Verrucous venous malformation (VVM) is a rare vascular lesion currently classified as a vascular malformation by the International Society for the Study of Vascular Anomalies (ISSVA). Diagnosis is based on the integration of clinical and pathologic findings. In this article, we describe the ultrasound features of 3 VVMs and propose ultrasound as a useful, noninvasive diagnostic and follow-up tool that can also be used to guide and optimize treatment.
We selected 3 patients with histologically confirmed VVM from the database in our department. Their lesions were assessed and compared using 22-MHz cutaneous ultrasound.
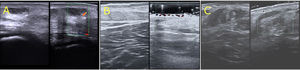
Patient 1 was a 10-year-old boy with a VVM on his left ankle that had been present since birth (Fig. 1A). Ultrasound showed a thickened, hyperechoic epidermis with hypoechoic vascular channels in the dermis and subcutaneous tissue and no color Doppler signal (Fig. 2A).
Clinical images of verrucous venous malformations. A, Patient 1. Verrucous erythematous violaceous plaque on the left ankle. B, Patient 2. Erythematous, violaceous, hyperkeratotic plaques with satellite lesions and hemorrhagic superficial vesicles on the back of the right leg. C, Patient 3. Erythematous, violaceous plaques with a verrucous surface comprising hyperkeratotic areas and crusts involving the circumference of the distal region of the left leg.
Ultrasound images of verrucous venous malformations (VVMs). A, Cutaneous ultrasound (22 MHz) of the VVM in patient 1. Thickened hyperechoic epidermis, hypoechoic dermis, hypoechoic vascular channels in the dermis and subcutaneous tissue, and absence of color Doppler signal. B, Cutaneous ultrasound (22 MHz) of VVM in patient 2. Thickened, hyperechoic epidermis with vascular channels in the superficial and deep dermis; no color Doppler signal. C, Cutaneous ultrasound (22 MHz) showing hyperechoic epidermis, decreased dermal echogenicity, and a loss of definition between the dermis and hypodermis. Note the thickened, heteroechoic subcutaneous tissue and absence of a color Doppler signal.
Patient 2 was a 25-year-old man with a VMM on the back of his right leg that had been present since birth (Fig. 1B). The patient had experienced recurring episodes of ulceration, pain, and bleeding over the previous 4 years. Cutaneous ultrasound showed a thickened, hyperechoic epidermis with vascular channels in the superficial and deep dermis. Again, there was no color Doppler signal (Fig. 2B).
Patient 3 was a 12-year-old boy with a circumferential VVM in the distal region of his left leg that had been present since birth (Fig. 1C). In recent years, the lesion had gradually gained in volume and become increasingly hyperkeratotic; it had also shown ulceration and bleeding. Cutaneous ultrasound showed a thickened, hyperechoic epidermis, decreased echogenicity in the dermis, a loss of definition between the dermis and hypodermis, hypodermal thickening and heterogeneity, and no color Doppler signal (Fig. 2C).
VVM is uncommon and is included in the group of vascular malformations in the 2018 ISSVA classification.1 It has been linked to a somatic mutation in the MAPK3 gene.2
VVM consists of a proliferation of venous blood vessels in the dermis and subcutaneous tissue, with sparing of the fascia and muscle tissue. It is congenital or develops in early childhood and mainly affects the lower extremities. Lesions are typically unilateral. Complications include bleeding, pain, and ulceration, especially in larger, more hyperkeratotic lesions. VVM is not associated with tissue hypertrophy or other developmental abnormalities.3
Diagnosis is usually established by correlating clinical and pathologic findings, although characteristic clinical findings typically help guide diagnosis. Histology shows epidermal acanthosis and papillomatosis, with compact hyperkeratosis and dilated venous vessels in the papillary and reticular dermis and subcutaneous tissue. Endothelial cells are positive for GLUT-1 and WT-1 and negative for D2-40 on immunostaining.4
Cutaneous ultrasound is a useful alternative to invasive diagnostic tests in the setting of vascular lesions. The ultrasound characterization of VVM is not well established, but based on our findings, we propose a description that could help diagnose this entity. Ultrasound features of VVM include a thickened, hyperechoic epidermis, a loss of definition between the dermis and epidermis, hyperechoic channels in the dermis and subcutaneous tissue, and absence of a color Doppler signal (Fig. 2).
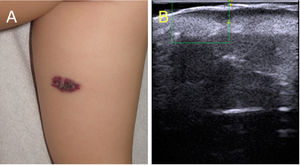
Angiokeratoma circumscriptum is the main entity to be considered in the differential diagnosis (Fig. 3A)5. Its histologic features include hyperkeratotic acanthosis and dilated capillaries in the papillary dermis, with no involvement of the deep dermis or subcutaneous tissue. Contrary to VVM, angiokeratoma circumscriptum shows negative endothelial expression of GLUT-1 and WT-1 and positive expression of D2-40 on immunostaining.6 Given the differences in the depth of involvement, ultrasound could help distinguish between the 2 entities without the need for invasive tests. Ultrasound features of angiokeratoma include epidermal thickening and hyperechogenicity and a hypoechoic lesion limited to the papillary dermis. As with VVM, there is no Doppler signal (Fig. 3B).7
Clinical and ultrasound image of an angiokeratoma. A, Angiokeratoma circumscriptum. Erythematous plaque with a hyperkeratotic surface, clinically indistinguishable from verrucous venous malformation. B, Cutaneous ultrasound (22 MHz). Epidermal hyperechogenicity with vascular channels limited to the papillary dermis; no color Doppler signal.
The treatment of VVM is largely surgical, but surgery can sometimes be complex. No treatment is an option in the absence of cosmetic concerns or symptoms.8 Pulsed dye, multiplex, and carbon dioxide laser therapy have been used to treat complications such as ulceration and bleeding and to achieve better cosmetic outcomes.9 It should be noted that laser therapy does not resolve deep lesions and is associated with a risk of recurrence. Good results with topical and oral sirolimus have been described.10
Ultrasound could also be useful for monitoring the treatment of VVM as it identifies deeper areas of involvement, which can be treated surgically, and more superficial areas, which can be treated with laser therapy or topical sirolimus. A combination of approaches may improve outcomes.
In conclusion, cutaneous ultrasound appears to be a useful tool for diagnosing VVM and differentiating it from angiokeratoma. It may also be of value for planning and monitoring treatment.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Amat-Samaranch V, Morales-Múnera C, Puig L, Roé E. Utilidad de la ecografía cutánea para el diagnóstico de la malformación venosa verrucosa. Actas Dermosifiliogr. 2021;112:958–961.