Dissecting cellulitis (DC) is a chronic, neutrophilic scarring alopecia that mainly affects the vertex and occipital areas of the scalp.1 Its hallmark clinical features include papules, pustules, nodules, and abscesses. This condition predominantly afflicts young black men of African descent, with rare occurrences in women and children, as evidenced by limited reports.2,3 While the precise causes remain elusive, genetic, and environmental factors, local trauma, imbalance of the scalp microbiota, and androgens seem to play a role.2,4
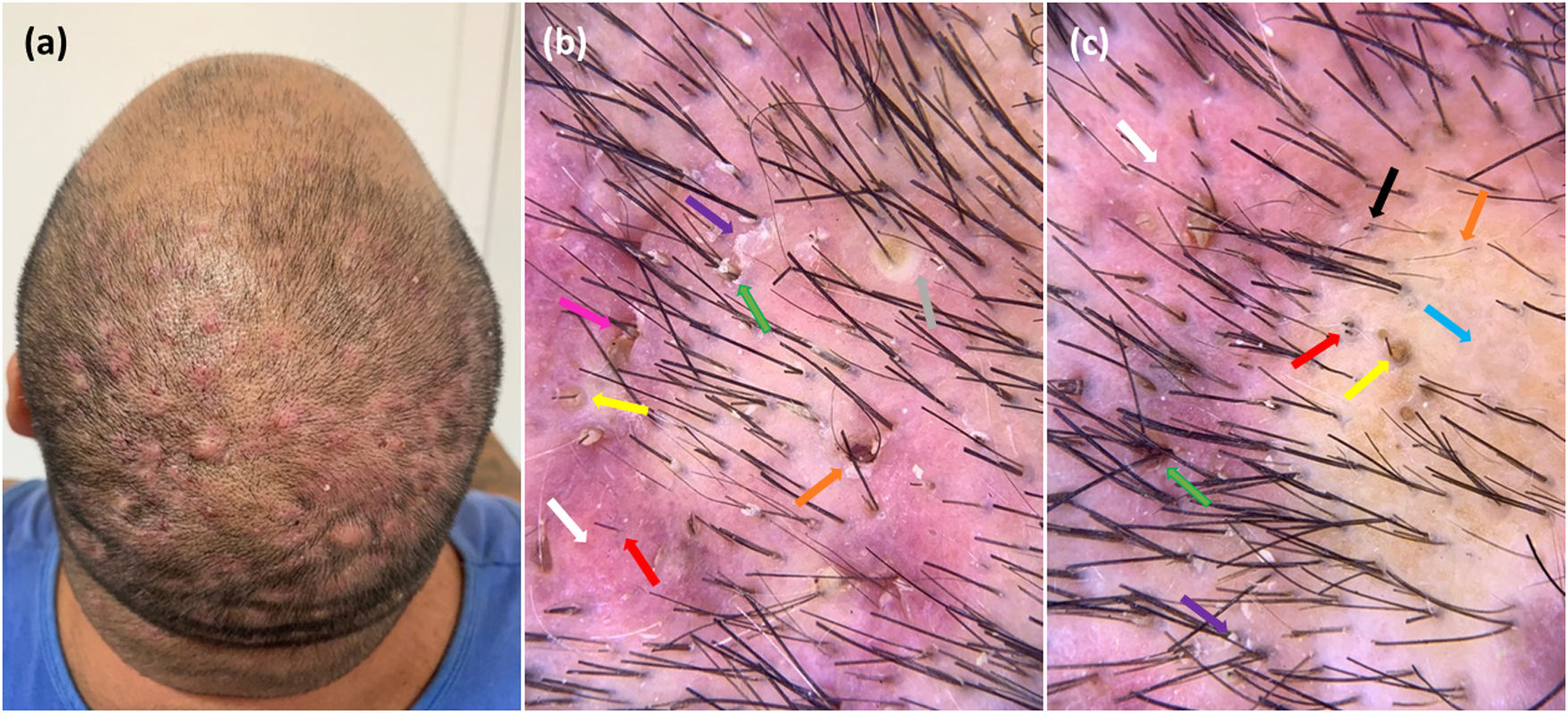
This is the case of a 55-year-old Fitpatrick phototype IV transgender male on androgen hormone therapy. The patient had been on intra-muscular testosterone for over a decade and presented with a several-month history of scalp nodules, abscesses, pruritus, and alopecia on the vertex and mid-scalp (Fig. 1A). Trichoscopy examination was noticeable for broken hairs, pustules, 3D yellow dots, scaling, erythema, polytrichia, and areas with absent follicular openings (Fig. 1B, C).
(a) Clinical image of a 55-year-old transgender man on androgen hormone therapy showing nodules, pustules and alopecia on the vertex and mid-scalp. (b) Trichoscopic image demonstrating a three-dimensional yellow dot (yellow arrow), polytrichia (green arrow), a large brown dot (orange arrow), diffuse erythema (white arrow), cutaneous clefts with emerging hairs (pink arrow), peri- and interfollicular scale (purple arrow), and broken hairs (red arrow). (c) Trichoscopy image showing a three-dimensional yellow dot (yellow arrow), polytrichia (green arrow), structureless area (blue arrow), short regrowing hair (orange arrow), diffuse erythema (white arrow), peri and interfollicular scales (purple arrow), black dots (black arrow), and broken hair (red arrow).
The word “transgender” is a generic term to describe persons whose gender identity or expression differs from the biological sex assigned at birth (between 0.1% and 2% of the population).1 These individuals may choose to undergo gender-affirming hormone therapy to align their physical characteristics with their affirmed gender,6 which in our patient consisted of testosterone therapy.4 The biological plausibility between gender/sexual hormones and the disease has been proposed due to the remarkable male predominance of this condition.2,3,5 DC is part of the “follicular occlusion tetrad” wherein the obstruction of the follicular infundibulum is considered the initial event.1,3,5
Testosterone affects the sebaceous gland primarily through local conversion to dihydrotestosterone (DHT) via 5-alpha reductase Type 1.6 Among all androgens, DHT binds cytoplasmic androgen receptors with the highest affinity. These receptors are expressed most abundantly in sebocytes, eccrine sweat epithelium, and dermal papilla cells and trigger a chain of metabolic events, which lead to excessive production of keratinocytes and sebum.6
The proliferating ductal lining cells, unable to escape the infundibulum of the pilosebaceous units, form a plug.6–8 Follicular dilation followed by rupture, keratin debris, and the presence of bacteria stimulates inflammation, abscess formation, and sinus tracts, eventually causing alopecia.1,5 The role of androgenic anabolic steroids on DC is further supported by Motosko et al. who described 1 case of abrupt onset of the disease in a male who used androgenic anabolic steroids for recreation for performance enhancement.9 Similarly, in our patient, the prolonged use of testosterone for gender-affirming purposes seemed to be the key factor inducing the disease in an otherwise unusual candidate.
DC is a rare condition that affects almost exclusively men with remarkable psychosocial impact. Its presence in a transgender man on androgenic therapy seems to be yet another piece of evidence of its pathogenic puzzle. Trichoscopy is useful in detecting the evolutionary stages of DC, early diagnosis, and monitoring the patient during treatment.10
In conclusion, DC is a stigmatizing disease with a prominent impact on quality of life. With the modern use of androgen therapy for gender reassignment, physicians should be aware of the possibility of this condition in transgender males on hormone treatment to tackle its signs before irreversible damage occurs.
StatementThe patient in this manuscript has given written informed consent to publication of the case details.
Funding sourceNone.
Conflict of interestThe authors declare no conflict of interests regarding this paper.
Data availability statementAll data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.