The International Day for the Elimination of Violence against Women is celebrated on November 25. In its broadest sense, violence against women includes not only gender violence on the part of a current or former partner, but any form of physical, psychological, sexual, economic, or institutional violence exercised against women or girls on the basis of their gender, constituting a violation of human rights.1 The United Nations has as a goal to end violence against women and girls around the world (UNiTE campaign) by 2030.1
In Spain, gender violence is an important social and health problem. According to data from the Institute for Women and Equal Opportunities of Spain (updated October 22, 2019), a total of 49 cases of fatalities due to gender violence were recorded in that year,2 a number that is even higher if we take into account other victims who were not killed by their current or former partner. Moreover, one in 2 women over the age of 16 reports having been the victim of some type of violence because they are women, and 14.2% have suffered physical and/or sexual violence from a current or past partner at some point in their lives.2
It is therefore not uncommon for us to find patients who suffer or are at risk of suffering this type of violence in our daily practice. In particular, the specialty of dermatology has peculiar characteristics that place professionals in a privileged position to detect such cases,3 as is the case with other forms of abuse such as child or elder abuse.4–7 Skin lesions can be the most visible sign of gender violence, and the dermatologist is the specialist most qualified to identify those that point to abuse and differentiate them from other similar-looking skin pathologies. Bruising, burns, lacerations, traumatic alopecia, or external genital injuries can be indicators of abuse, and can be easily identified by routine dermatologic examination.6
The physical manifestations of Gender violence can be the same as those of other forms of violence, and it should be noted that there are no pathognomonic lesions.8 Minor injuries are more frequent than serious injuries,8 and a high index of suspicion is therefore essential. Some of the injuries that should make us suspect violence against women are listed in Table 1. As in other forms of abuse, one of the main difficulties is to determine whether the skin findings were caused by intentional violence or by accidental trauma.4,7
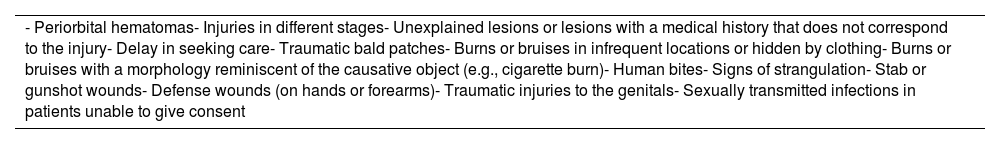
Some of the Injuries That Should Make Us Suspect Gender Violence.
| - Periorbital hematomas- Injuries in different stages- Unexplained lesions or lesions with a medical history that does not correspond to the injury- Delay in seeking care- Traumatic bald patches- Burns or bruises in infrequent locations or hidden by clothing- Burns or bruises with a morphology reminiscent of the causative object (e.g., cigarette burn)- Human bites- Signs of strangulation- Stab or gunshot wounds- Defense wounds (on hands or forearms)- Traumatic injuries to the genitals- Sexually transmitted infections in patients unable to give consent |
The fundamental difference between gender and other types of violence is the victim of the abuse. Girls, pregnant women, the elderly, immigrants, women with physical or mental disabilities, or in other situations of social exclusion (prison, prostitution, poverty) are especially vulnerable to gender violence.8,9
Some of the indicators that may lead us to suspect gender violence are shown in Table 2.8,9 They include data from the medical history, from the physical examination, and on the attitude of the patient and of the man accompanying her. The recognition of risk factors or warning signs is essential so that we can perform a physical examination and a directed history to confirm gender violence.
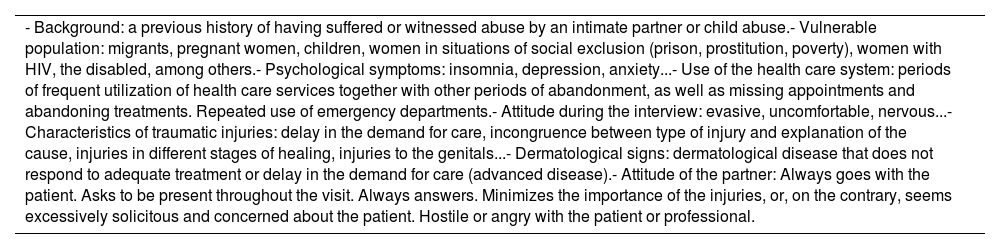
Some Indicators of Suspected Gender Violence.
| - Background: a previous history of having suffered or witnessed abuse by an intimate partner or child abuse.- Vulnerable population: migrants, pregnant women, children, women in situations of social exclusion (prison, prostitution, poverty), women with HIV, the disabled, among others.- Psychological symptoms: insomnia, depression, anxiety...- Use of the health care system: periods of frequent utilization of health care services together with other periods of abandonment, as well as missing appointments and abandoning treatments. Repeated use of emergency departments.- Attitude during the interview: evasive, uncomfortable, nervous...- Characteristics of traumatic injuries: delay in the demand for care, incongruence between type of injury and explanation of the cause, injuries in different stages of healing, injuries to the genitals...- Dermatological signs: dermatological disease that does not respond to adequate treatment or delay in the demand for care (advanced disease).- Attitude of the partner: Always goes with the patient. Asks to be present throughout the visit. Always answers. Minimizes the importance of the injuries, or, on the contrary, seems excessively solicitous and concerned about the patient. Hostile or angry with the patient or professional. |
In our practice, we have encountered different forms of gender violence (as with other forms of abuse5–7) with dermatological consequences, including: 1) dermatological sequelae of physical violence, 2) psychological sequelae that hinder or condition the treatment of an unrelated dermatological pathology, 3) worsening of a chronic dermatological pathology (for example, psoriasis or atopic dermatitis) in the context of the stress experienced by the victims, and 4) consequences of sexual violence.
We present 3 cases from our clinical practice that illustrate this latent social problem.
Patient 1 was a 31-year-old woman who consulted for keloid scars that had been developing over the previous year after she had been stabbed by her former partner (Fig. 1). Some of the scars were in clearly visible locations, such as the neck, the arm, and the exposed part of the chest, and affected the patient's way of dressing and her personal relationships. She was treated with corticosteroid infiltrations and pulsed dye laser, with good aesthetic results and patient satisfaction.
Patient 2 was a 39-year-old woman who presented with basal cell carcinoma of 1cm in diameter in the inner canthus of the eye. She had delayed consultation because she was immersed in a judicial process for gender violence by her former partner. As a result of physical and psychological abuse, she suffered from claustrophobia, agoraphobia, and post-traumatic stress disorder. We encountered several difficulties during the planning and performance of the surgery, as on several occasions the patient presented an anxiety attack, and the procedure had to be suspended. Finally, the surgery was performed under sedation with no further complications.
Patient 3 was an 11-year-old girl who came with her mother to consult for perineal lesions, clinically compatible with condylomata acuminata. In a directed anamnesis the patient denied sexual intercourse or situations of abuse. A shave biopsy performed on one of the lesions confirmed the clinical diagnosis and ruled out high-risk human papillomavirus. Given the high level of suspicion, the case was brought to the attention of the pediatric department and social services, who, on investigation, concluded that it was a case of sexual abuse by a family member, and the minor was moved to safety away from her attacker.
While the pathology for which such patients consult is relatively trivial and common, the clinical management of victims of gender violence is complex. In most cases, we can reduce patient suffering or perhaps even take the first step in detecting the situation and avoid prolonged suffering.
Numerous articles emphasize the role of the dermatologist in detecting elder4–6 or child7–10 abuse or neglect, but there is little mention of gender violence in the dermatological literature.3,8,11
The management of situations of gender violence requires a multidisciplinary approach. As health professionals, it is essential for us to be able to identify and manage such situations in our clinical practice, since for many patients we will be the gateway to the system.
Screening for gender violence takes place mainly in primary care, gynecology, and emergency departments.11 The little training dermatologists receive in this area is really striking.12 A study conducted at a single institution in the United States concluded that most dermatologists were interested in training about domestic violence, but that roughly half of them were unfamiliar with the legal implications.12
In practice, it is advisable to routinely ask all women who come to our clinic about their family situation during the clinical interview, especially if we find any of the warning signs mentioned above. This can be done with a simple question (for example: How are things at home?9) In any event, the question should be asked in plain language, taking care not to judge patients, and in the absence of their partner and children whenever possible. The patient's answers should be included verbatim in her medical record8 and a complete skin scan including the genital area performed. All lesions arousing suspicion of abuse should be documented using body maps or photographs.8
If gender violence is suspected, it is essential that we first understand the complexity of the situation. Our primary concern is to ensure the patient's safety. This can be assessed by using questions such as: Are you afraid to go home? Have there been any homicide or suicide attempts?8... If the patient is safe, our role should be supporting and providing the victim with information and access to resources in a safe way. But if we should witness any act of violence on the part of a current or former partner, such violence is now considered a public crime and can be reported by any person or institution with knowledge of the facts.2
The Government Delegation Against Gender Violence offers a free 24-hour telephone service (016) to provide information and free legal advice. The service can also be accessed by WhatsApp (600 000 016) or email (016-online@igualdad.gob.es). In addition, many of our hospitals offer sensitization courses on the subject, and there are violence commissions where such cases can be reported.
Our intention in this article is to raise awareness of this social problem so widely recognized in other areas, but apparently neglected in the field of dermatology. As a scientific society, it is our duty to make this problem visible and work for gender equality in our environment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.