The rapid spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections soon led to a pandemic with serious health, economic, political, and cultural repercussions across the globe. The disease caused by SARS-CoV-2, coronavirus disease 2019 (COVID-19), is a multisystemic disease that requires a multidisciplinary approach involving specialists from all fields and levels of care. In this article, we review the literature on the diverse cutaneous manifestations associated with COVID-19. We also describe the pathophysiologic mechanisms proposed to date and their possible association with these manifestations. Finally, we propose a system for classifying the cutaneous manifestations of COVID-19 according to their underlying pathophysiologic mechanisms and prognosis.
La infección por SARS-CoV-2 se ha convertido rápidamente en una pandemia con importantes implicaciones en ámbitos sanitarios, económicos, políticos y culturales en todo el planeta. La enfermedad que produce, llamada COVID-19, es considerada actualmente una patología florida y de obligatorio manejo multidisciplinario por todas las especialidades médicas y de servicios de salud.
Este artículo presenta una revisión bibliográfica de las variadas manifestaciones cutáneas a causa de la COVID-19. Posteriormente, se mencionan los diversos engranajes fisiopatológicos que se han postulado hasta el momento y su posible relación con los hallazgos de la enfermedad en la piel. Por último, se propone una clasificación de las manifestaciones cutáneas según mecanismos fisiopatológicos de base y pronóstico de la enfermedad.
In December 2019, the Chinese health authorities reported multiple cases of acute respiratory illness in the province of Wuhan, mostly affecting workers at a small seafood market.1 It was not long before the causative agent was identified: a virus from the Coronaviridae family of likely zoonotic origin and whose original reservoir is the bat.2 Soon afterwards, the virus was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) to distinguish it from the other Coronaviridae viruses responsible for 2 other pandemics this century: SARS-CoV-1 and Middle East Respiratory Syndrome coronavirus (MERS-CoV).3,4
Although SARS-CoV-2 is associated with a case fatality rate of 2.3%,5 lower than that of SARS-CoV-1 (9.5%) and MERS-CoV (34.4%),6 it is highly contagious and quickly spread outside China; its high transmissibility—higher than that of SARS-CoV-17—can be partly explained by the higher viral loads in the respiratory tract. SARS-CoV-2 can also survive in aerosols for more than 3 hours, remains viable on a variety of surfaces for 72 hours, and has a relatively short incubation period (< 2 weeks).8
Early reports of coronavirus disease 2019 (COVID-19), the disease caused by SARS-CoV-2, indicated that most patients experienced fever, rhinorrhea, a cough without expectoration, asthenia, and adynamia.9 A small proportion required hospitalization due to severe pneumonia. In a cohort of 70 000 patients with SARS-CoV-2 infection in China, Wu et al.3 reported that 14% of patients developed severe pneumonia (dyspnea, tachypnea, desaturation, and a decreased arterial oxygen partial pressure to fractional inspired oxygen ratio) and that 5% required critical care. The case fatality rate was 2.3% for the general population and 14% for patients aged 80 years or older. Their findings were corroborated by later reports from Europe.10
The main risk factors for severe COVID-19 include male sex, diabetes, high blood pressure, chronic lung disease, and cardiovascular disease.11,12 Children younger than 10 years have mild symptoms and are much less likely than adults to develop complications or die.13
Reports from Asia, Europe, and the United States have described a wide range of cutaneous manifestations associated with COVID-19. Although these manifestations were initially considered to be nonspecific, the publication of an increasing number of cases revealed an apparent pattern and possibly even an association with prognosis. In this article, we review the literature on the diverse cutaneous manifestations described to date in patients with COVID-19. We then outline the different pathophysiologic mechanisms and hypotheses proposed so far to explain their occurrence.
ResultsCutaneous Manifestations in COVID-19SARS-CoV-2 Infection and Onset of Nonspecific RashesThere are 39 coronavirus species. Seven of these, including SARS-CoV-1, SARS-CoV-2, and MERS-CoV, affect humans.14 The other viruses—HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1—cause mild respiratory conditions such as the common cold. Like other respiratory viruses, many coronaviruses probably also cause viral rashes that go undetected because of the lack of specific testing.
The first report mentioning cutaneous manifestations in patients with COVID-19 was published by Guan et al.15 in February 2020. The authors analyzed data for 1099 patients infected with SARS-CoV-2 and described 2 cases of skin lesions. They did not, however, specify the type of lesions or describe their clinical characteristics or time of onset, probably explaining why this early report was somewhat overlooked. The publication was followed by a report of a patient in Thailand presenting with a “morbilliform rash and multiple petechiae” and a low platelet count who was initially diagnosed with dengue and assigned to outpatient care.16 The patient, however, returned with respiratory symptoms and was diagnosed with SARS-CoV-2 infection by reverse-transcript polymerase chain reaction (PCR). This report alerted physicians to the importance of investigating cutaneous manifestations in patients with COVID-19.17,18
The first large report of cutaneous manifestations in COVID-19 came from a cohort of 88 patients in Italy.19 Of these, 18 (20.4%) had developed cutaneous manifestations: 8 during hospitalization and 10 following discharge. There were 14 cases of “erythematous rash”, 3 of “widespread urticaria”, and 1 of “chickenpox-like vesicles”. The vast majority of patients had trunk lesions, which were largely asymptomatic, resolved spontaneously, and did not appear to be associated with disease severity. Unfortunately, no photographs were taken due to the hospital policies in place at the time of the study.
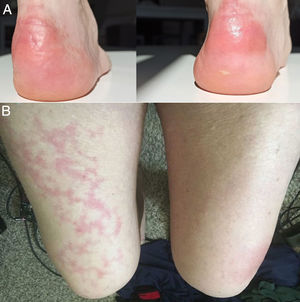
As the days passed, new reports emerged of patients with confirmed SARS-CoV-2 infection and a range of very different cutaneous manifestations, including pruritic erythematous-yellowish plaques on the heels (Fig. 1A),20 a morbilliform rash sparing acral sites,21 a generalized maculopapular morbilliform rash with cephalocaudal progress,22 urticaria-like lesions,23,24 a rash reminiscent of symmetrical drug-related intertriginous flexural exanthema,25 and even livedo reticularis on the lower extremities (Fig. 1B).26 As in the previous cases, biopsies were not performed due to hospital policies and the mild, self-limiting nature of the lesions.
In April, the Journal of the American Academy of Dermatology published a series of 22 patients with COVID-19 who developed a mild varicella-like rash after a median of 3 days from the onset of systemic symptoms; the rash cleared after a median of 8 days, leaving no residual scarring.27 Most of the patients were male (72.7%) and the mean age was 60 years. The varicella-like lesions were predominantly vesicles and were scattered in 72.7% of cases and diffuse in 27.3%. The trunk was affected in all cases. None of the reports mentioned facial or mucosal involvement (Fig. 2A and B). The most common symptom, present in almost half of the patients, was mild pruritus. A skin biopsy performed in 7 patients showed findings consistent with an acute viral infection (Fig. 2C and D). The authors suggested that this type of rash might be a specific manifestation of SARS-CoV-2 infection and as such could be useful for raising suspicion of COVID-19 in patients with mild disease.
A and B, Patients with coronavirus disease 19 (COVID-19) with a papulovesicular rash on the trunk. Note the vesicles with a central varicella-like crust in the photograph on the left (A). C and D, Histopathologic changes in patients with COVID-19 and a varicella-like rash. C, Slightly atrophic epidermis, basket-weave hyperkeratosis, vacuolar degeneration of the basal layer with multinucleated, dyskeratotic hyperchromatic keratinocytes (hematoxylin-eosin, original magnification ×10). D, At higher magnification (hematoxylin-eosin, original magnification ×40), note the vacuolar alteration with disorganized keratinocytes with altered maturation and multinucleated keratinocytes with dyskeratotic cells.
A later publication described the case of a man in the fourth decade of life with PCR-confirmed SARS-CoV-2 infection, fever, and concomitant nonpruritic, annular, circinate, erythematous-edematous fixed plaques on the neck, thorax, abdomen, and upper limbs (symmetric distribution) (Fig. 3A-C).28 The lesions cleared after 7 days. The biopsy findings were consistent with a viral rash (Fig. 3D).
A and B, Erythematous-edematous annular and circinate plaques on the anterior and posterior neck. C, Note the symmetric distribution on the upper limbs. D, Superficial perivascular lymphocytic infiltrate, papillary dermal edema, mild spongiosis, lichenoid and vacuolar interface dermatitis, occasional polymorphonuclear cells in the dermal infiltrate (hematoxylin-eosin, original magnification ×10).
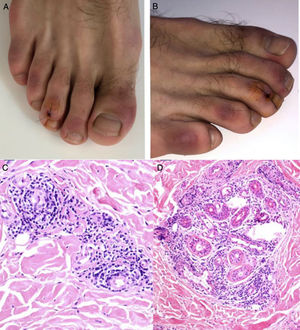
The Chinese group led by Zhang29 published a retrospective review of 7 patients with COVID-19 and pneumonia treated at an intensive care unit in Wuhan. The patients had multiple acro-ischemic manifestations, including acrocyanosis, retiform purpura, and gangrene (Fig. 4). Clinical and laboratory data were evaluated on admission to hospital, at the onset of the cutaneous manifestations, and after the use of anticoagulation therapy. They showed D-dimer, fibrinogen, and fibrinogen degradation product alterations related to the sequential events described. Five of the patients (71.42%) died. This was the first step in the formulation of a hypothesis on the existence of a hypercoagulable state per se in patients with SARS-CoV-2 infection.
Progressive worsening in a patient with coronavirus disease 2019 and acro-ischemic manifestations who developed bullae and finally dry gangrene on his feet.
Around the same time, multiple reports began to emerge from Europe, the Middle East, and the United States of chilblain-like lesions in young people who had been in close contact with a patient with confirmed or probable SARS-CoV-2 infection. The symptoms varied, but the chief complaints were pain and a burning sensation in the skin; the lesions resolved spontaneously and none of the patients developed SARS-CoV-2 pneumonia.30–32
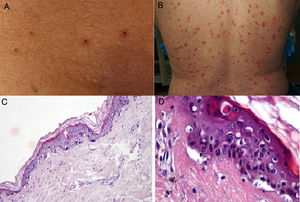
Kolivras et al.33 reported the case of a young man who developed painful, acute-onset, violaceous plaques on the toes and lateral aspect of the feet (Fig. 5A and B) 3 days after the onset of upper respiratory symptoms. A skin biopsy showed findings consistent with chilblain lupus (Fig. 5C and D). The nasopharyngeal swab collected on admission was positive for SARS-CoV-2.
A and B, Hardened violaceous plaques against an erythematous background on the dorsal aspect of the toes and sides of the feet. C and D, Biopsy of lesion on third toe of right foot (hematoxylin-eosin). C, Note the lymphocytic infiltrate with occasional plasma cells in close contact with the vessels and no evidence of fibrin or thrombi (hematoxylin-eosin, original magnification ×40). D, Perieccrine infiltrate (hematoxylin-eosin, original magnification ×40).
In view of the enormous impact of the pandemic on the European continent, numerous groups started to publish studies aimed at characterizing the chilblain-like lesions observed in patients with COVID-19.34 In Italy, Recalcati et al.31 and Tosti et al.35 reported that these lesions were more common in younger patients (especially children [78.5%]), predominantly involved the feet (71% of cases), were self-limiting, and were associated with normal blood tests and an absence of systemic symptoms. A French study of skin lesions observed in 277 patients during 3 weeks of the COVID-19 pandemic found that 142 patients had acral lesions and that 106 of these (75%) were painful erythematous-violaceous edematous macules and papules consistent with chilblain lupus.36 Fernández-Nieto et al37 studied 132 nonhospitalized patients who consulted for acro-ischemic lesions over a period of 5 weeks. The mean age of the patients was 19.9 years; 40.9% had been in close contact with a patient with confirmed SARS-CoV-2 infection and 14.4% tested positive. Over 90% of the lesions affected the fingers or toes, but mostly the toes (81.8%). Similarly to the other cases reported, the patients experienced mild disease.
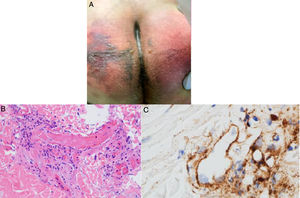
Magro et al.38 reported on patients with COVID-19 who developed cutaneous manifestations consistent with a procoagulant or microangiopathic state. A skin biopsy was performed in 3 patients who developed retiform purpura or livedo racemosa (Fig. 6A) associated with elevated D-dimer levels during the course of their respiratory illness, with findings showing pauci-inflammatory thrombogenic vasculopathy and C5b-9 and C4d deposition (Fig. 6B and C). This observation sparked the hypothesis of a link between mechanisms dependent on the alternative or lectin complement pathways and thrombotic events in patients with SARS-CoV-2 infection, and subsequently provided an explanation for the existence of procoagulant states in other organs.39
A, 32-year-old man with coronavirus disease 2019 who developed retiform purpura on his buttocks 4 days after initiation of mechanical ventilation due to acute respiratory failure. B, Skin biopsy showing extensive pauci-inflammatory vascular thrombosis with endothelial cell injury (hematoxylin-eosin, original magnification ×40). C, C5b-9 deposits in microvessels (diaminobenzidine, original magnification ×40).
The British Journal of Dermatology published the results of a Spanish consensus study of 375 patients with confirmed or suspected SARS-CoV-2 infection who developed cutaneous manifestations without a clear explanation.40 Numerous factors were evaluated over a period of 2 weeks, including clinical manifestations, time of onset in relation to other symptoms, demographics, and associations with disease course and outcomes. The group, led by Galván Casa, divided the manifestations into 5 clinical patterns: 1) pseudo-chilblains (19%), 2) vesicular eruptions (9%), 3) urticarial lesions (19%), 4) maculopapular eruptions (47%), and 5) livedoid or necrotic lesions (6%). They found that livedoid and necrotic lesions affected older patients (mean age, 63 years) with severe disease (mortality rate, 10%), while pseudo-chilblain lesions (acral areas of erythema and edema with vesicles or pustules) were more common after the onset of respiratory symptoms (59% of cases) and occurred in young patients (mean age, 21.8 years) with mild COVID-19. The survival rate of patients with maculopapular eruptions was 98%. The Spanish findings were consistent with reports from other authors, especially in terms of the mild nature of these chilblain-like lesions.30–33
Pathophysiological FindingsPathophysiology of SARS-CoV-2 Infection and Possible Association With Cutaneous ManifestationsLaboratory findings in patients with severe SARS-CoV-2 infection include leukocytosis, neutrophilia, lymphopenia, thrombocytopenia, increased lactate dehydrogenase and procalcitonin levels, and D-dimer and fibrinogen degradation product alterations.41 In some cases, these findings overlap with those observed in disseminated intravascular coagulation syndrome.42 Lippi and Favoro43 reported a directly proportional association between D-dimer levels and severe respiratory illness in patients with SARS-CoV-2 infection, supporting previous reports showing a link between elevated D-dimer levels and mortality in COVID-19.42
In humans, ferritin exerts a protective function during infection by limiting the amount of iron available to numerous pathogens,44 explaining also why ferritin levels increase during inflammatory states.45 Very high ferritin levels have been observed in patients with severe COVID-19 and linked to high morbidity and mortality.46
As mentioned, COVID-19 is characterized by a diverse range of biochemical changes. These changes, however, are reminiscent of findings observed in macrophage activation syndrome47 and highlight the important role of white blood cells, in particular T cells and macrophages, in the exaggerated cytokine and thrombotic immune response associated with COVID-19.
Macrophages and T Cells at the Root of Acro-Ischemic Lesions in COVID-19Preliminary studies characterizing the novel coronavirus identified the angiotensin converting enzyme 2 (ACE2) receptor as the main receptor in SARS-CoV-2 infection.2 SARS-CoV-2 uses the ACE2 receptor to enter human cells and has no affinity for receptors used by other coronavirus families, such as the dipeptidyl peptidase 4 receptor.48
The ACE2 receptor is found on the surface of pulmonary epithelial cells, in enterocytes of the small intestine, in arterial and venous endothelial cells, and in arterial smooth muscle cells in numerous organs, including the skin.49 Viral replication within cells causes direct cell injury, triggering the release of proinflammatory alarmins (direct viral effect). Viral particles can also trigger innate immune responses, including the activation of alveolar macrophages and the complement cascade through the lectin pathway.38,50
Complement activation and diverse immune responses promote the recruitment of leukocytes and an exaggerated proliferation of lymphocytes and massive release of proinflammatory cytokines (interleukin [IL] 1B, IL-6, IL-8), interferon-gamma (IFN-γ), and tumor necrosis factor alpha (TNF-α), among others. IFN-γ, in large quantities, drives macrophage activation and ferritin production,45 IL-6 causes fever,51 and hemophagocytosis causes pancytopenia.47,52 Macrophages also release plasminogen activator, and this is possibly one of the many mechanisms that would explain the thrombotic events and elevated D-dimer levels observed in severe COVID-19.53 It could also explain other findings such as the presence of antiphospholipid antibodies in patients with severe disease in the absence of comorbidities.54 Bowles et al.55 in the United Kingdom and Connel et al.56 in the United States confirmed the presence of antiphospholipid antibodies (especially lupus anticoagulant) in patients with SARS-CoV-2 infection. This might be linked to the observation of acro-ischemic presentations (other than chilblain-like lesions), necrosis, and even livedo reticularis and racemosa in certain patients with COVID-19 and concomitant multisystemic thrombotic responses.
Viral sepsis has also been proposed to explain the systemic and cutaneous changes associated with COVID-19.57 This hypothesis, which came about following multiple reports of multiorgan damage in autopsy studies of patients who had died of severe COVID-19,58 holds that the massive release of cytokines, in particular TNF-α, would promote the death of infected cells via apoptosis-dependent pathways. In addition, SARS-CoV-2 may also be capable of infecting T cells, leading to lymphopenia.
There is sufficient evidence to support direct viral injury to endothelial cells followed by diffuse endothelial inflammation and consequently vascular endothelial apoptosis,59 raising the question of whether COVID-19 may actually be an endothelial disease.60 This theory is supported by reports of death in patients with COVID-19 who had a history of diabetes mellitus or chronic cardiovascular disease and the observation of ischemic cutaneous manifestations, particularly at acral sites.
Association Between IFN and Chilblain-like LesionsPatients with chilblain-like lesions,30–32 apart from being apparently younger, experience mild COVID-19, while those with severe acro-ischemic manifestations, such as gangrene29 and retiform purpura,38 develop more severe disease. The milder forms of disease associated with chilblain-like lesions may be linked to type I IFN.
Kolivras et al.33 highlighted the robust activation of type I IFN in SARS-CoV-2 infection, stating that a similar response was induced in many other acute viral infections.61 Type I IFN levels are elevated in lupus erythematosus and interferonopathies such as Aicardi-Goutières syndrome, which is also characterized by microangiopathic changes at acral sites.62 The authors hypothesized that these changes are the result of early type I IFN responses, which would also explain the mild disease course, as IFN exerts an antiviral effect. In addition, because early type I IFN responses are capable of suppressing the uncontrolled release of diverse proinflammatory cytokines, they would reduce the risk of a cytokine storm. Elderly patients, however, or patients with comorbidities that alter the functioning of the immune system, would generate a delayed type I IFN response, leading to the release of cytokines, macrophage activation syndrome, elevated ferritin and D-dimer levels, true acro-ischemic lesions, and a much worse prognosis.
DiscussionThe COVID-19 pandemic has created enormous challenges for health care professionals, including the need to keep abreast with the vast spectrum of clinical manifestations associated with this disease. COVID-19 is a multisystemic disease that affects multiple organs, including the skin. The occurrence of cutaneous manifestations, however, represents an advantage, as their recognition can lead to early suspicion of disease in some cases and provide clues about individual immune responses or complications in others.
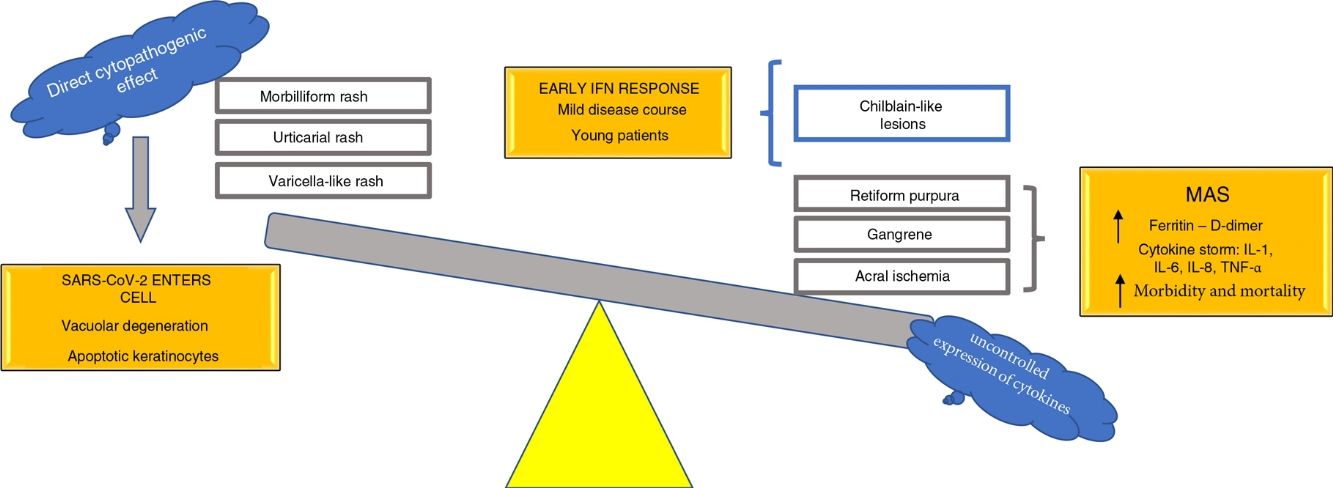
Based on the pathophysiological mechanisms hypothesized, we propose classifying the various cutaneous manifestations of COVID-19 into 2 groups: 1) manifestations primarily linked to a direct cytopathogenic effect on cells such as keratinocytes, which are involved in many known viral infections (morbilliform or urticarial rashes, reactions similar to drug eruptions, varicella-like lesions) and 2) manifestations linked to an uncontrolled release of cytokines due to alterations in specific white blood cells, such as T cells and macrophages. This second group could be divided into a further 2 groups: 1) manifestations characterized by features similar to those seen in macrophage activation syndrome (acral ischemia, gangrene, retiform purple, livedo racemosa) and associated with poor outcomes in terms of morbidity and mortality and 2) cutaneous manifestations with a mild, self-limiting disease course, observed in young patients and linked to the activation of an early type I IFN response (chilblain-like lesions) (Fig. 7). This hypothesis is one of the first in the literature to provide a possible explanation of the pathophysiological mechanisms underlying the main cutaneous manifestations of COVID-19; it also provides a means of classifying these manifestations and establishing their possible prognostic value.
We believe that it is paramount for physicians, nurses, respiratory therapists, health care professionals still in training, and even members of the general population to be aware of the relationship between SARS-CoV-2 infection and the skin and its various manifestations. Heightened awareness will promote an active search for manifestations and a detailed study of cases, adding to the scientific knowledge and our understanding of the pathophysiology of COVID-19 and ultimately contributing to the development of effective treatments and protocols that will mitigate the complications of this infection.
FundingThis study did not receive any specific funding from public sector bodies or commercial or nonprofit entities.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
To all the frontline health care professionals involved in caring for patients with COVID-19; their contribution to the history of medicine is invaluable.
Please cite this article as: González González F, Cortés Correa C, Peñaranda Contreras E. Manifestaciones cutáneas en pacientes con COVID-19: características clínicas y mecanismos fisiopatológicos postulados. Actas Dermosifiliogr. 2021;112:314–323.