Chronic nodular prurigo (CNP) is a chronic dermatological disease characterized by the presence of chronic pruritus and pruritic nodular lesions. The aim of this study was to reach consensus among a group of experts based on a non-systematic literature review and an algorithm for the clinical diagnosis of CNP. The resulting algorithm is structured in 3 blocks: 1) early identification of the patient with a possible diagnosis of CNP; 2) diagnosis and assessment of CNP; and 3) categorization of CNP (identification of the underlying causes or associated comorbidities).
We believe that this clinical algorithm can facilitate the correct diagnosis of patients with CNP. Additionally, it raises awareness on the need for a multidisciplinary approach and specific treatment of CNP, steps of paramount importance to make better therapeutic decisions.
El prurigo crónico nodular (PCN) es una enfermedad dermatológica crónica, caracterizada por la presencia de prurito crónico (PC) y lesiones nodulares pruriginosas cutáneas. El presente trabajo tuvo como objetivo consensuar entre un grupo de expertos, a partir de una revisión bibliográfica no sistemática, un algoritmo para el diagnóstico clínico del PCN. El algoritmo resultante se ha estructurado en tres bloques: 1) identificación precoz del paciente con posible diagnóstico de PCN; 2) diagnóstico y valoración del PCN; y 3) categorización del PCN (identificación de las causas subyacentes o de las comorbilidades asociadas)
Consideramos que este algoritmo clínico puede facilitar el diagnóstico correcto de los pacientes con PCN. Además, genera conciencia de la necesidad de un abordaje multidisciplinar y de un tratamiento específico del PCN, pasos indispensables para tomar mejores decisiones terapéuticas.
Chronic nodular prurigo (CNP) or prurigo nodularis (PN)1,2 is a chronic inflammatory skin disease characterized by lesions with intense pruritus. Although recent transcriptomic studies have characterized CNP as an independent entity, with a predominant Th2 inflammatory response—interleukin-4 (IL-4), IL-13, IL-31—Th17 and Th22 components are also present.3,4 Although the pathophysiology is not fully understood, it has been hypothesized that the pathogenesis of CNP involves changes in the distribution of cutaneous nerve fibers that triggers neuronal sensitization to pruritus.5 The immune system plays a crucial role, as CNP lesions show an infiltrate of eosinophils, T lymphocytes, and mast cells secreting pro-inflammatory cytokines,6–8 and particularly pruritus-inducing mediators such as IL-31 and oncostatin M.9 This neuroimmunological dysfunction triggers an unrelenting itch-scratch cycle, resulting in the appearance of the distinctive pruritic lesions of this disease.10
CNP primarily affects middle-aged adults,11–15 with a slightly higher incidence in women and individuals with higher phototypes.1,10,14,15 CNP is usually associated with other dermatological conditions, such as atopic dermatitis (AD), lichen planus, etc.,14,16 systemic conditions, such as chronic kidney disease (CKD), or diabetes mellitus (DM),1,6,10,12–15,17,18 neurological conditions, such as postherpetic neuralgia, chronic pain, etc., psychiatric disorders,13,15–17 or oncological conditions, such as Hodgkin's disease, GI cancers, etc.14,16 The presence of CNP leads to an impaired quality of life and significantly impacts the activities of daily of living. Sleep disorders, anxiety and depression, and even suicidal ideation are common findings in these patients.1,10,16,18
The diagnosis of CNP is clinical and is based on a thorough history and physical examination. However, there are still differences on what is considered CNP, which complicates diagnosis and the appropriate therapeutic approach for patients.11 The objective of this work was to establish and reach consensus on a clinical algorithm for the correct diagnosis of CNP.
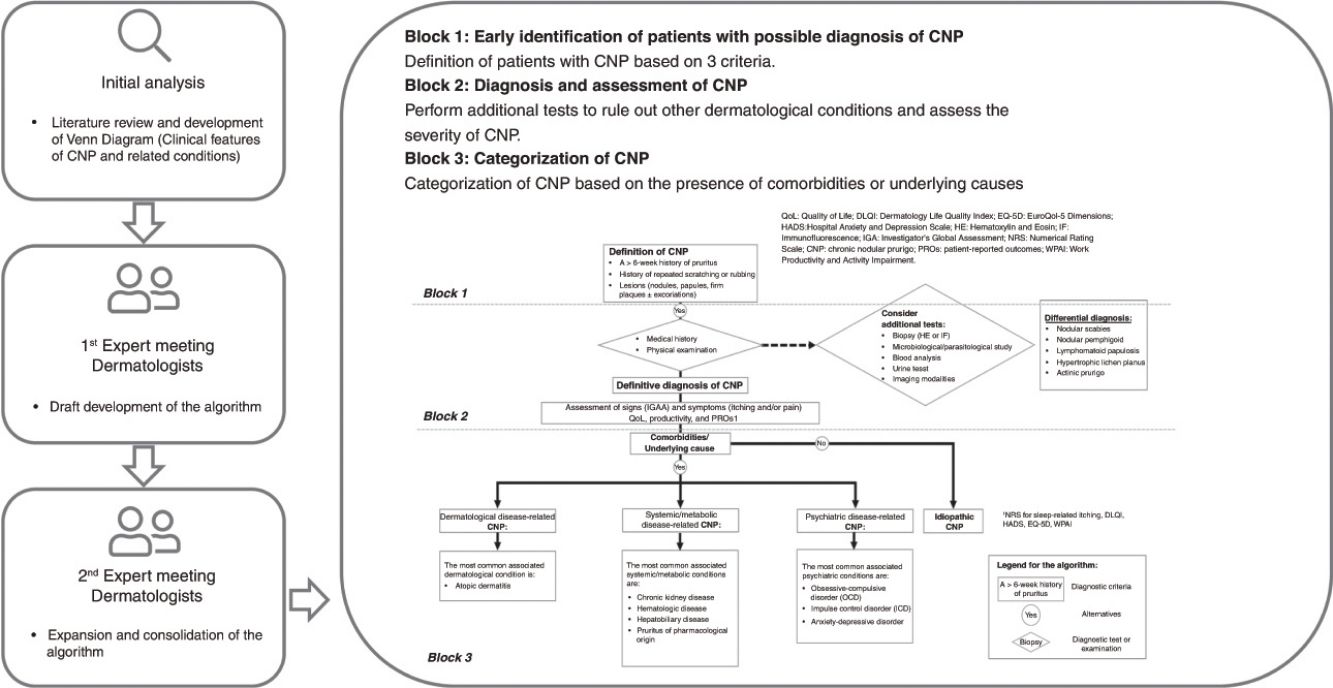
Materials and methodsThis project was carried out from July 2022 through September 2023. The consensus process was conducted through a working group including 9 experts. The project coordinator participated in group selection, allowing for the formation of a group of nationally recognized experts in dermatology. All had a medical specialty in dermatology and venereology, more than 3-5 years of professional experience, demonstrated expertise in the management of CNP patients, and experience as authors of publications or participation in clinical trials in the field of prurigo. In the initial phase, a literature review was conducted to identify the clinical characteristics of CNP and its associated comorbidities.
Subsequently, 2 meetings were held with participation from the experts, during which the clinical approach algorithm for CNP was agreed upon. Finally, the level of consensus among participants was evaluated through an online questionnaire.
Literature reviewWe conducted a literature search to identify reports characterizing the clinical profile of patients with CNP, regardless of whether they were associated with other conditions or not. Clinical features among these patients that could suggest potential criteria for the differential diagnosis of CNP were sought. Key bibliographic sources, such as international guidelines, consensus documents, and reviews, were prioritized. Articles only focused on treatments, validations, biomarkers, populations, or specific situations, and entities unrelated to CNP, were excluded. The search was conducted across PubMed, limited to the last 10 years, and in full compliance with the search criteria detailed in supplementary table 1.
In a later stage, duplicate articles were eliminated, and those that met the above-mentioned criteria were selected after reviewing title and abstract (supplementary figure 1).
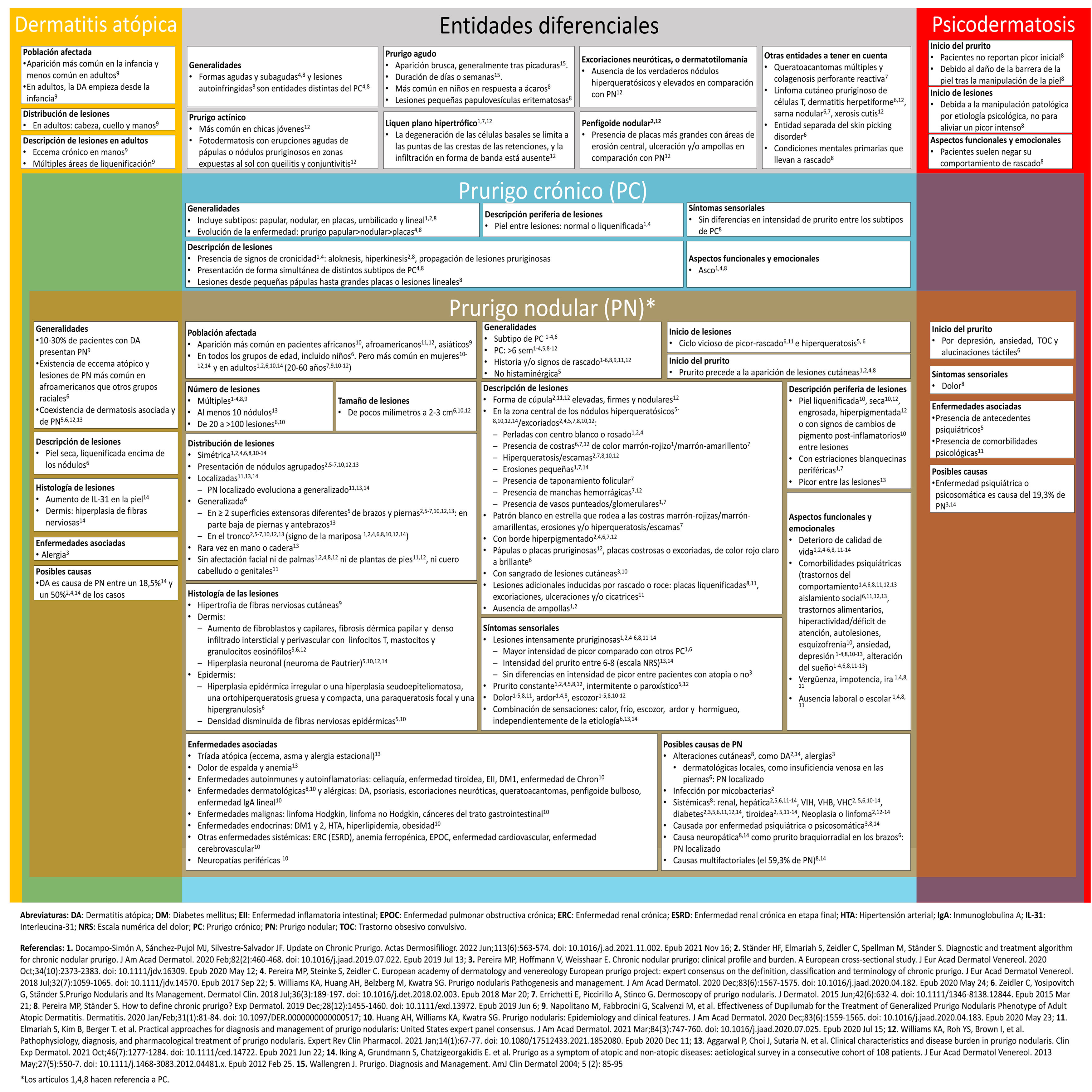
Data mining and classificationFrom the selected bibliography, specific clinical characteristics of PN were drawn, as well as those shared with chronic pruritus (CP), AD, psychodermatoses, and other related entities. These clinical features were graphically organized in a modified Venn diagram (supplementary figure 2), which provided the initial starting point for subsequent discussions and the development of the algorithm.
Expert meetings and consensusIn the first meeting, an initial consensus was reached to define CNP based on the clinical characteristics described in the literature. This consensus allowed the development of a draft algorithm, which was later expanded and consolidated in a second meeting. Finally, the level of consensus among participants on various aspects of the algorithm was assessed through an online questionnaire.
ResultsA total of 245 reports were identified in the initial search. After the process of duplicate elimination and screening, a total of 14 reports were selected.1,2,6,10–12,14–21
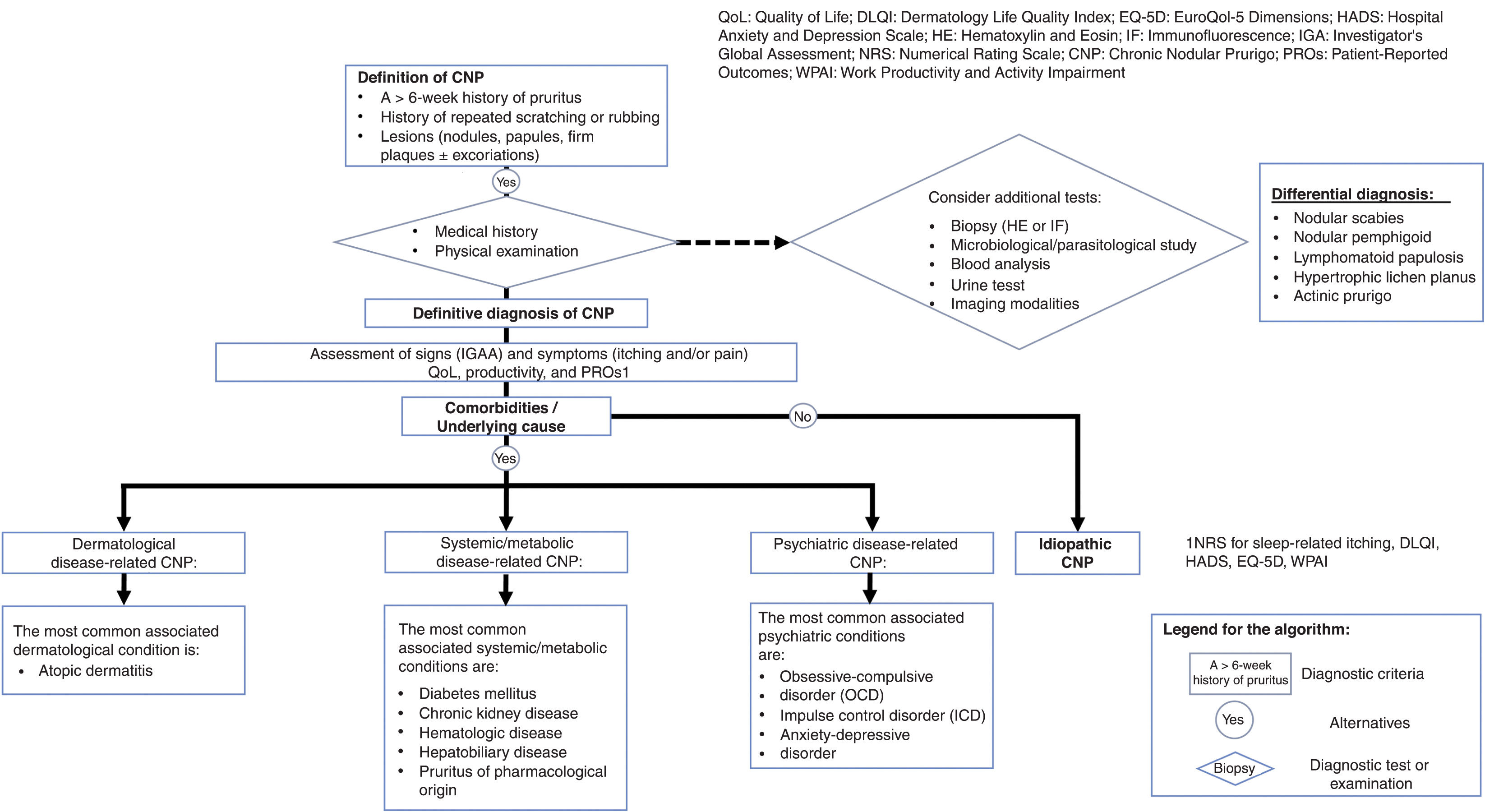
Figure 1 shows the algorithm resulting from the consensus reached, which was structured into 3 blocks: 1) early identification of patients with possible CNP diagnosis; 2) diagnosis and assessment of CNP; and 3) categorization of CNP (identification of underlying causes or associated comorbidities).
The following topics were debated by the expert panel.
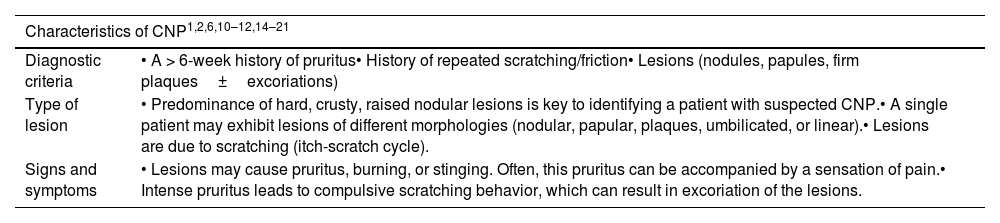
Block 1: early identification of patients with possible chronic nodular prurigoBased on the analysis of the Venn diagram, specific characteristics of patients with CNP were identified (Table 1), which were prioritized in terms of clinical relevance and frequency. Based on this, CNP was defined as the presence of chronic pruritus (a >6-week history of chronic pruritus) leading to compulsive scratching behavior and the presence of predominantly nodular pruritic lesions, with possible coexistence of other lesions with different morphologies, such as firm plaques, papules, umbilicated or linear lesions. Consensus was reached that the appearance of these lesions is due to an itch-scratch cycle.
Characteristics of patients with CNP.
| Characteristics of CNP1,2,6,10–12,14–21 | |
|---|---|
| Diagnostic criteria | • A > 6-week history of pruritus• History of repeated scratching/friction• Lesions (nodules, papules, firm plaques±excoriations) |
| Type of lesion | • Predominance of hard, crusty, raised nodular lesions is key to identifying a patient with suspected CNP.• A single patient may exhibit lesions of different morphologies (nodular, papular, plaques, umbilicated, or linear).• Lesions are due to scratching (itch-scratch cycle). |
| Signs and symptoms | • Lesions may cause pruritus, burning, or stinging. Often, this pruritus can be accompanied by a sensation of pain.• Intense pruritus leads to compulsive scratching behavior, which can result in excoriation of the lesions. |
CNP, chronic nodular prurigo.
Once the 3 diagnostic criteria for CNP are confirmed, a history and physical examination of the patient should be conducted. These evaluations will determine the need for additional tests, such as microbiological/parasitological tests, blood count/urinalysis, imaging modalities, or biopsies. In the case of a biopsy, the detection of hypertrophy of cutaneous nerve fibers can aid in the diagnosis of CNP. These guidelines are primarily aimed at facilitating a differential diagnosis of CNP that rules out other dermatological diseases that may exhibit similar clinical features.
It was agreed that the differential diagnosis should primarily be established against the following conditions: nodular scabies, nodular pemphigoid, lymphomatoid papulosis, hypertrophic lichen planus, actinic prurigo, and leishmaniasis.
Once the diagnosis of CNP is confirmed, its severity should be evaluated too. To do this, it is important to quantify the number of lesions (Investigator Global Assessment [IGA] scale) and the intensity of symptoms (pruritus and pain). Simultaneously, it is recommended to assess the impact of the lesions on the patients’ quality of life and social-occupational activity. For this purpose, several patient-reported outcome (PRO) scales were recommended: numerical rating scale (NRS) for pruritus, NRS for sleep, Dermatology Life Quality Index (DLQI), Hospital Anxiety and Depression Scale (HADS), EuroQoL 5 dimensions (EQ-5D), the Work Productivity and Activity Impairment (WPAI) scale, or Barratt Impulsiveness Scale (rarely used outside psychodermatology).
Block 3: categorization of chronic nodular prurigoAfter evaluating CNP, it is necessary to search for its underlying cause, if any, or the associated comorbidities that patients may exhibit. Patients were categorized based on the presence of comorbidities or underlying causes into 4 groups: 1) dermatological disease-related CNP, 2) systemic/metabolic disease-related CNP, 3) psychiatric disease-related CNP, or 4) idiopathic CNP.
Idiopathic CNP, understood as CNP with prurigo lesions without any association with a different disease, represents a very small percentage of confirmed CNP diagnoses.
In most cases, CNP coexists with other diseases, especially AD (and less frequently with psoriasis, lichen planus, or hypertrophic lupus). In addition, various systemic or metabolic diseases, such as DM, CKD, various hematological disorders, hepatobiliary disorders, or iatrogenic pruritus, can predispose to the development of CNP. In the field of psychiatric disorders, obsessive-compulsive disorders (OCD), impulse control disorders (ICD), and anxiety-depressive disorders were considered more common associated with CNP (Fig. 1).
DiscussionThe clinical algorithm developed facilitates the accurate diagnosis of patients with CNP, determines its possible etiology, and categorizes it—an essential step in guiding therapeutic decisions. Such algorithm provides a holistic view of CNP including all its associated diseases.
The heterogeneity in the clinical presentation of CNP has triggered debate about its definition, which explains, at least partially, its underdiagnosis in clinical practice. Currently, CNP is recognized as an independent entity3,4 characterized by the presence of chronic pruritus and numerous localized or generalized pruritic lesions.11 In this regard, the 2019 European consensus of the pruritus working group of the European Academy of Dermatology and Venereology (EADV) concluded that CP must be clearly distinguished from other diseases, such as “acute prurigo” or “subacute prurigo,” as well as from psychogenic self-inflicted skin lesions, which respond to different diagnostic criteria. The term CP is used to describe a series of similar signs, although different primary lesions may predominate in its clinical presentation.2 From a practical standpoint, and given the existing controversy, the terms CP and PN can be considered synonymous, as both the diagnostic and therapeutic approaches are the same.
In line with the diagnostic criteria for CNP described in the European consensus,2 which defines CNP by the presence of primary symptoms and a range of clinical signs, the algorithm establishes 3 basic criteria for diagnosing CNP: 1) a >6-week history pruritus, 2) a history of repeated scratching/friction, and 3) presence of skin lesions due to scratching, such as nodules, papules, firm plaques with or without excoriations.
The algorithm takes into consideration the heterogeneity, size, and distribution of the lesions to correctly diagnose patients with CNP. Although the nodule is the most distinctive lesion of CNP, it can present with other lesions, such as papules—umbilicated or linear lesions—along with crusts or excoriations due to persistent pruritus and scratching. Furthermore, since lesions do not always remain static and may progress over time,2,16 it is common to see mixed lesions11,12,16 of a “papulonodular” type. The presence of white scars with peripheral hyperpigmentation6 can also provide additional guidance for diagnosing CNP in patients who do not exhibit nodules during their examination. Regarding lesion size, some authors have established a minimum diameter of 1cm as a cutoff point.6,13,14 However, other experts accept smaller lesions if they are abundant,2,11,12,16,17,21 thereby including a broader spectrum of people affected by CNP in clinical practice. Regarding lesion distribution, although most patients exhibit a symmetrical pattern on their upper and lower limbs, this is not a definitive trait for identifying someone with CNP. Less common locations, such as the facial area, genital area, palms of the hands, or soles of the feet, have also been reported.1,6,8,11,12,16
When CNP is suspected, it is crucial to perform a differential diagnosis to rule out other dermatological diseases with similar clinical signs, such as nodular scabies,22 nodular pemphigoid,11,12 lymphomatoid papulosis,10,13 hypertrophic lichen planus,10,11,20 actinic prurigo,10 and, less frequently, leishmaniasis.23
For the clinical evaluation of signs and symptoms, it is necessary to determine the severity of the lesions by considering the number of lesions, the intensity of pruritus (or intolerance to friction), and the impact on quality of life. In this context, the IGA scale categorizes the severity of CNP based on the number of lesions and presence of excoriations into 5 grades (clearance, almost clear, mild, moderate, and severe). However, this scale is not validated in Spanish and is more widely used in clinical research settings than in the routine clinical practice.12 CNP also negatively affects the patients’ psychosocial well-being and self-esteem.19 According to a global burden of disease study, CNP ranks among the top 50 diseases with the greatest impact on quality of life worldwide.24 It has been reported that the health-related quality of life of people with CNP is even lower than that of individuals with a history of stroke.25
Regarding the categorization of CNP, part of the medical community identifies idiopathic CNP as the only possible profile. However, during this consensus, experts agreed that this category of CNP is uncommon.11,14–16 In most cases, CNP coexists with other conditions.2,6,8,10,12,14–18 Indeed, recent observations show that only 10.8% of patients with CNP have zero comorbidities, and nearly half exhibit 3 or more comorbidities. The most common skin disease was AD while 24%, and 27% had anxiety as the most common psychiatric disorder.26 Nonetheless, it is essential to accurately differentiate between causal and reactive conditions. Some comorbidities, such as psychiatric disorders, may act as predisposing or triggering factors for CNP, while others may be just a consequence of scratching.1,2,6,11,12,14–18 Therefore, it is important to consider the multifactorial nature of CNP in most cases2,15,16 and treat CNP even when the underlying cause has been resolved.
Finally, it is important to mention the limitations of this work: 1) the lack of consensus on the definition of CNP may have resulted in heterogeneous characteristics; 2) the relationship between CNP and its comorbidities can be complex and is not fully understood, meaning that interpreting whether a disease is the cause or consequence of CNP can vary greatly; 3) the limited number of participants may affect the applicability of this algorithm, so it is recommended to reinforce this consensus in a larger group of experts using the Delphi method; and 4) the limited availability of studies and the lack of national consensus have prevented the inclusion of evidence levels and grades of recommendation. Nevertheless, this algorithm may be useful in guiding the diagnosis of people with CNP and contribute to establishing specific and effective treatment.
ConclusionsThe developed algorithm provides a new perspective on CNP that can facilitate the diagnosis of patients in a clinical setting where, to this date, no consensus had ever been reached.
The initial diagnosis of CNP should be based on 3 criteria: a >6-week history of pruritus, a history of repeated scratching/friction, and skin lesions, such as nodules, papules, firm plaques with or without excoriations.
The etiology of CNP is often multifactorial, with most patients exhibiting associated comorbidities. Health care professionals must be aware of the need for a multidisciplinary approach and the importance of specifically treating CNP, even if the underlying cause has been resolved.
For a deeper understanding of CNP pathogenesis and its relationship with other diseases, it is necessary to undertake registries, epidemiological studies, and real-life studies to expand and correlate evidence in this field. Advances in the clinical characterization of CNP represent a reality that would improve the quality of care these patients receive.
Conflicts of interestJavier Ortiz de Frutos: has collaborated as an advisor for Leo Pharma, Galderma, Novartis, Astellas Pharma, Uriach, Sanofi, GSK, Pfizer, AbbVie, Lilly, and Almirall; has given paid lectures for Leo Pharma, BDF, Astellas, Novartis, MSD, Sanofi, and AbbVie; participated in clinical trials for Astellas, Novartis, Bayer, Sanofi, Leo Pharma, Lilly, Pfizer, and AbbVie; and received conference grants from ISDIN, Grupo Menarini, Astellas, Novartis, MSD, Sanofi, LETI Pharma, Leo Pharma, and AbbVie.
Esther Serra Baldrich: has collaborated as an advisor or speaker for Sanofi, AbbVie, Leo Pharma, Pfizer, Lilly, Galderma, and Pierre Fabre.
Juan Francisco Silvestre: has collaborated as a speaker, advisor, and/or researcher for AbbVie, Almirall, Amgen, AstraZeneca, Bristol Myers Squibb, Eli Lilly, Galderma, Incyte, Leo Pharma, Novartis, Pfizer, Regeneron, and Sanofi Genzyme.
María José Tribó Boixareu: has collaborated as an advisor for Galderma.
José Carlos Armario Hita: has received funding to attend meetings and conferences, speaking fees, and funding to participate in research from Sanofi, AbbVie, Lilly, Novartis, Galderma, Pfizer, UCB Pharma, Janssen, and Leo Pharma.
José Manuel Carrascosa Carrillo: has collaborated as an advisor for Galderma and participated as the principal investigator in clinical trials for Galderma and Sanofi.