Recent years have seen a progressive increase in the incidence of sexually transmitted infections (STIs).1 Since the French scientists Barré-Sinoussi and Luc Montagnier identified the human immunodeficiency virus (HIV) as the causative agent of AIDS in 1983 and cases were reported worldwide, awareness programs and information campaigns have been developed to help prevent unsafe sexual practices. Although more than 95% of patients present skin manifestations during the course of the disease, in the vast majority of cases these occur in advanced stages.2 Because dermatologists frequently manage the diagnosis and treatment of patients who consult for an STI or risky sexual contact, it is important that they perform serology for early detection of primary HIV infection in these patients. In this study we quantify new diagnoses of HIV infection made in a dermatology department and describe the corresponding clinical and epidemiological characteristics.
Data on all cases of new HIV diagnoses made between July 2016 and July 2019 in the dermatology department of Hospital General Universitario de Valencia were obtained from the department's STI database. Early diagnosis was defined as a CD4 count >350 cells/µL in the first tests performed after diagnosis of HIV infection; late diagnosis as a CD4 count <350 cells/µL; and advanced disease as a CD4 count <200 cells/µL.
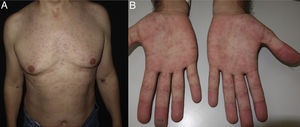
A total of 18 new HIV diagnoses were established during the 3-year study period, accounting for 1.9% of the total number of STIs diagnosed (n = 940). The clinical and epidemiological characteristics of the patients are shown in Table 1. Twelve of the cases (66.7%) were diagnosed in the screening analysis performed when the patient consulted for an STI. In 2 cases, the diagnosis was not associated with any other concomitant disease or STI. In these 2 cases, both patients presented with acute retroviral syndrome associated with general malaise, asthenia, and a generalized morbilliform macular rash with palmar–plantar involvement that had begun 2 weeks earlier (Fig. 1). Both had normal CD4 lymphocyte counts.
Clinical and Epidemiological Characteristics of Patients Diagnosed With de Novo Human Immunodeficiency Virus Infection
| Variable | Number of Cases, n (%) |
|---|---|
| Sex | |
| Male | 17 (94.4) |
| Female | 1 (5.6) |
| Mean age, y | 37 |
| Region of Nationality | |
| Spain | 13 (72.2) |
| Latin America | 4 (22.2) |
| Africa | 1 (5.6) |
| Sexual orientation | |
| MSM | 15 (83.3) |
| Heterosexual | 3 (16.7) |
| Casual diagnosis after laboratory test | 16 (88.8) |
| Associated diagnosis (n = 16) | |
| Syphilis | 7 (38.8) |
| Kaposi sarcoma | 3 (16.7) |
| Condylomata acuminata | 2 (11.1) |
| Gonococcal urethritis | 2 (11.1) |
| Bacillary angiomatosis | 1 (5.6) |
| Lymphogranuloma venereum | 1 (5.6) |
| Emergency dermatological consultation | 14 (77.8) |
| History of previous STIs | 12 (66.7) |
| Stage at diagnosis | |
| Early diagnosis | 14 (77.8) |
| Late diagnosis | 3 (16.7) |
| Advanced diagnosis | 1 (5.6) |
Abbreviations: MSM, men who have sex with men; STI, sexually transmitted infection.
According to the Spanish National Registry of HIV and AIDS Cases (updated June 30, 2019), 3244 new HIV diagnoses were reported in 2018, corresponding to a rate of 6.94 per 100000 inhabitants without correcting for reporting delays and 8.65 per 100000 inhabitants after correction. Patients aged less than 30 years at the time of HIV diagnosis accounted for 27.7% of cases (n = 898). Men accounted for 85.3% of cases and the median age was 36 years, in agreement with the demographic profile of our series. The highest proportion of cases (83.3%) occurred in men who have sex with men (MSM). This percentage was slightly higher than that reported in the National Registry of HIV and AIDS Cases (56.4%), probably due to the fact that patients in our cohort consulted at an STI unit in our hospital. In Spain, non-Spanish nationals account for 37.6% of new HIV infection diagnoses,3 a slightly higher percentage than that observed in our series.
It is rare for large series of patients to be diagnosed with de novo HIV infection in a dermatology department. Mendes-Bastos et al,4 dermatologists from Lisbon, Portugal, diagnosed 97 de novo cases of HIV infection in 9 years of follow-up, corresponding to almost 11 cases per year. This rate is higher than that reported in our series, possibly because HIV prevalence in Portugal is among the highest in western Europe. In that series, approximately half of the patients were diagnosed with a concomitant STI, compared with two-thirds of patients in our series. It is thought that diagnosis is established earlier and viral loads are lower in cases involving a concomitant STI versus a concomitant non-STI disease4: in the former scenario diagnosis is established based on serological screening, while patients that present with concomitant non-venereal diseases, such as Kaposi sarcoma or bacillary angiomatosis, are usually already in an advanced state of immunosuppression.
Some authors have highlighted the importance of dermatology and venereology in the diagnosis of new HIV cases,4 although to date there are no concrete data available for most regions of the world. It should be borne in mind that many patients who visit the emergency department with a suspected STI do not return for follow-up visits, and therefore may not be informed of their HIV diagnosis. Mendes-Bastos et al estimate that 12% of patients in their series who were diagnosed with de novo HIV infection did not return,4 underscoring the importance of extracting blood samples at the first visit of all patients who present to the emergency department with a STI, even those with condylomata acuminata, and of scheduling follow-up according to the potential HIV window period in cases of infections with a short incubation period, such as gonococcal urethritis. This approach should also be extended to patients with lesions typically associated with HIV or with atypical or exuberant presentations of other diseases (e.g. psoriasis, prurigo nodularis, seborrheic dermatitis, atopic dermatitis, herpetic infections, esophageal candidiasis).
In our experience, dermatologists continue to play an important role in the diagnosis both of STIs and de novo HIV infections, as they are often the first point of contact for these patients within the healthcare system. Furthermore, dermatologists are well positioned to offer and prescribe recently developed pre-exposure prophylactics, applying inclusion criteria that are fulfilled by a large proportion of patients who present at STI units (MSM aged over 18 years who have or have had anal sex without a condom with at least 10 different individuals in the preceding year and at least 1 episode of a bacterial STI in the preceding 12 months).
FundingNo funding was received for this study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Magdaleno-Tapial J, Hernández-Bel P, Valenzuela-Oñate C, Pérez-Ferriols A. Diagnóstico de VIH de novo en un Servicio de Dermatología. Actas Dermosifiliogr. 2021;112:932–934.