A 12-month-old boy with no drug allergies or past medical history of interest was seen for a congenital umbilical lesion that was stable in size and presented no history of bleeding or discharge and no associated systemic manifestations. The patient had been treated on one occasion by his pediatrician with silver nitrate cauterization, but the lesion persisted.
Physical ExaminationPhysical examination revealed a shiny, erythematous umbilical papule with a smooth surface, measuring 1cm in diameter. The adjacent skin was normal (Fig. 1).
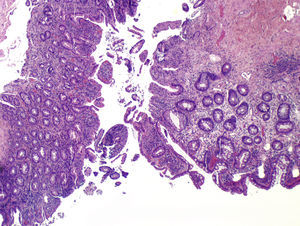
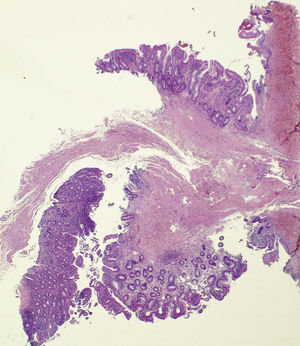
HistopathologyHistologic examination revealed a raised lesion with a polyploid morphology (Fig. 2). Higher magnification revealed a focal coating composed of multilayered keratinized epidermal-type epithelium, in transition with gastrointestinal mucosa (Fig. 3), with superficial erosions and a moderate inflammatory infiltrate in the lamina propria.
What Is Your Diagnosis?
DiagnosisUmbilical polyp (persistence of the omphalomesenteric duct [OMD]).
Clinical Course and TreatmentSurgical removal and intraoperative examination of the base of the polyp were performed. No other abnormalities were observed. The patient was examined by the pediatric gastrointestinal unit. Soft-tissue ultrasound detected no involvement of deeper tissue layers and scintigraphy using 99mTc-pertechnetate was negative for ectopic gastric mucosa.
CommentThe OMD is the structure that connects the embryonic midgut to the yolk sac to provide nourishment for the embryo while the placenta develops during the first weeks of intrauterine life. Under normal conditions, the OMD should obliterate between the fifth and ninth week of development and should have disappeared completely by the time of birth. In 2% of the population, involution is incomplete,1 resulting in various remnants, such as Meckel's diverticulum (the most common form), fistula between the ileum and the umbilicus, umbilical sinus, an omphalomesenteric duct cyst, an umbilical polyp, and a fibrous cord running from the ileum to the umbilicus. These conditions are asymptomatic in 50% of cases; in other cases, they manifest as bowel obstruction (36%), acute abdomen (31%), persistent umbilical mass and/or secretion (29%), or rectal bleeding (5%)1 during the neonatal period, early childhood, or, less frequently, in adulthood.2
Umbilical polyp is a rare entity resulting from the protrusion of the mucosa of the OMD through the navel. It is identified from birth as a bright red papule or nodule with a smooth surface, possibly with bleeding and/or serous or serosanguinous discharge, which can irritate the surrounding skin. Histologic examination generally shows an eroded epidermis contiguous with digestive tract mucosa, usually (in order of frequency) the small bowel mucosa, gastric mucosa, large bowel mucosa, and pancreatic tissue.3,4
The main differential diagnosis is umbilical granuloma, which is also a bright red papular-nodular lesion, but with a more friable surface formed by excess granulation after the detatchment of the umbilical cord. Umbilical granuloma responds to silver nitrate cauterization.5 Entities that manifest as masses or umbilical secretion—such as persistent urachus, capillary hemangioma (and other vascular neoplasms), umbilical hernia, omphalocele, and gastroschisis—should also be considered.3,6
Simple surgical excision is the treatment of choice. Given the reports of cases associated with other forms of persistence of the OMD, the question of whether additional tests should be performed systematically has been a subject of debate. The most recent studies recommend that a thorough intraoperative examination of the base of the polyp should be carried out and that additional tests should only be ordered when the intraoperative examination yields abnormal findings.4
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr. Itziar Eraña Tomás for the histologic images.
Please cite this article as: Pérez-Mesonero R, Melgar-Molero V, Martín-Fuentes A. Nódulo umbilical congénito en paciente de un año. Actas Dermosifiliogr. 2017;108:466–467.