A 51-year-old woman with a past medical history of hypothyroidism on 100mg of levothyroxine daily, presented with a <1-year history of generalized pruritic lesions.
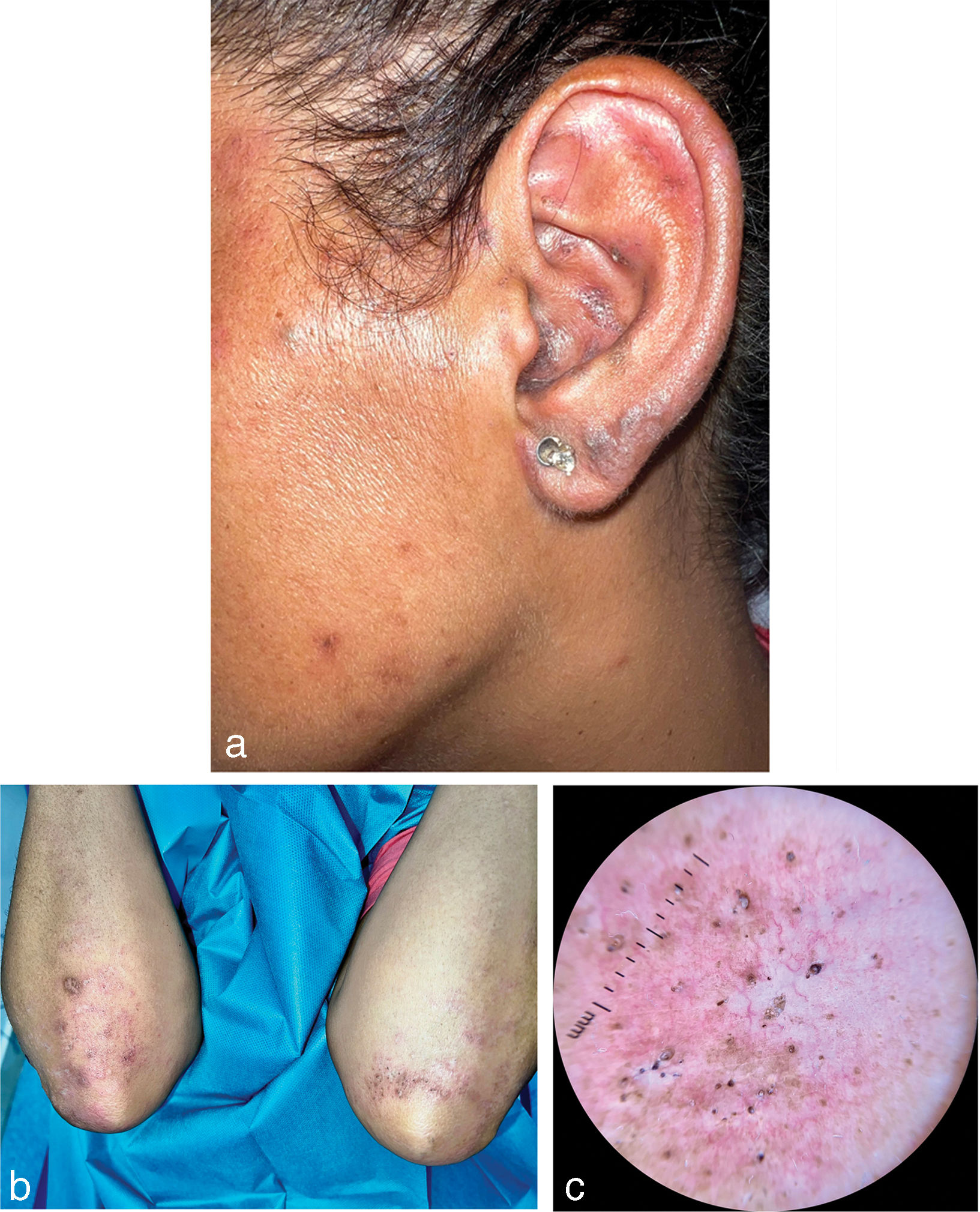
Physical examinationPhysical examination revealed the presence of multiple plaques composed of follicular plugs and open comedones with an erythematous–violaceous peripheral halo, distributed on the elbows, ears, preauricular region, knees, and palms, without involvement of the soles or mucous membranes (Fig. 1a–c). Lesions were highly pruritic and refractory to treatment with sedative antihistamines, appeared after sun exposure and were accompanied by asthenia, arthralgia, and a slight increase of hair loss. Photosensitivity, however, was not reported.
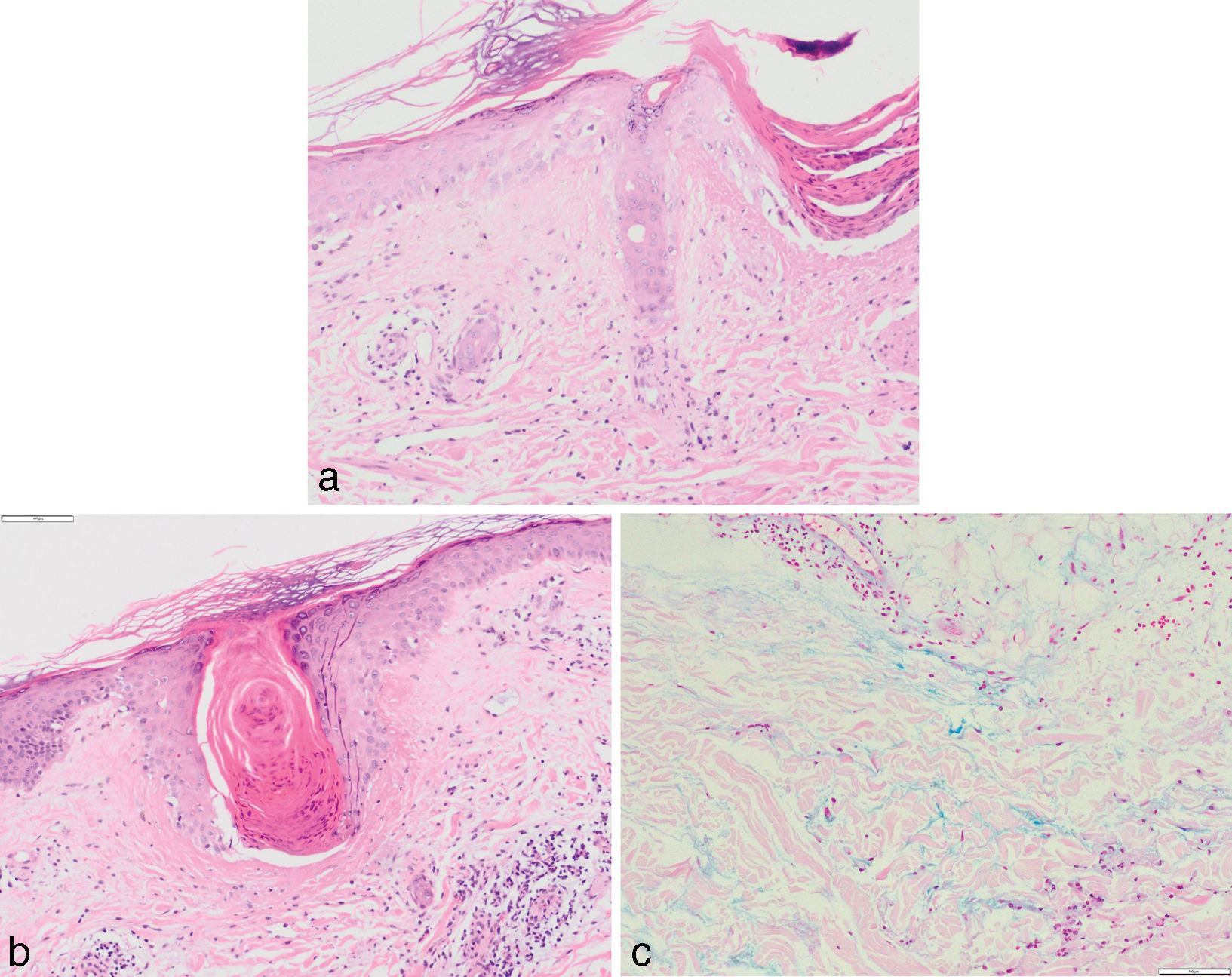
Histologic examination revealed an atrophic epidermis with vacuolar degeneration and rarefaction of the basal layer (Fig. 2a), along with superficial and deep perivascular dermatitis, a mild-to-moderate chronic lymphomonocytic inflammatory infiltrate in the superficial and mid-dermis that spared the periannexal area, and marked follicular hyperparakeratosis with dilation of the follicular ostium and infundibular destruction with fibrinoid necrosis forming early comedones (Fig. 2b), accompanied by interstitial mucin in the reticular dermis (Fig. 2c).
Additional tests: blood tested revealed low-titer positive antinuclear antibodies (ANA 1:40), thrombocytopenia, and decreased serum complement C3 levels, and positivity for extractable nuclear antigen (ENA) antibodies, anti-Smith (anti-Sm) antibodies, anti-small nuclear ribonucleoprotein (anti-RNP) antibodies, and anti-Ro antibodies. Antiphospholipid antibodies turned out negative.
DiagnosisComedonic lupus cutaneous, which did not meet the classification criteria for systemic lupus erythematosus since ANA titers did not reach 1:80.
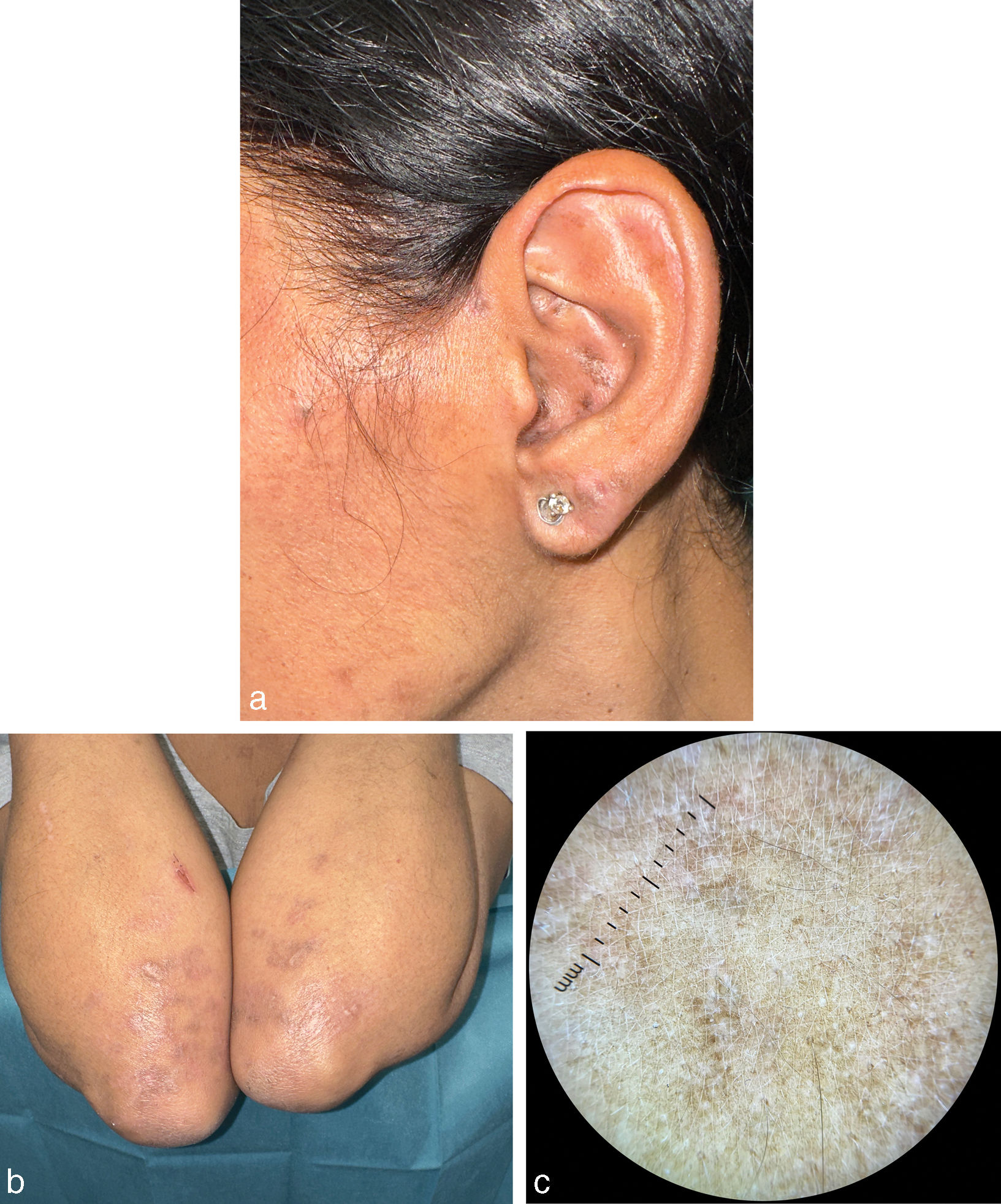
Disease progression and treatmentAfter an early regimen of topical tretinoin 0.5mg/g daily and 25mg of hydroxyzine orally every 8h—which proved ineffective—oral prednisone and topical fluticasone were administered, along with strict photoprotection. Afterwards, oral hydroxychloroquine at a dose of 200mg every 12h was introduced, with maintenance therapy using tacrolimus 0.1% ointment. Lesions improved significantly after 2 months of treatment (Fig. 3a–c), along with the resolution of thrombocytopenia, negative autoimmune parameters, and normalization of C3 levels.
CommentaryComedonic lupus is a rare and poorly understood form of chronic cutaneous lupus erythematosus (CCLE).1 It is primarily described in young women in their 30s and 40s, with a slightly increased risk among smokers.1,2 Lesions are typically pruritic and appear in photo-exposed areas, predominantly on the malar, preauricular, and chin regions. They consist of comedones or cysts with varying degrees of surrounding inflammation and may heal with scarring.1
The presence of comedones can be associated with elevated levels of interleukin-1 (IL-1), as this has been found to be biologically and pathologically significant in early-stage comedones and is known to play a crucial role in the pathogenesis of lupus erythematosus.3,4 Therefore, controlling inflammatory activity is essential to prevent the growth of new lesions, whereas keratolytics or sebum regulators such as topical retinoids have proven less effective.5
This condition can be easily mistaken for other benign conditions such as acne vulgaris, which typically exhibits more inflammatory flare-ups, pustules, and a distribution beyond photo-exposed areas. Other differential diagnoses include follicular lichen planus tumidus, which requires histopathological and analytical findings for differentiation; milia en plaque; Favre-Racouchot disease—elastosis with cysts and comedones—which features similar lesions but less inflammation and significant actinic damage; nevus comedonicus—which is present since childhood—syringomas; or trichoepitheliomas—which require histological examination for definitive diagnosis.1,5 Currently, although comedonic lupus is considered an underdiagnosed form of lupus, it is gaining clinical relevance.1,2,5
However, comedonic CCLE can be locally destructive, leading to atrophic and disfiguring scars in untreated cases.6 Immunofluorescence assays may assist in diagnosis when histopathological findings prove inconclusive, as deposits of IgM, IgG, and C3 at the dermoepidermal junction can be observed.1,5
Regarding treatment, photoprotection is essential in all cases.2 Oral hydroxychloroquine has demonstrated the highest efficacy, followed, to a lesser extent, by topical corticosteroids or oral tetracyclines.1,2 Other authors have reported satisfactory outcomes with dapsone combined with methotrexate in 2 cases.1 Topical retinoids have shown limited effectiveness.5 Since up to one-third of cases are associated with systemic lupus erythematosus, a comprehensive evaluation and regular follow-ups are necessary to prevent future local CCLE-related complications.1,5,6
Conflicts of interestNone declared.