A 21-year-old woman with no relevant past history and who was only undergoing treatment with oral contraceptives visited our department with a vulvar lesion that had appeared 2 months earlier; the lesion had gradually grown and was causing discomfort on contact with clothing.
Physical ExaminationPhysical examination revealed a pediculated papule in the transition between the clitoris and labia minora; the lesion had a maximum diameter of 0.6cm and was brownish in color with a firm consistency (Fig. 1).
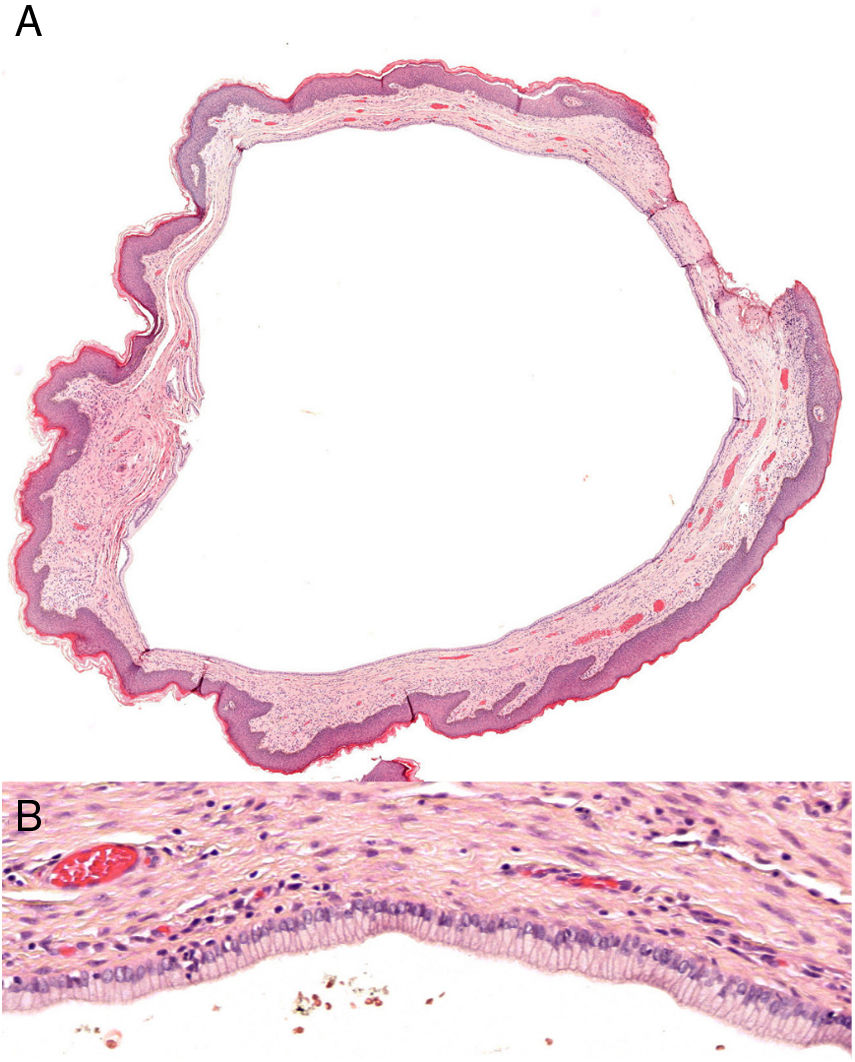
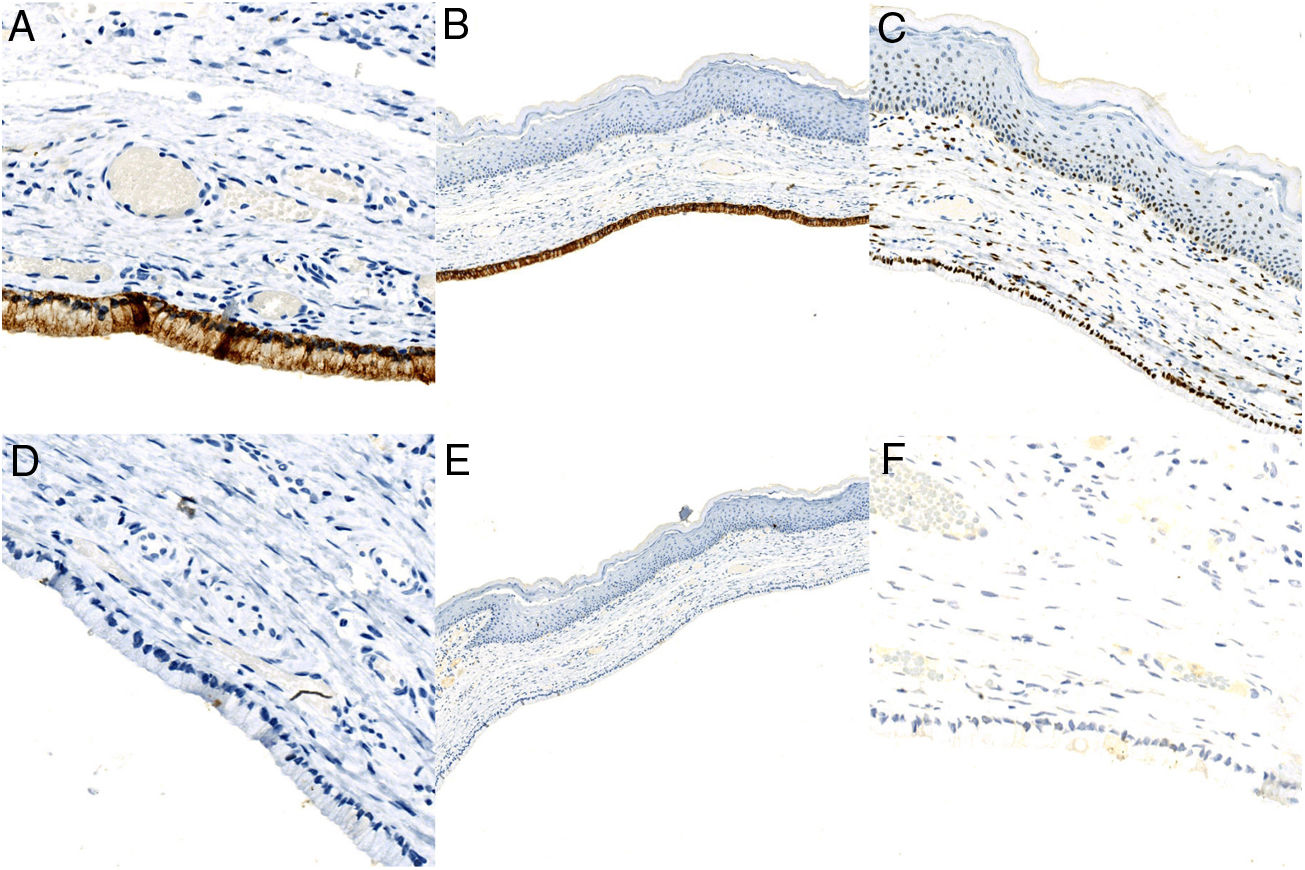
Additional testsSurgical resection of the lesion was performed by shaving of the lesion. Histopathology revealed a well demarcated cystic structure covered with a single layer of columnar cells with a ciliated surface (Fig. 2). Immune staining was positive for epithelial membrane antigen (EMA), estrogen receptor, and cytokeratin 7 (CK7), and negative for progesterone receptor, cytokeratin 20 (CK20), and carcinoembryonic antigen (CEA) (Fig. 3).
DiagnosisCiliated vulvar cyst.
Clinical CourseThe patient has remained asymptomatic and has presented no recurrence of the lesion after 6 months of follow-up.
DiscussionCiliated vulvar cysts (CVC) are a rarely reported entity that normally appears in young women, although it has been reported in women of all ages.1–6 It has been linked to pregnancy and progesterone use, and some authors consider it a variant of the ciliated cutaneous cyst.1–3 The etiology is unknown, although different origins have been suggested: remains of Mullerian ducts (paramesonephric origin), vestiges of the terminal portion of the Wolffian ducts (mesonephric origin), the urogenital sinus, or the sweat glands.2 The most widely accepted theory, however, is Mullerian heterotopia, due to the sequestration and migration of these tissues during embryo development. This theory is based on the histologic and immunohistochemical similarities with the Mullerian epithelium, and other lesions derived from it, such as retroperitoneal Mullerian cysts or transitional cell carcinoma of the fallopian tube.1,2
CVC presents as a solitary lesion of variable size that typically affects the upper portion of the labia minora.1–6 Histopathology reveals a cystic structure demarcated by a single layer of columnar or cuboid ciliated cells. Immune staining is normally positive for EMA, ER, progesterone receptor, and CK7, and negative for S-100, CEA, CK20, and smooth-muscle actin.1,2,5,6 The differential diagnosis includes other vulvar cystic lesions, such as Bartholin’s cyst, papilliferum hidradenoma, cyst of Nuck, inclusion cyst, and vestibular mucinous cyst.2,3 The differential diagnosis with Bartholin’s cysts is of note due to their frequency. These cysts are normally found in the middle-lower portion of the labia minora and may have an acinar origin (nonciliated columnar epithelium) or ductal origin (transitional or squamous epithelium).2
The treatment of choice is surgical.1–6 The lesions may grow and become disfiguring, especially in young girls due to the smaller size of the anatomical structures.1,3,4 No cases of local recurrence after surgery or of malignant transformation have been reported, although follow-up is very limited in the published cases.1–6
In conclusion, we present a new case of CVC, a rare entity with only 20 cases described in the literature to date. We also report the 5th case with an immunohistochemical study, with findings similar to those of the other 4 previously published cases, which support the theory of paramesonephric origin due to remains of Mullerian epithelium. It is important for dermatologists and gynecologists to be aware of this entity, with emphasis on the importance of histopathology and immune staining in vulvar cystic lesions. A greater number of cases and a more extensive study of these lesions are required to determine their true etiology.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ponce S, Montenegro T, Cameselle D. Lesión quística vulvar. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2019.02.029