A 62-year-old woman visited our department with skin lesions that had appeared 5 years earlier and presented in outbreaks. The lesions had begun in the submammary folds and later spread to other areas, predominantly in skin folds. She had received different treatments, often corticosteroids and antifungal agents, both topical and oral, with which the lesions had initially improved without disappearing. The area affected had increased considerably in the previous year, affecting the patient's quality of life.
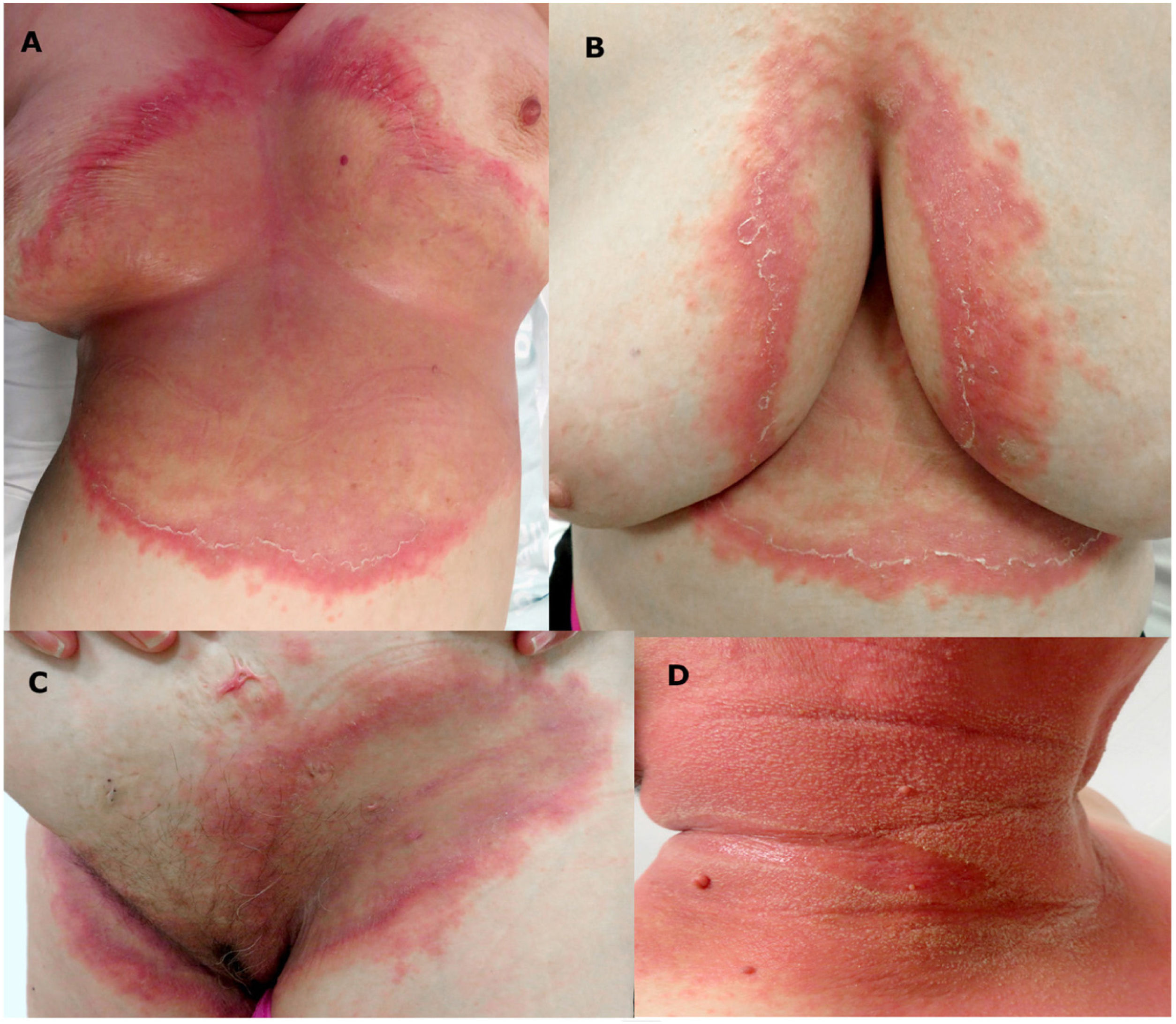
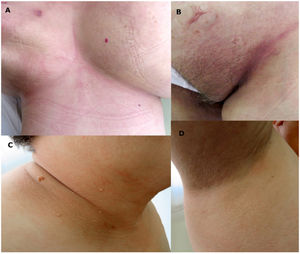
The examination revealed large erythematous plaques with erosive borders showing micropustules (Fig. 1), involving the submammary and intermammary area, the groin, the lateral surfaces of the neck, the antecubital fossa, and the axillae.
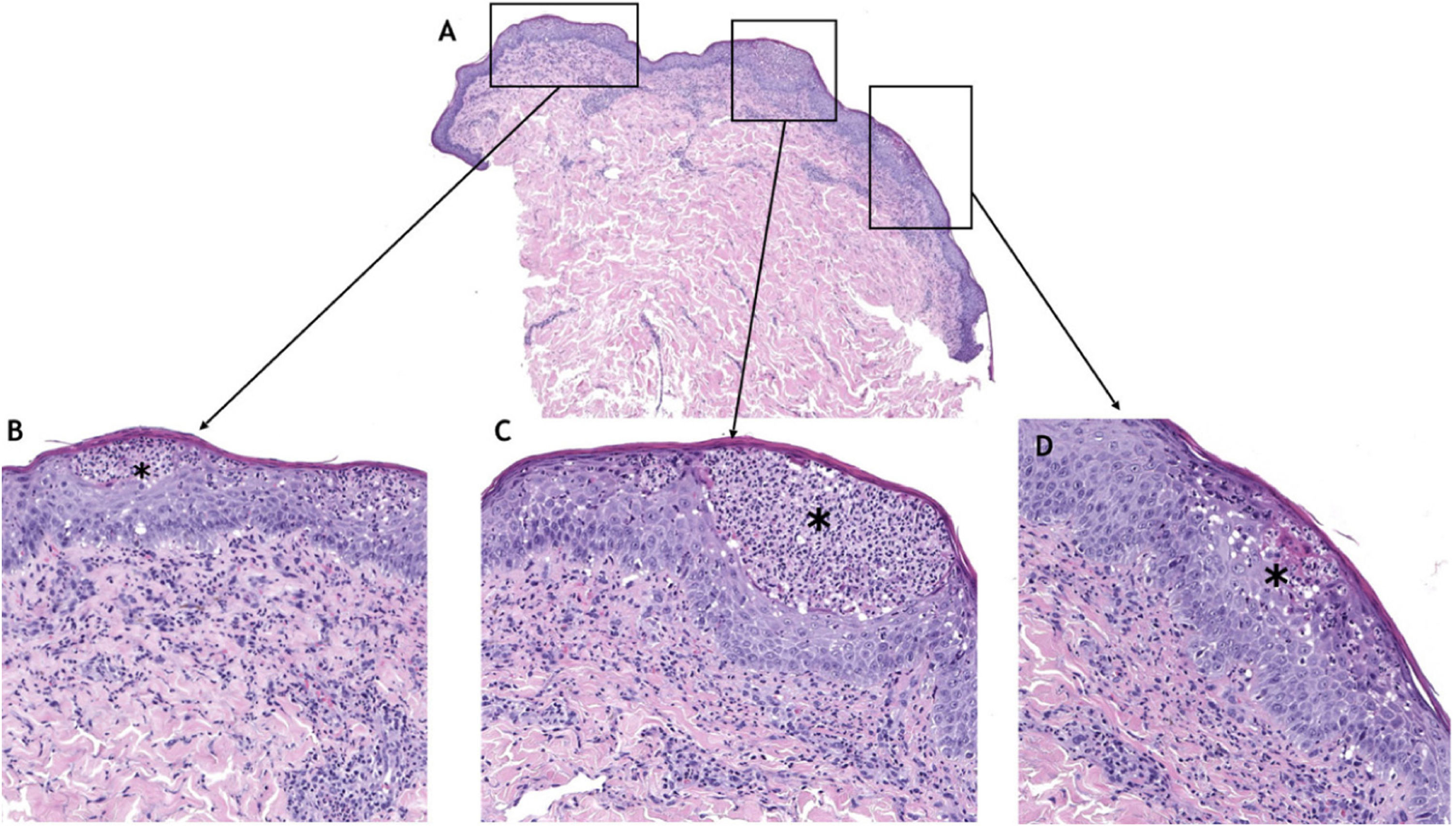
Microbiology cultures were negative for fungi and bacteria. Histology of a biopsy of one of the lesions revealed a dense, predominantly epidermal neutrophilic infiltrate with subcorneal accumulations (Fig. 2). It was not possible to perform a direct immunofluorescence (DIF) study of the lesions.
Furthermore, a blood test was positive for antinuclear antibodies (ANA) with a high titer (1/1280) and a centromeric pattern (AC-3), for double-strand anti-DNA (anti-DNA-ds), and for anticentromere, M2 recombinant antimitochondrial antibodies. The test also revealed increased activated partial thromboplastin time (APTT), compatible with lupus anticoagulant in the blood (also positive). No other abnormalities of note were found in the rest of the tests, except for elevated levels of cholesterol and triglycerides.
These abnormalities were unknown until that moment and suggested the presence of an autoimmune disease. The patient, however, stated that she had no history or associated current clinical manifestations.
In light of the clinical, histologic, and analytical findings (shown in Table 1), amicrobial pustulosis of the folds (APF) was diagnosed.
Diagnostic Criteria.
| Obligatory criteria | Minor criteria |
|---|---|
| Pustulosis affecting ≥1 major skin folds, affecting ≥1 minor skin folds and the anogenital fold | Association with ≥1 autoimmune disease |
| Histology: intraepidermal spongiform pustules and a principally neutrophilic infiltrate in the dermis | ANA with a titer of ≥1/160 (antinuclear antibodies) |
| Negative culture of an intact pustule | Presence of ≥1 of the following antibodies:• ENA (extractable nuclear antigen), anti-DNA• Anti-smooth muscle• Anti-mitochondrial• Anti-parietal gastric cell• Antiendomysial |
| The diagnosis of APF can be confirmed if the obligatory criteria and at least 1 of the minor criteria are met. |
Source: Diagnostic criteria for antimicrobial pustulosis of the folds, proposed by Marzano et al.3
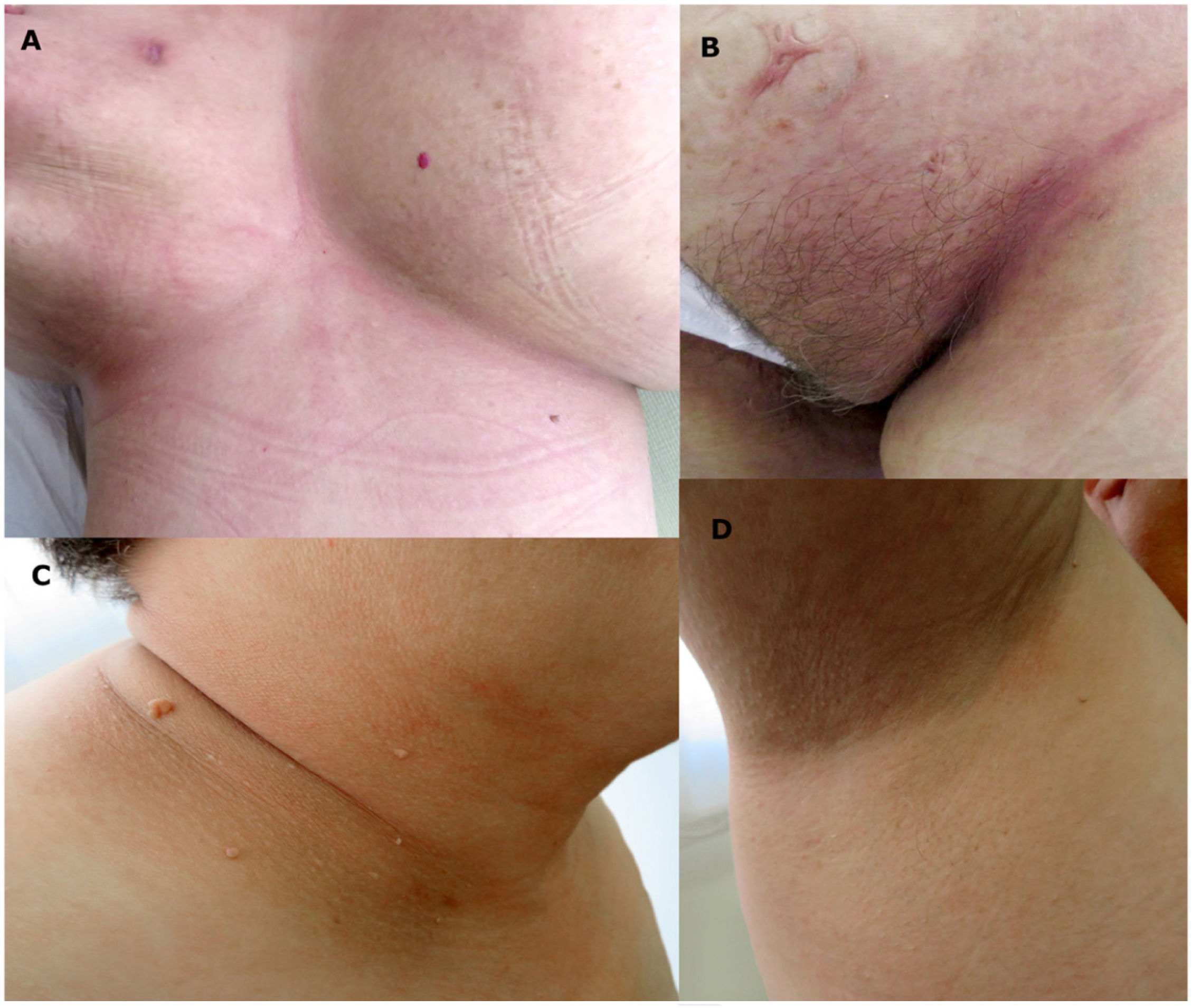
Oral corticosteroids are among the most widely used drugs in this disease. Our patient reported that they had proven ineffective on previous occasions and that they had caused adverse effects. We therefore decided to prescribe oral doxycycline at a dosage of 100mg per day and topical zinc sulfate. After 2 months of treatment, the lesions had disappeared completely, both on the neck and on the torso, with minimal erythema remaining at the bottom of the inguinal fold (Fig. 3). Given the practical resolution of the lesions, we decided to suspend treatment. The patient has not presented new lesions after a year of follow-up.
APF was first described in 1991 as a pustular rash in young women with systemic lupus erythematosus (SLE).1 Since then, fewer than 100 cases have been reported. In 2017, Schissler et al. performed a review that included 63 patients.2 Clinically, it is characterized by outbreaks of pustular lesions that predominantly affect the skin folds. Other typical areas, such as the external auditory canal, scalp, and anogenital region, may also be affected.2–5 It occurs in the context of a known autoimmune disease, typically SLE, but since it was described, many underlying diseases have been reported (thyroiditis, rheumatoid arthritis, Sjögren syndrome, etc.). In some patients, the only finding is abnormal analytical results, with no clinical criteria for any specific disease. Some cases have been described in patients with inflammatory bowel disease treated with tumor necrosis factor ɑ.6,7
In 2008, Marzano et al. proposed diagnostic criteria, which are shown in Table 1.3
The condition has been considered to be a superficial or epidermal variant of the spectrum of neutrophilic dermatoses,8 given the strong presence of neutrophils in the histology samples examined.
Neutrophils are part of the innate immune system and, therefore, neutrophilic dermatoses are included among autoinflammatory diseases. In these diseases, the increase in proinflammatory cytokines generates accumulations of neutrophils in the tissues.8 Although autoimmune and autoinflammatory diseases have different pathogenic mechanisms, coexistence of neutrophilic dermatoses and autoimmune diseases is not uncommon, the principal example of which is APF and SLE. Some authors have suggested renaming this entity neutrophilic cutaneous lupus8,9 and classifying it as one of the clinical manifestations of SLE.9–11
With regard to treatment, many therapeutic alternatives have been used, from ascorbic acid supplements or cimetidine to biological drugs.2 Oral corticosteroids have traditionally been considered the most effective drug, although relapses are frequent on suspension of treatment. Other drugs have therefore been used as corticosteroid-sparing agents, the most widely used of which are methotrexate, hydroxychloroquine, and dapsone.2
Treatment with oral antibiotics has generally been considered to be ineffective, except for superinfections secondary to the lesions.5 Doxycycline is an antibiotic of the tetracycline family that is widely used in dermatologic diseases such as acne and rosacea, not so much because of its antimicrobial power but because of its anti-inflammatory capability. It has practically no contraindications and its adverse effects are mild and transitory.
Its use in APF has only been reported in a poster at the Congress of the American Academy of Dermatology (AAD) in 2017, which described a single patient treated with this drug with good results.12 It was also used in conjunction with ivermectin to treat Demodex infestation on existing APF lesions in one patient.13
Finally, we selected this case because this is a rare entity that was first described relatively recently. In most patients, the autoimmune disease is diagnosed first, but the clinical skin manifestations may sometimes begin before diagnosis. Therefore, in clinically compatible pictures, it is worth checking for potential associated autoimmune diseases.
Furthermore, we highlight our good experience with doxycycline, which although limited, suggests that it may be considered as a valid alternative to classically used treatments, such as oral corticosteroids and other immunosuppressive agents, without the long-term adverse effects of those agents.
Conflicts of InterestThe authors declare that they have no conflicts of interest.