Epidermodysplasia verruciformis (EV) is an autosomal recessive genodermatosis characterized by high susceptibility to β human papillomaviruses (HPV).1 Characteristic clinical manifestations include polymorphic pityriasis versicolor–like lesions and verruca plana–like papules. Both appear in childhood and have malignant potential, with 30% to 70% of patients developing a malignancy in adulthood.2,3 EV-like is an acquired form of EV that occur in patients with acquired cell-mediated immunity defects.1
We reviewed medical records and available images for all patients with histologically confirmed EV and EV-like at Hospital Universitari Arnau de Vilanova, in Lleida, Spain. Seven patients were studied. Their characteristics are summarized in Table 1 and illustrated in Fig. 1.
Characteristics of Patients With EV and EV-Like Lesions.
| EV/EV-like lesions | Sex | Age at symptom onset, y | History of EV | Skin type | Skin lesions | Comorbidities | NMSC during follow-up | |
|---|---|---|---|---|---|---|---|---|
| 1 | EV | F | 12 | Yes (mother) | 2 | Erythematous scaling maculopapular rash on the trunk and top of the upper and lower limbs. Filiform warts on both shoulders. Flat warts on the dorsum of the hands and top of the limbs. Plantar keratoderma. | Hypertension | Yes (SCC on lower limb) |
| 2 | EV | M | 8 | No | 5 | Hypopigmented maculopapular lesions located predominantly on the trunk and in the cervical region. Cervical seborrheic keratosis–like lesions and flat warts on the dorsum of the hand. | No | No |
| 3 | EV-like | F | 24 | No | 4 | Hypopigmented maculopapular lesions located bilaterally in the lower abdominal and inguinal region. Seborrheic keratosis–like lesions in the bilateral inguinal region. | HIV, CIN-I | No |
| 4 | EV-like | F | 31 | No | 2 | Hypopigmented maculopapular lesions located predominantly on the upper trunk and top of the limbs. Flat warts on the dorsum of the hand. | HIV, HBC, HVC, CIN-III | No |
| 5 | EV-like | M | 40 | No | 3 | Confluent, salmon-colored papular lesions, some with central umbilication, in the upper region of the trunk. Flat warts on the dorsum of the hand. | HIV | No |
| 6 | EV-like | M | 40 | No | 2 | Hypopigmented maculopapular lesions in the right neck region. Filiform wart on the forehead. Common wart on the tip of the fourth finger of the left hand. | NHL, autologous bone marrow transplant, lung transplant, polychemotherapy, splenectomy, treatment with tacrolimus and methylprednisolone | Yes (oral SCC) |
| 7 | EV-like | M | 42 | No | 2 | Hypopigmented maculopapular lesions measuring 3 to 4mm in the perianal area, the inner aspect of the labia majora, and the vulva. Pink maculopapular lesions on the pubis and inner thighs. | HIV, HVC, CIN-I | No |
Abbreviations: CIN, cervical intraepithelial neoplasia; EV, epidermodysplasia verruciformis; F, female; HBV, hepatitis B virus; HCV, hepatitis C virus; IHC, immunohistochemistry; M, male; NMSC, nonmelanoma skin cancer; NHL, non-Hodgkin lymphoma.
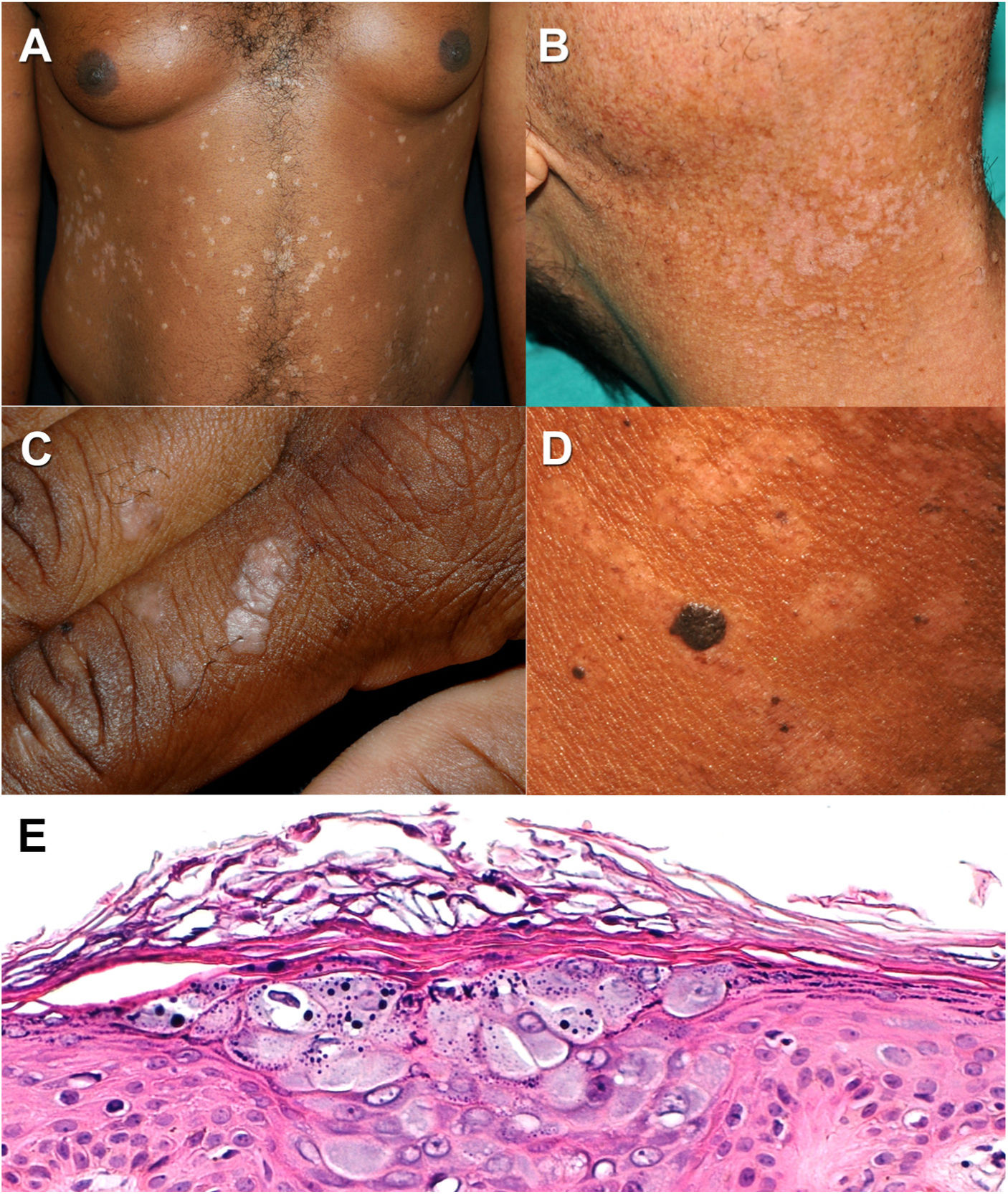
Epidermodysplasia verruciformis. A and B, Pityriasis versicolor-like hypopigmented macules in 2 patients with a low and high Fitzpatrick skin type. C, Verruca plana-like lesions on the dorsum of the hand. D, Seborrheic keratosis-like lesions and hypopigmented pityriasis versicolor-like macules in a patient with a high Fitzpatrick skin type. E, Characteristic histology findings in epidermodysplasia verruciformis. Note the thickened keratinocytes with grayish-blue cytoplasm in the stratum spinosum and keratohyaline granules in the interior (hematoxylin–eosin, original magnification ×20).
EV is an inherited genetic condition characterized by abnormal susceptibility to β HPV types,1 mostly HPV-5 and HPV-8, but others have been identified.1 Merkel cell polyomavirus DNA has also been found in patients with EV and EV-like lesions.1 Classic EV is inherited in an autosomal recessive manner due to homozygous inactivating mutations in the EVER1/TMC6 and EVER2/TMC8 genes located on chromosome 17q25.1 These genes are expressed in keratinocytes and immune cells encoding proteins that regulate intracellular zinc. The proteins are involved in the induction of proapoptotic factors and inhibit the transcription of HPV4 genes.4 A nonclassic form of EV associated with RHOH, MST-1, and CORO1A was recently described.1,5 EV-like is an an acquired form of EV that occur in predisposed patients with cell-mediated immunity defects. The main immunosuppressive factor is HIV infection.1 In our series, 4 of the 5 patients with EV-like had HIV infection. “The main clinical manifestations of both EV and EV-like lesions are pink, scaling, hypopigmented” or hyperpigmented pityriasis versicolor–like macules and erythematous or whitish verruca plana–like papules.1 All 7 patients in our series had pityriasis versicolor–like lesions and 4 had verruca plana–like lesions (Fig. 1A–C). These findings are consistent with those of the series described by Lutzner et al.,6 where all the patients had pityriasis versicolor–like lesions and many had verruca plana–like lesions. Pigmented, hyperkeratotic seborrheic keratosis–like papules have also been described in EV, mainly in black patients and patients with phenotypes associated with a worse prognosis.1 Patients #2 (EV) and #3 (EV-like) in our series, both with a high Fitzpatrick skin type, developed seborrheic keratosis–like lesions (Fig. 1D). Lesions are usually disseminated in EV, although there have been reports of localized eruptions.7 The 2 patients with EV in our series had disseminated lesions, and 4 of the 5 patients with an EV-like eruption had localized lesions. EV and EV-like are associated with increased susceptibility to nonmelanoma skin cancer (NMSC). Two patients in our series developed NMSC. Patient #1 developed cutaneous squamous cell carcinoma (SCC), while patient #6 developed SCC in the oral mucosa (a sun-protected area). It is worth noting that the latter patient only developed pityriasis versicolor–like lesions in the mandibular region, which had previously been treated with radiation therapy. Risk of NMSC is also influenced by HPV type. Types HPV-5, HPV-8, HPV-10, and HPV-47 have been identified in more than 90% of EV-associated malignancies.8 Sun exposure is the main risk factor for NMSC in patients with EV and EV-like lesions. Patients with high Fitzpatrick skin types may be more likely to have a benign course due to the UV protection conferred by increased pigmentation.3 The patient who developed cutaneous SCC in our series had a low Fitzpatrick skin type. Those with higher types (patients #2 and #3) did not develop any malignancies during follow-up. Diagnosis of EV and EV-like lesions is clinical and usually confirmed histologically. Typical histologic findings in EV are hyperkeratosis, epidermal acanthosis with keratinocytes with a bluish cytoplasm and keratohyaline granules, and cytologic atypia (Fig. 1E).1 Dermoscopy was recently described as a useful diagnostic tool for EV.9 Management of EV and EV-like consists of regular dermatology check-ups and strict sun protection measures to prevent NMSC. Although there are no specific treatments for EV, it has been suggested that systemic retinoids might be useful prophylactics for high-risk patients due to their antiproliferative and differentiation-inducing effects.10
Dermatologists must be familiar with the clinical presentation of congenital and acquired EV. Early diagnosis and initiation of preventive measures are key to prognosis and management.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We would like to thank Dr. Joan Àngel Baldo and Dr. Manel Baradad for their contributions and help in compiling the cases.