The umbilicus is known to receive metastatic malignancy from diverse visceral organs. Accurate and correct diagnosis of umbilical lesions is imperative since metastatic malignancy signifies a serious underlying situation with dire prognosis. Identification of demographic features that can contribute to diagnostic resolution of umbilical lesions is desirable. We analyzed umbilical biopsies received over a 20-year period to determine any gender distinctive attributes of umbilical nodules.
Materials and methodAll umbilical biopsies received in our department from 1st January 2000 to 31st December 2019 were identified and analyzed. Data acquired included patient's gender, age, date of biopsy, type of biopsy and histopathological diagnoses and these were analyzed using computer software.
ResultsThere were 67 umbilical biopsies from 22 males and 45 females giving a male: female ratio of 1:2. The difference between the mean age (SD) of male patients [47.8 years (19.4 years)] and that of the females [42.8 years (13.9 years)] was not statistically significant (p=0.28). Twenty-five of the 67 umbilical lesions were benign while 42 were malignant. About 90.9% of biopsies in males were malignant and 9.1% benign while 48.9% of biopsies in females were malignant and 51.1% benign. The odds of malignant umbilical biopsy in males compared to females is 10.5 [OR=10.5; 95% CI=2.2–50.1)].
ConclusionUmbilical biopsies were relatively infrequent in our practice and were more common in females than males. Umbilical lesions presented by males are mostly malignant. Overall, 78% of all umbilical lesions in females were of gynecological derivation.
Se sabe que en el ombligo se presentan metástasis de neoplasias de diversos órganos viscerales. Es imperativo el diagnóstico preciso y correcto de las lesiones umbilicales, ya que la caracterización metastásica implica una situación subyacente grave con un pronóstico nefasto. Es deseable la identificación de las características demográficas que pueden contribuir a la resolución diagnóstica de las lesiones umbilicales. Analizamos las biopsias umbilicales recibidas durante un período de 20 años para determinar los atributos distintivos de género de los nódulos umbilicales.
Material y métodoSe identificaron y analizaron todas las biopsias umbilicales recibidas en nuestro departamento desde el 1 de enero de 2000 hasta el 31 de diciembre de 2019. Los datos adquiridos incluyeron el sexo del paciente, la edad, la fecha de la biopsia, el tipo de biopsia y los diagnósticos histopatológicos y se analizaron mediante un software informático.
ResultadosHubo 67 biopsias umbilicales de 22 hombres y 45 mujeres dando una relación hombre: mujer de 1:2. La diferencia entre la edad media (DE) de los hombres [47,8 años (19,4 años)] y la de las mujeres [42,8 años (13,9 años)] no fue estadísticamente significativa (P=0,28). Veinticinco de las 67 lesiones umbilicales fueron benignas mientras que 42 fueron malignas. El 90,9% de las biopsias en hombres fueron malignas y el 9,1% benignas, mientras que el 48,9% de las biopsias en mujeres fueron malignas y el 51,1% benignas. El riesgo de que una biopsia umbilical fuera maligna en hombres en comparación con mujeres fue de 10,5 [RP=10,5; IC del 95%=2,2 a 50,1)].
ConclusiónLas biopsias umbilicales fueron relativamente poco frecuentes en nuestra práctica y fueron más comunes en mujeres que en hombres. Las lesiones umbilicales que presentan los varones son en su mayoría malignas. En general, el 78% de todas las lesiones umbilicales en mujeres fueron de derivación ginecológica.
The umbilicus is a depressed scar that immortalizes the site of prenatal attachment of baby to the mother. It is situated at the center of the anterior abdominal wall level with the highest point of the iliac crest and opposite the 4th lumbar or opposite the disk between the 3rd and 4th lumbar vertebrae.1 The mean (SD) height and width of the umbilicus in the non-obese subjects have been reported to be 2.1cm (0.6cm) and 2.3cm (0.7cm) respectively.2
The umbilicus occasionally becomes a focus of clinical attention, as a variety of conditions are known to affect it. By far the most prevalent neoplastic lesion of the umbilicus is metastatic carcinoma. Eponymously called Sister Mary Joseph's nodule (SMJN), it often signposts an advanced underlying visceral malignancy with dire prognosis. While metastasis to the umbilicus has been adjudged rare, representing only about 10% of all cutaneous metastases,3 the umbilical region is unique among the cutaneous regions in being a focal point of metastases of primary tumors from diverse human organs.4
The differentials of an umbilical mass or nodule are diverse and may sometimes present a diagnostic challenge or uncertainty.5,6 Because malignancies constitute a high proportion of the incident lesions of the umbilicus, and because the most common malignant neoplasms of the umbilicus are metastatic tumors (SMJN) signifying a more serious underlying situation, accurate and correct diagnoses becomes very imperative. Identification of demographic and clinical features that can contribute to diagnostic resolution at presentation is desirable. Dae-Lyong Ha et al.7 investigated for the clinical and dermoscopic differences that may distinguish benign and malignant lesions of the umbilicus.
In the present study, umbilical biopsies received in a tertiary hospital of a black African population over a period of 20 years were analyzed according to sex in order to determine if there are gender distinctive attributes of umbilical nodules.
Materials and methodsThis is a descriptive, retrospective cross-sectional study of all umbilical biopsies seen at the Morbid Anatomy Department, University of Nigeria Teaching Hospital, Ituku-Ozalla, (UNTH) from 1st January 2000 to 31st December 2019. UNTH is a university teaching hospital and a tertiary referral center situated in Enugu state, south-eastern Nigeria. UNTH being a referral center, attracts patients from all socioeconomic strata without any bias. The study was approved by UNTH research ethics committee.
A search of our departmental digital records was undertaken, and all umbilical biopsies submitted in the period under review were identified. Data extracted included patient's gender, age, date of biopsy, type of biopsy, histopathological diagnoses and site of primary tumor where applicable. Data so obtained were entered into Statistical Package for Social Science (SPSS) as well as R statistical software, split by gender variable, analyzed and plotted using the ggplot2 package of R.8,9 Continuous variables were analyzed for mean (SD) and compared by Student's t-test while categorical variables were analyzed for frequency and compared with Pearson Chi square. Alpha level of<0.05 was considered significant.
ResultsOnly 67 umbilical biopsies were present in 2620 cutaneous biopsies received over a 20-year period. Thus, umbilical biopsies constituted 2.6% of all cutaneous biopsies seen during the period under review and this translates to about 3 umbilical biopsies per year. There were 22 males and 45 females giving a male: female ratio of 1:2. The ages of the male subjects ranged from 6 to 79 years while that of the females was 22–76 years. The mean age (SD) of male patients was 47.8 years (19.4 years) while that of the females was 42.8 years (13.9 years). The difference between the mean ages of both sexes was not statistically significant [t(df32)=−1.09; p=0.28].
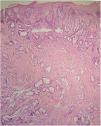
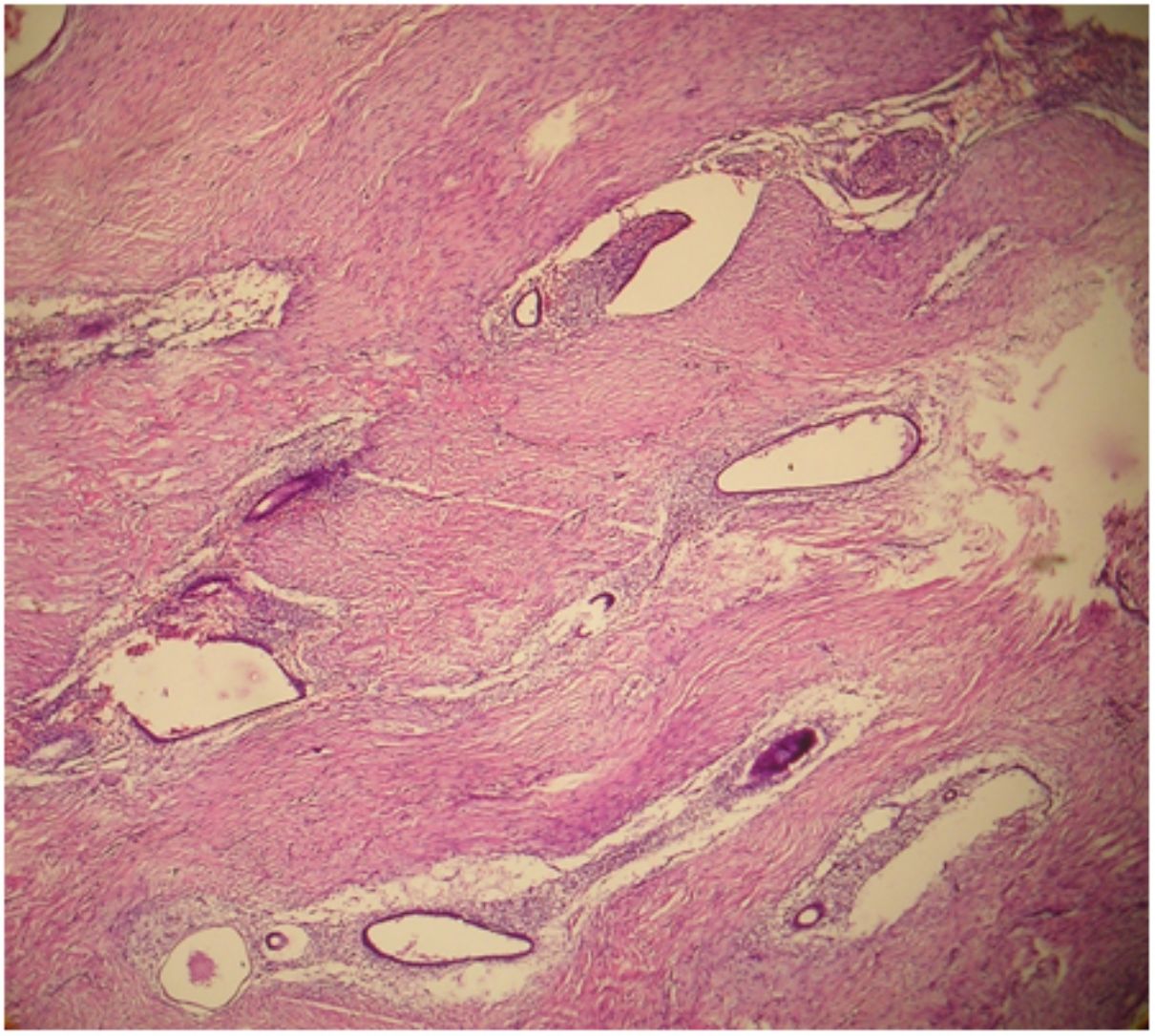
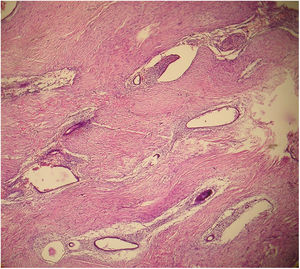
Table 1 depicts the histological diagnoses and the biological nature of the umbilical lesions in both sexes. It shows 25(37.3%) of the 67 umbilical biopsies were benign while 42(62.7%) were malignant. Whereas malignant lesions occurred with almost equal frequency in both males and females, 23 out of the 25 benign lesions occurred in females and were almost entirely endometriosis (Fig. 1). Overall, 78% of all umbilical lesions in females were of gynecological derivation (endometriosis and gynecological malignancies). The mean age (SD) of patients with benign umbilical lesion compared to malignant diagnoses was 32.8(8.3) years against 51.4(15.3) years. The difference was statistically significant [t(df64)=−6.44, p<0.001].
Age group, nature of lesions and histological diagnoses of umbilical biopsies stratified according to sex of patients.
| Sex of patients | ||
|---|---|---|
| Female | Male | |
| Age group | ||
| <25 years | 1 | 1 |
| 25–34 years | 14 | 5 |
| 35–44 years | 15 | 5 |
| 45–54 years | 4 | 2 |
| 55 years and above | 11 | 9 |
| Total | 45 | 22 |
| Nature of lesion | ||
| Benign | 23 | 2 |
| Malignant | 22 | 20 |
| Total | 45 | 22 |
| Histological diagnosis | ||
| Endometriosis | 23 | 0 |
| Epidermoid cyst | 0 | 1 |
| Granular cell tumor | 0 | 1 |
| Metastatic carcinoma | 21 | 20 |
| Retiform haemangioendothelioma | 1 | 0 |
| Total | 45 | 22 |
Table 2 is a cross tabulation of nature of lesion by sex of patient showing a statistically strong association between the two variables [χ2(1)=11.2; p=0.001]. About 91% (20/22) of the biopsies in males was malignant and 9.1% (2/22) was benign. In comparison, 48.9% of biopsies in females were malignant and 51.1% benign. The odds of malignant umbilical biopsy in males compared to females is 10.5 [OR=10.5; 95% CI=2.2–50.1].
Cross tabulation of nature of lesion and sex of 67 cases of umbilical biopsies.
| Sex | Nature of lesion | Total | Statistics | |
|---|---|---|---|---|
| Malignant | Benign | |||
| Male | 20 (90.9) | 2 (9.1) | 22 (100.0) | χ2(1)=11.2; p=0.001 |
| Female | 22 (48.9) | 23 (51.1) | 45 (100.0) | Cramer's V=0.408; p=0.001 |
| Total | 42 (62.7) | 25 (37.3) | 67 (100.0) | OR=10.5; 95%CI (2.2; 50.1) |
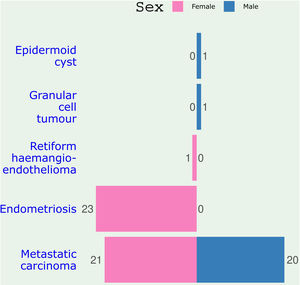
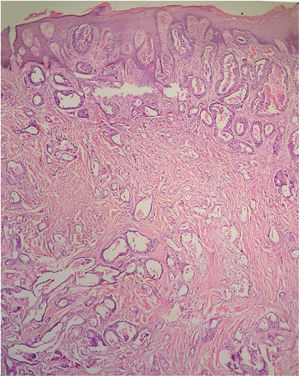
Histologically, the major underlying pathology of the umbilical biopsies was endometriosis and metastatic carcinomas (SMJN). Table 3 shows the histology of the metastatic cancers and their primary organs for both male and female patients. In males, colon was the most common site of primary tumor followed by stomach while in females, ovary was the most common site followed by pancreas and uterus (Fig. 2). Altogether, colon was the most common location of primary tumor giving metastasis to the umbilicus. It contributed 19.5% of all the metastatic carcinomas. Ovary was second (17.1%) and stomach third (14.7%) most common source of metastasis to the umbilicus. The primary source of the umbilical metastasis was not detected in 19.5% of the cases (Fig. 3).
Primary sites and histological type of metastatic umbilical tumors.
| Primary site | Cancer type | Count | Percent | |
|---|---|---|---|---|
| Female | Male | |||
| Colon | Adenocarcinoma | 1 | 7 | 19.5 |
| Stomach | Adenocarcinoma | 0 | 6 | 14.7 |
| Pancreas | Adenocarcinoma | 3 | 1 | 9.8 |
| Rectum | Adenocarcinoma | 1 | 0 | 2.4 |
| Liver | Hepatocellular carcinoma | 0 | 1 | 2.4 |
| Gallbladder | Adenocarcinoma | 1 | 0 | 2.4 |
| Ovary | Serous adenocarcinoma | 4 | – | 9.8 |
| Endometrioid carcinoma | 2 | – | 4.9 | |
| Sertoli-Leydig cell tumor | 1 | – | 2.4 | |
| Uterus | Serous adenocarcinoma | 2 | – | 4.9 |
| Adenosquamous carcinoma | 1 | – | 2.4 | |
| Cervix | Squamous cell carcinoma | 2 | – | 4.9 |
| Undetected | Adenocarcinoma | 0 | 3 | 7.3 |
| Metastatic carcinoma (nos) | 2 | 1 | 7.3 | |
| Mucinous adenocarcinoma | 1 | 1 | 4.9 | |
| Total | 21 | 20 | 100 | |
In the present study, we analyzed the demographic and pathological features of umbilical biopsies received in a histopathology laboratory over a 20-year period and we compared the features of umbilical nodules in male and female in order to ascertain if there are gender distinctive characteristics that might be of help in clinical assessment. The umbilicus is an anatomical site that can present a gamut of disease entities such as metastatic and primary cancers, benign neoplasms, endometriosis, developmental lesions, pilonidal sinus among others.6,7,10,11 With this variety of conditions and with the umbilicus established as a focus of metastatic deposit from diverse visceral organs, accurate assessment and diagnoses of umbilical lesions is necessary. Our study documents the relative infrequency of umbilical nodules – 2.6% of all cutaneous biopsies in our setting. However, the sizable numbers of metastatic malignancy popping up at the umbilicus confers on umbilical lesions, considerable prognostic significance. While histopathologic assessment will yield definitive diagnoses in cases of umbilical tumors, demographic, clinical and demoscopic features could, most times point to the likely diagnoses of lesion in question.7,11
There is no shortage, in medical literature, of articles focusing on the umbilicus. There are case reports and case series of metastatic (SMJN) and primary cancers; case reports and case series of umbilical endometriosis in addition to other benign conditions and review articles aggregating published case reports from multiple sources. Scarce, however, are single institution-based, cross sectional study of all umbilical biopsies such as we present in the current work. Our PubMed and Google Scholar search returned only two such studies.7,10
In a historical study, in which 677 literature reported cases of umbilical lesions were aggregated, Barrow MV determined that 32.2% were endometriosis, 29.7% metastatic carcinomas, 29.7% benign tumors and 8.4% primary umbilical malignancy.12 His report did not specify the sex distribution of the umbilical lesions but it can be inferred that females were the preponderant subjects given the high proportion of endometriosis (32.2%) and the fact that 17.8% of 202 metastatic tumors were attributed to gynecological organs. In our series, 67% (45/67) of the umbilical lesions were presented by females while 33% (22/67) were from males. A similar trend of female predominance was portrayed in another report by Yan et al., in which 78.8% (78/99) of all umbilical lesions were seen in women and 21.2% (21/99) in males.10 Thus umbilical biopsies are usually more common in females than males (Fig. 4).
Considering the histology of the biopsies, 90.9% (20/22) of male biopsies in our series turned out malignant compared to 48.9% (22/45) in females. Thus the odds of an umbilical biopsy being malignant in males was 10 fold that of the female. This wide female to male disparity in proportion of malignant biopsies was caused by high contribution of umbilical endometriosis in females and near absence of benign conditions in our male presentation. In contrast, 61% of female and 52% of male umbilical lesions featured in the report of Yan et al.10 were malignant. They registered a varied spectrum and higher numbers of benign conditions including epidermal inclusion cysts (15/40), endometriosis (11/40), lipomas (3/40), neurofibroma (3/40), fibromas (3/40), and skin adnexal tumor (2/40). In their study, 10 out of the 40 benign conditions were seen in males while 30 presented in females. The benign conditions seen in our study consists of 23 cases of endometriosis all in females, 1 case of epidermoid cyst in a 6-year-old boy and 1 case of granular cell myoblastoma presenting in a 25-year-old man. Remarkably, benign umbilical biopsies in our setting were almost entirely, endometriosis. The dearth of other benign condition might be due to genuine low incidence or, more plausibly, non-presentation for care. In our health system where payment for health care is essentially out-of-pocket, patients are known to present late, and only if symptoms become too disturbing. Ninety-six percent of biopsies in our series are composed of either metastatic carcinoma or endometriosis, two conditions that, primarily, may have extra-umbilical symptoms and umbilical manifestation of worrisome nature such as ulceration, infection, discharge, pain or catemenial bleeding. Whatever be the reason, it is instructive to recognize that in our setting, umbilical lesions presented by adult males have a high chance of being something sinister.
Similar to the report of Yan and colleagues,10 primary malignant lesion was extremely rare in our series. Papalas et al.13 reported a series of 77 umbilical malignancies and determined that 88% were metastatic carcinomas and 12% primary to the umbilicus. All the primary umbilical tumors were skin cancers including 6 melanomas, 2 squamous cell carcinomas and 1 basal cell carcinoma.13 Similarly, primary skin cancers constituted the second most common cancer type in the primary umbilical malignancies reported by Barrow VM.12 Given that primary skin cancer is the dominant histology of primary umbilical malignancies, it is hardly surprising that our series is devoid of such tumors because the epidemiological characteristics of skin cancer in black African population like ours, is distinct. Africans population have low propensity for skin cancer when compared with whites, melanomas occur mostly in acral locations and squamous cell carcinomas arise most times in Marjolin ulcers or chronically inflamed scars.14
In our study, the gynecological organs were the most common primary source of metastatic malignancy to the umbilicus in females, while gastro intestinal tract was the most common source in males (Fig. 2). This finding is in agreement with previous reports.15–17 Umbilicus is unique in being a ‘fertile soil’ for metastasizing tumors from diverse organs. Secondary tumors of the umbilicus have originated from stomach, small intestine, colon, rectum, pancreas, gallbladder, liver, ovary, endometrium, cervix, fallopian tube, urinary bladder, kidney, prostate, breast, appendix and lungs.4,12,13 The mechanism by which metastasis to the umbilicus occurs is not fully elucidated but factors identified as potentially contributory include: extensive vascular (venous, arterial and lymphatic) connections with the upper and lower trunks of the body; ligamentous remnants of embryological structures; and proximity to abdominal viscera.3 Also likely to be important are intrinsic tumor characteristics and umbilical skin microenvironment which might cooperate to encourage tumor homing. Hugen et al. report that umbilical metastasis was detected synchronously with the primary tumor in 67.7% of cases and metachronously in 32.3% of patients and concluded with the fact that survival was dependent on the origin of the primary tumor and poor overall survival rates warrant early recognition.17
In addition to metastatic carcinoma, endometriosis featured prominently in our series of umbilical lesions raising questions about possible common molecular mechanisms in the umbilical implantation of both entities. Also of note is the finding that lesions of gynecological derivation are responsible for about 78% of umbilical biopsies in females. Age at presentation is another pointer to underlying pathology. In this regard, a spectrum of congenital lesions feature more in pediatric age groups while tumors are more of a concern in presenting adults.18 Hence any umbilical growth or nodule should be evaluated diligently, especially in adults, as it can be the only clue to underlying hidden malignancy.
ConclusionUmbilical biopsies were relatively infrequent in our practice representing only about 2.6% of all cutaneous biopsies at an average of about 3 biopsies per year. Umbilical lesions were more common in females than males. Sixty-seven percent of all umbilical biopsies in our setting were contributed by females and 78% of all umbilical lesions in females were from gynecological organs. In our setting, umbilical biopsies in males were mostly malignant. An umbilical lesion had 10 time more odds of being malignant in males compared with females. All malignant umbilical lesions were metastatic. The gastrointestinal tract was the most common primary source of umbilical metastasis in males while gynecological organs were the most common source in females.
Conflict of interestThe authors declare that they have no conflict of interest.