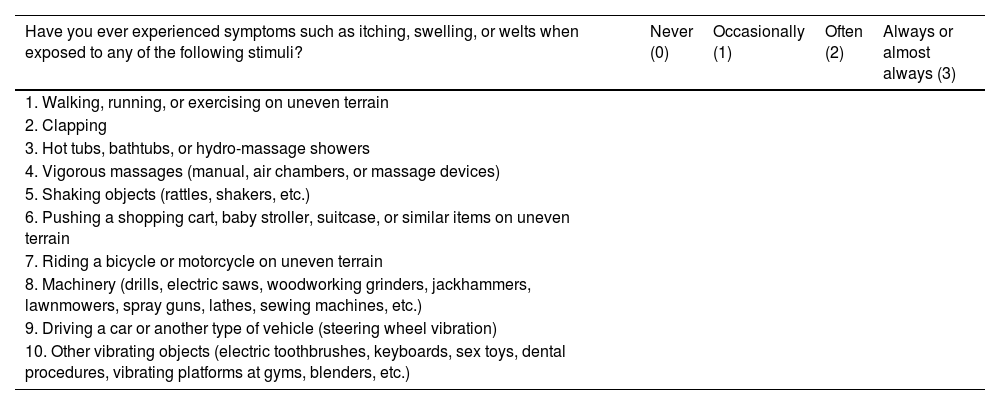
A questionnaire (Table 1) was administered to evaluate the past personal history of symptoms – frequency of pruritus or edema – in response to vibratory stimuli, with scores ranging from 0 to 30 in each case.
Table 1.Questionnaire on previous reactions to vibratory stimuli.
Have you ever experienced symptoms such as itching, swelling, or welts when exposed to any of the following stimuli? Never (0) Occasionally (1) Often (2) Always or almost always (3) 1. Walking, running, or exercising on uneven terrain 2. Clapping 3. Hot tubs, bathtubs, or hydro-massage showers 4. Vigorous massages (manual, air chambers, or massage devices) 5. Shaking objects (rattles, shakers, etc.) 6. Pushing a shopping cart, baby stroller, suitcase, or similar items on uneven terrain 7. Riding a bicycle or motorcycle on uneven terrain 8. Machinery (drills, electric saws, woodworking grinders, jackhammers, lawnmowers, spray guns, lathes, sewing machines, etc.) 9. Driving a car or another type of vehicle (steering wheel vibration) 10. Other vibrating objects (electric toothbrushes, keyboards, sex toys, dental procedures, vibrating platforms at gyms, blenders, etc.) - 2.
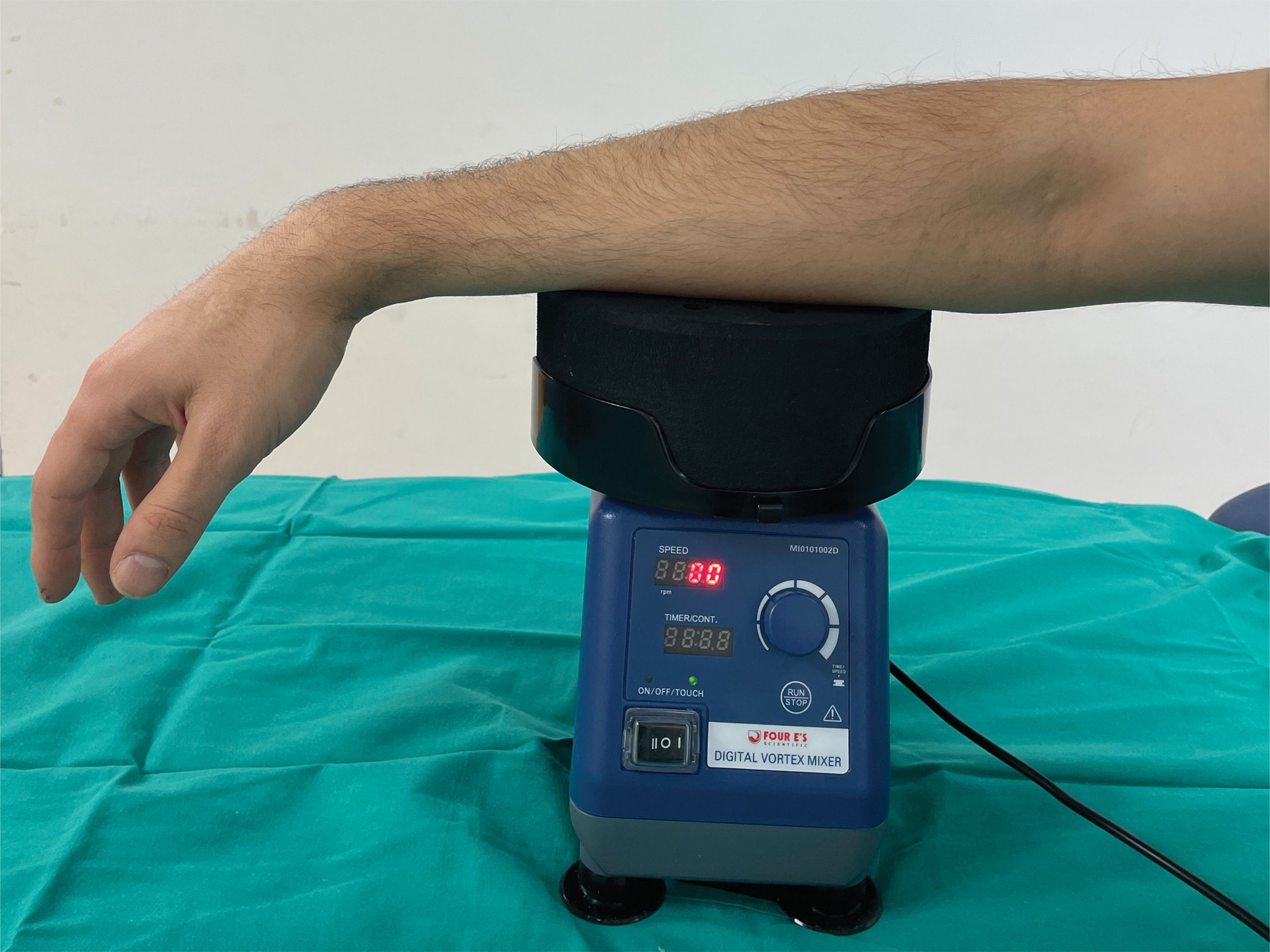
A laboratory vortex mixer at 1200rpm was used as the provocation test tool. The volar surface of each participant's forearm was exposed to vibration induced by this device for 5min. The same vortex model was used across all participant centers (Four E's Scientific Digital Vortex Mixer, model: MI0101002D, movement type: orbital; orbital diameter: 6mm; speed range: 0–3000rpm) (Fig. 2).
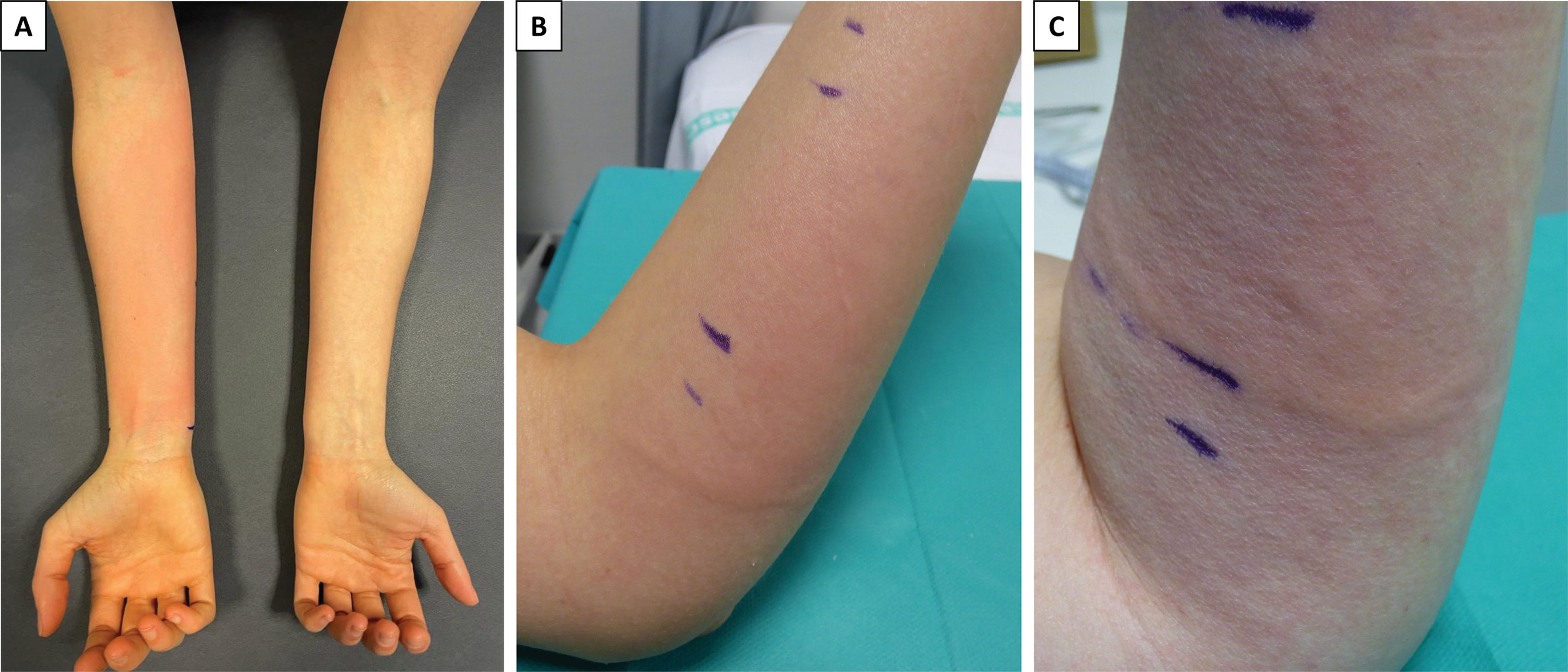
Prior to the test, at each center, two independent researchers measured the forearm circumference at three levels: proximal (below the antecubital flexure), distal (at wrist level of the styloid process), and a midpoint between the two. Multiple reference points were marked with surgical markers for consistency.
Ten minutes after completing the vibratory stimulus, the researchers conducted new measurements at the same levels. Additionally, they recorded the presence/absence of erythema, warmth, urticaria, or localized edema vs the contralateral forearm which remained non-exposed to the stimulus. Localized edema was defined as areas of linear edema corresponding to the regions in contact with the edges of the vortex plate – the point of highest vibration intensity – including <1-h history superficial linear wheals and deeper, longer-lasting angioedema lesions.
- 3.
A visual analog scale was used by participants to evaluate the intensity, speed of onset, and duration of pruritus (the only subjective response variable).
- 4.
For the dermographism provocation test, FricTest® – a dermographometer – or a blunt object was used, depending on availability at each center, immediately after the cessation of vibration. The presence/absence of dermographism was read and recorded 1° min after stopping vibration, immediately before recording the other variables.
The reproducibility of the diagnostic tests was analyzed using the intraclass correlation coefficient (ICC) and the kappa index for quantitative and qualitative variables, respectively. To evaluate the correlation between the final score of the previous symptom questionnaire and the vortex test response variables, we used Pearson/Spearman correlation coefficients for quantitative variables.
Data recording, both by the investigators at each center (regarding objective variables such as the presence of erythema, heat, hives, or localized edema, or the measurements of the forearm perimeters), and the participants (subjective variables related to itching, and responses to the previous symptom questionnaire with vibratory stimuli), was conducted using a double-blind procedure to make sure that the interpretation of the vortex test response by the investigators was not affected. The study methodology is shown in Fig. 1.
ResultsA total of 140 volunteers were evaluated, 17 of whom exhibited dermographism and were excluded. A total of 59% of the 123 participants without dermographism responded affirmatively to, at least, 1 item on the symptom questionnaire. The mean questionnaire score was 2.02, 95% CI, 1.53–2.50.
An altered response to the vortex test was observed for the qualitative variables: erythema, warmth, or urticaria/localized edema in 58.5%, 38.2%, and 32.5% of cases, respectively (Fig. 3).
Pruritus onset was reported by 73.6% of participants. The mean pruritus intensity (as estimated by participants using a visual analog scale from 1 to 10) was 3.44, 95% CI, 2.94–3.94.
The ICC used to evaluate inter-rater concordance for forearm circumference increases measured at three different levels was: 0.477, 95% CI, 0.253–0.634; 0.496, 95% CI, 0.280–0.647; and 0.370, 95% CI, 0.100–0.559, respectively. The kappa index used to evaluate inter-rater reliability for qualitative dichotomous variables, such as erythema, warmth, and urticaria or localized edema, was 0.868, 0.756, and 0.757, respectively.
The bivariate analysis (Mann–Whitney test) revealed a significant correlation between the total questionnaire score and the qualitative variables erythema, warmth, and urticaria/localized edema: asymptotic significance (Asymp Sig) for two-tailed tests: 0.000, 0.013, and 0.001, respectively.
A multivariate logistic regression analysis was performed, but combining variables did not achieve greater significance.
According to the Mann–Whitney U test for independent samples, no significant correlation was reported between the presence of pruritus and the questionnaire score (0.285). However, a significant Spearman's rank correlation coefficient was found between the questionnaire score and the intensity, onset time, and duration of pruritus: two-tailed Asymp Sig: 0.002, 0.025, and 0.001, respectively.
DiscussionSymptoms triggered by vibratory stimuli and altered responses to the vortex provocation test turned out to be a common finding in our population of health care professional volunteers across 12 dermatology departments in Spain. The percentage of affected volunteers (59%) was even higher than previously reported figures in similar studies published in the literature (41.3–43%).20,21
The high frequency of symptoms (pruritus, erythema, or edema) triggered by vibratory stimuli in this and other groups of otherwise healthy volunteers20,21 raises the practical difficulty of establishing a threshold to differentiate between physiological and pathological responses, similar to how thresholds are applied in other inducible urticarias (e.g., simple and symptomatic dermographism).4 It is possible that the classification of these responses as pathological likely depends on the degree of functional impairment and the quality-of-life deterioration due to mandatory exposure to vibratory stimuli, especially in occupational contexts.4
In our study, significant agreement between evaluators was observed regarding qualitative objective response variables in the vortex test (erythema, urticaria/localized edema, and warmth), as expected, since these variables are easy to assess by comparing the exposed and non-exposed forearm skin.
Additionally, we identified a significant correlation between these variables and the total questionnaire score, suggesting that individuals who recall prior symptoms in response to vibratory stimuli are more likely to develop an abnormal test response in terms of erythema, warmth, urticaria, or localized edema.
We also observed a significant correlation between the questionnaire score and the intensity, onset speed, and duration of pruritus, but not with the presence/absence of pruritus. This suggests that vibration may physiologically induce a mild degree of transient pruritus in some individuals with a normal test response, unlike individuals with altered responses (in terms of erythema, warmth, or urticaria/localized edema), who tend to experience earlier, more intense, and longer-lasting pruritus.
Our study found poor inter-rater reliability regarding the increase in forearm circumference, with a low intraclass correlation coefficient. We believe this may be related to the challenges investigators faced in taking forearm circumference measurements at precisely the same level before and after the test, despite meticulous use of surgical marker reference points on both sides of the forearm and efforts to apply uniform pressure with the measuring tape.
The increase in forearm circumference was described in the EAACI/GA2LEN/EDF/UNEV 2016 consensus on the management of inducible chronic urticaria as an objective parameter to quantify the vortex test response. In our opinion, the value of this consensus recommendation should be revisited due to the lack of inter-rater reliability and practical difficulties reported. These findings add to the scarce literature references on how the test should be run,4 where most studies do not report or mention the measurement of forearm circumference. When reported, differences in circumference before and after the test are minimal, often falling within the margin of measurement error, rendering them non-significant.
In contrast, the assessment of erythema, warmth, or urticaria/localized edema is straightforward compared with the contralateral forearm. These variables also demonstrate optimal inter-rater reliability and correlate significantly with the questionnaire on prior symptoms following vibratory stimuli.
We acknowledge that our results apply to unselected volunteer individuals. Further studies are needed to evaluate the behavior of all response variables to the vortex provocation test in patients suspected of having vibratory urticaria or angioedema.
ConclusionsIn conclusion, we highlight the high frequency of prior symptoms in response to vibratory stimuli among a group of healthy volunteers. Additionally, we emphasize the significant correlation between this history (total questionnaire score) and altered responses to the test across different variables.
Based on the results of this study, we suggest that the proposal outlined in the 2016 EAACI/GA2LEN/EDF/UNEV consensus document regarding forearm circumference measurement as a marker of positivity to the vortex provocation test in vibratory urticaria or angioedema is inadequate due to high inter-individual variability in observations.
We propose that other response variables, not previously considered in the consensus document – such as erythema, urticaria, localized edema, or warmth – should replace forearm circumference measurement and be considered requirements to define a positive response to the vortex provocation test. These variables are easier to assess, demonstrate optimal inter-rater reliability, and correlate with the total questionnaire score on prior symptoms. In other words, we propose that the provocation test should be considered positive if vortex-induced vibration triggers erythema, urticaria, localized edema, or warmth.
Ethical responsibilitiesThe study was approved by the Clinical Research Ethics Committee for Medicinal Products (Complejo Hospitalario Universitario de Toledo, registration No. 721) and then by the ethics committees of the other participant centers. Participation was voluntary, and all participants signed an informed consent document.
FundingThe vortex mixers were donated by Novartis Spain to the Urticaria Center (UCEN) Group in recognition of the Best Innovative Research Project of 2019 at the GEIDAC Urticaria Meeting (Segovia, Spain, 2019). This research did not receive any additional funding from public, private, or nonprofit organizations. The authors declared no financial, non-financial, or personal relationships that could be perceived as biased.
Conflicts of interestNone declared.