Dyshidrosiform eruptions have a broad differential diagnosis.1 Linear immunoglobulin (Ig) A dermatosis is a rare, autoimmune blistering disease that can be idiopathic or drug-induced,2 and is characterized by a linear deposit of IgA in the epidermal basement membrane.3,4 We describe a case of linear IgA dermatosis that began as a dyshidrosiform eruption.
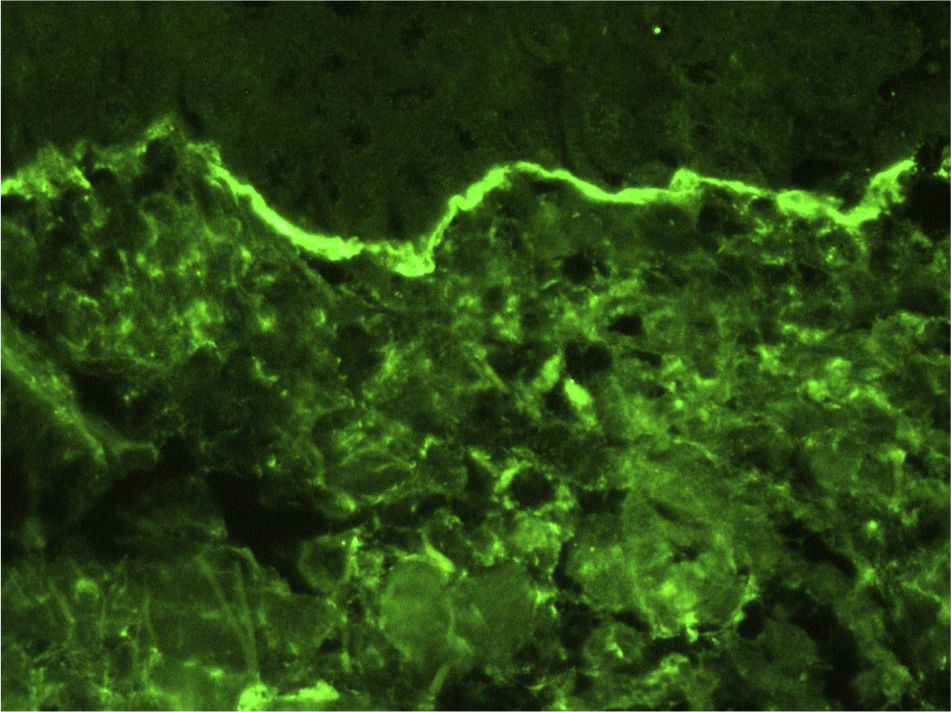
A 56-year-old woman presented at the emergency room with palmoplantar blisters and vesicles (Fig. 1) that were very painful and itchy and had appeared 24hours previously. She was diagnosed with dyshidrosis. Several days later she developed blisters on the trunk and extremities, without mucosal involvement. A biopsy of one of the lesions was performed. Three weeks previously the patient had been treated for a urinary tract infection with oral fosfomycin, and had experienced diarrhea secondary to the antibiotic treatment. Laboratory tests, including indirect immunofluorescence analysis of antinuclear, antitransglutaminase, anti-intercellular adhesion, and anti-basement membrane antibodies, were normal. Histopathology revealed subepidermal blisters that contained a papillary dermal infiltrate consisting of abundant neutrophils and formed noneosinophilic microabscesses at the tips of the papillary ridges. Direct immunofluorescence (DIF) revealed linear IgA deposition in the epidermal basement membrane, but no deposits of IgG or C3 (Fig. 2). Based on these findings the patient was diagnosed with linear IgA dermatosis. She responded well to treatment with oral prednisone with no recurrence within 6 months of stopping treatment.
While the initial appearance of palmoplantar vesicles and blisters suggested a diagnosis of dyshidrotic eczema, the subsequent appearance of lesions on the trunk and extremities was indicative of a blistering disease. Histopathology and the results of the DIF led to a diagnosis of linear IgA dermatosis.
Linear IgA dermatosis can be clinically and histologically similar to bullous pemphigoid and dermatitis herpetiformis.3 These 3 entities are characterized by subepidermal blister formation, an inflammatory infiltrate, and immunoglobulin deposition in the epidermal basement membrane. They can be distinguished by histological analysis and DIF. In dyshidrosiform pemphigoid the inflammatory infiltrate is composed mainly of eosinophils, and DIF shows a linear deposition of IgG and C3.5 Cases of IgA pemphigoid involving linear deposition of IgA and C36 have also been reported. In dermatitis herpetiformis abundant neutrophils are observed at the tips of the dermal papillae and DIF shows granular deposition of IgA.5 In linear IgA dermatosis the inflammatory infiltrate is composed mainly of neutrophils, and DIF reveals linear IgA deposition in the epidermal basement membrane.5
It should be noted that although dyshidrosiform linear IgA dermatosis is rare, several cases have been reported.7,8 This clinical form was first described in 1988 by Barth and coworkers,7 who reported 3 cases. Another case was later described by Duhra and colleagues.8 All 4 cases featured palmar involvement. Dyshidrosiform linear IgA dermatosis can be induced by drugs, most commonly vancomycin.2,9,10 While no association between fosfomycin and linear IgA dermatosis has been described, we cannot rule out the possibility that fosfomycin acted as a trigger in the present case. Treatment involves the administration of dapsone, together with corticosteroids in refractory cases.4
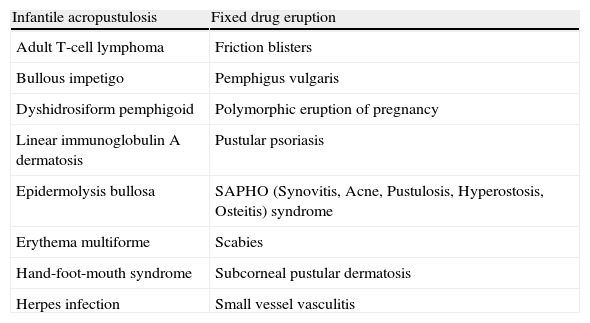
We have presented this case so that linear IgA dermatosis can be included within the broad differential diagnosis of dyshidrosiform eruptions (Table 1).1
Differential Diagnosis of Dyshidrosiform Eruptions.
| Infantile acropustulosis | Fixed drug eruption |
| Adult T-cell lymphoma | Friction blisters |
| Bullous impetigo | Pemphigus vulgaris |
| Dyshidrosiform pemphigoid | Polymorphic eruption of pregnancy |
| Linear immunoglobulin A dermatosis | Pustular psoriasis |
| Epidermolysis bullosa | SAPHO (Synovitis, Acne, Pustulosis, Hyperostosis, Osteitis) syndrome |
| Erythema multiforme | Scabies |
| Hand-foot-mouth syndrome | Subcorneal pustular dermatosis |
| Herpes infection | Small vessel vasculitis |
Adapted from Wollina,1 2010.
Please cite this article as: Borja-Consigliere H, Ormaechea-Pérez N, Lobo-Morán C, Tuneu-Valls A. Dermatosis Inmunoglobulina A lineal dishidrosiforme. 2014;105:429–430.