The eyelid is subject to considerable deformity owing to the particular laxity of the subcutaneous cellular tissue, which is caused by infiltration of the interstitial spaces. The degree of swelling can range from simple tumefaction of the ciliary margin to a considerable increase in periocular tissue volume, which in some cases can lead to narrowing, or even closure, of the palpebral fissure. Differential diagnosis of eyelid swelling is complex. It requires a meticulous physical examination and inclusion of both inflammatory and noninflammatory causes. The main noninflammatory cause is acute hypothyroidism, as in the present case.1
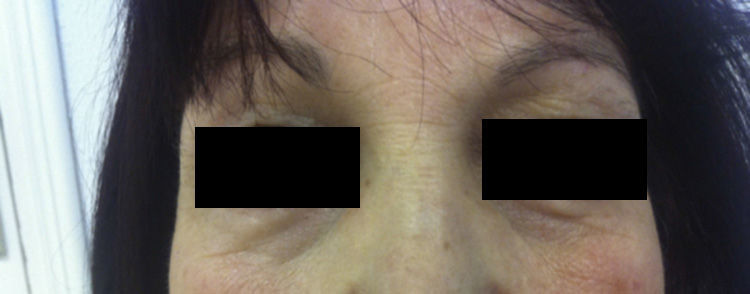
We describe the case of a 52-year-old woman who presented with a 1-week history of sudden-onset bilateral eyelid swelling that was neither painful nor pruriginous. Her personal history was remarkable for autoimmune hypothyroidism (Hashimoto thyroiditis) that first appeared 5 years previously and for which she was receiving hormone replacement therapy (levothyroxine 75μg/d). She also had a 1-year history of autoimmune hepatitis, which was treated with prednisone (7.5mg/d po), and hypertension, which was treated with enalapril (20mg/d po). She attended our clinic with bilateral eyelid swelling that had begun 24hours earlier. The patient had not ingested new drugs, experienced injury, received insect bites or stings, or applied cosmetic products to the area. Examination revealed soft bilateral edema that was more pronounced on the right side with discrete erythema and no crepitus, vesicles, or desquamation (Figs. 1 and 2). Her visual acuity and eye movement were unaltered, and she had no skin lesions at other sites. The results of a full laboratory workup were normal, although thyroid-stimulating hormone (TSH) was 50.3mIU/L and free thyroxine was diminished (0.5ng/dL). The dose of levothyroxine was increased considerably (500μg/d), as was that of oral prednisone (15mg/d), to reduce inflammation. Seven days after the first visit, her TSH level had fallen to 35mIU/L, thyroid hormone levels had returned to normal, and the swelling had improved considerably. A week later, the skin complaint was in total remission (Fig. 3) and the TSH concentration had fallen to 20mIU/L.
The characteristics of the lesion and the clinical course confirmed a diagnosis of bilateral eyelid swelling associated with acute hypothyroidism.
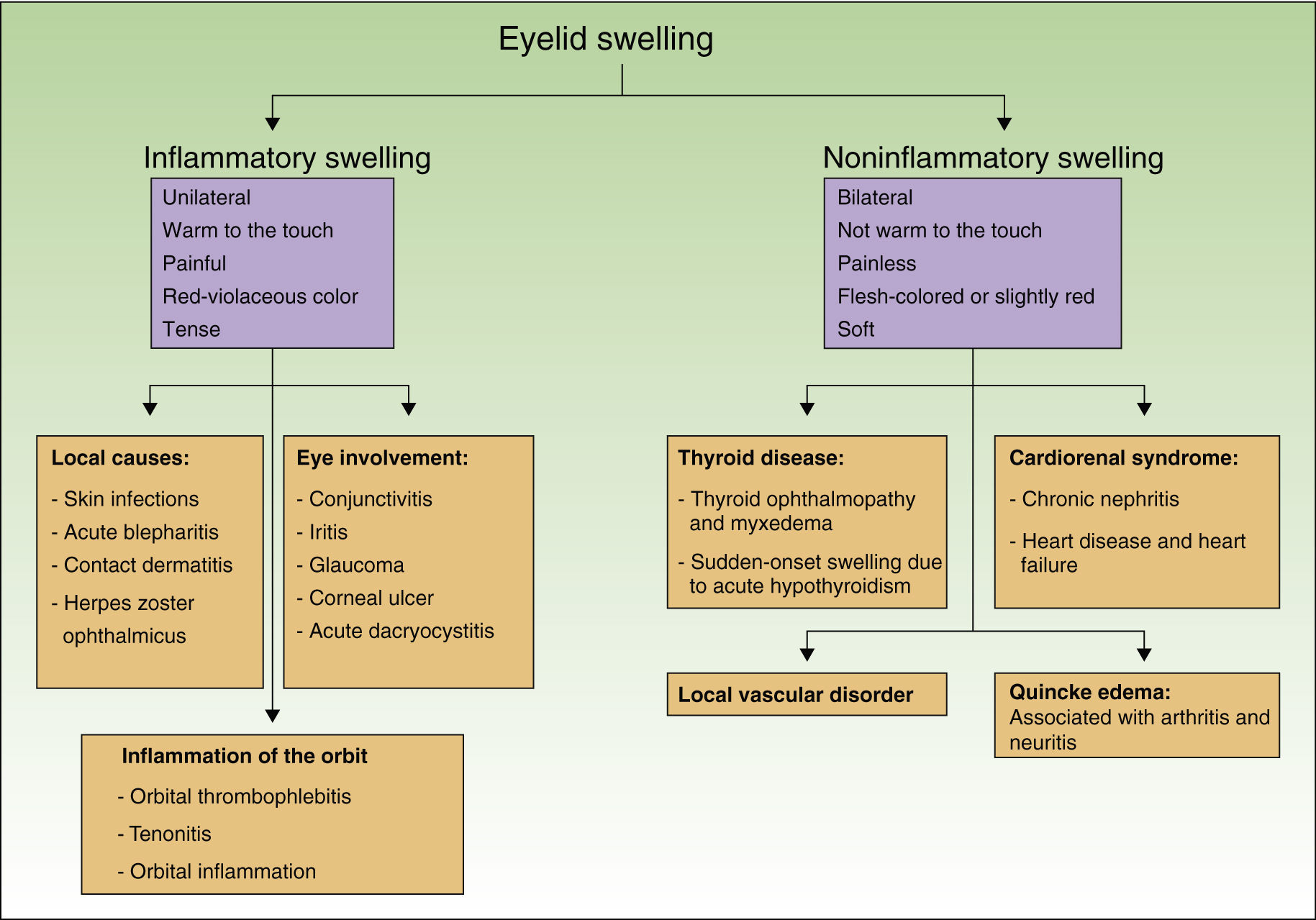
The differential diagnosis of eyelid swelling should include various clinical entities (Fig. 4). A careful evaluation should be made of the intensity, location (one or both eyelids), and coloring of the swelling. The initial examination first makes it possible to rule out swelling caused by trapped air, with its characteristic crunching snow sensation, and blood pooling in the case of hematoma. Finally, it is necessary to define whether the swelling is inflammatory or noninflammatory and analyze the possible causes.
Eyelid swelling associated with hypothyroidism is uncommon and can occasionally mimic other conditions such as angioedema, bites and stings, and contact dermatitis.2 In the case we describe, the absence of induration, vesicles, and pruritus make a diagnosis of eczema or angioedema unlikely; in addition, the patient's clinical condition improved considerably when the acute hypothyroidism resolved. The causes of swelling are not well known, although mucopolysaccharide deposits play a role. Case reports show that eyelid swelling is a clinical sign of severe acute hypothyroidism. It is sometimes more subtle, is associated with thinning of the eyebrows,3 and, in some cases, can manifest as palpebral redundancy resulting from laxity of the eyelid.4 The swelling resolves gradually with treatment of hypothyroidism.4,5
Eyelid swelling is not the only dermatologic manifestation associated with hypothyroidism, and other more common presentations sometimes go unnoticed. In more than 80% of cases the epidermis is thin, dry, rough, hyperkeratotic, and covered with fine superficial scales.6 The hair is opaque, rough, and brittle, partly owing to reduced secretion of sebum. Alopecia has been reported in up to 50% of patients and can be diffuse or partial; the nails are thin and fragile with striations and horizontal and longitudinal ridges.7
Finally, in the case of sudden-onset asymptomatic bilateral soft swelling in which dermatitis and angioedema can be ruled out, systemic causes such as hypothyroidism should be suspected. Therefore, eyelid swelling can be a sign of numerous local and systemic diseases and requires a meticulous clinical workup in order to determine the cause and enable appropriate treatment to be started.
Please cite this article as: Salazar-Nievas M, Arias-Santiago S. Edema palpebral bilateral asociado a crisis hipotiroidea. Actas Dermosifiliogr. 2014;105:427–429.