The term coma blisters refers to a condition that occurs in patients who lose consciousness. It was first described in 1812 by Larrey1 in soldiers with carbon monoxide poisoning. Since then, it has been mainly associated with overdose of drugs and nervous system depressants, such as barbiturates, tricyclic antidepressants, opiates and alcohol; neurological disorders, such as meningoencephalitis, cerebrovascular disease, and cranioencephalic trauma; and metabolic disorders, such as hyperkalemia, hypoglycemia, and diabetic ketoacidosis.2–4 Coma blisters, however, have also been described in patients without an altered state of conscience, in particular in cases of long immobilization or Wegener granulomatosis.5–7
We present the case of a 24-year-old woman with a history of a personality disorder and occasional consumption of cocaine and amphetamines who was found unconscious in her home. She had taken multiple pills from her regular medication supply (topiramate, duloxetine, quetiapine, and clorazepate).
On arrival at the emergency department, she had a low level of consciousness (score 6 on the Glasgow Coma Scale), pale skin, and reactive mydriatic pupils. Partial improvement (Glasgow Coma Scale 10) was observed following physical stimulation, and the patient was treated with oxygen, fluid therapy, gastric lavage, and activated charcoal.
There was no evidence of acute intracranial lesions on the computed tomography scan. The laboratory workup showed a serum creatine kinase level of 5590U/L and normal kidney function. The urine drug screening test showed high levels of benzodiazepines.
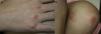
During her first 24hours in hospital, the patient developed asymptomatic skin lesions located mainly on bony prominences. The physical examination showed tense clear fluid-filled blisters on well-delimited erythematous plaques (Fig. 1A,B). The lesions had an artifactual morphology and were characteristically located on pressure points (metacarpophalangeal joints on the right hand, right hip, and left knee).
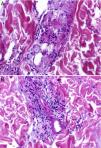
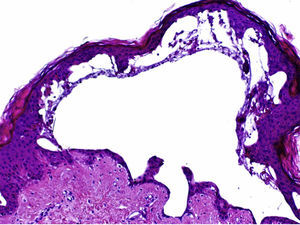
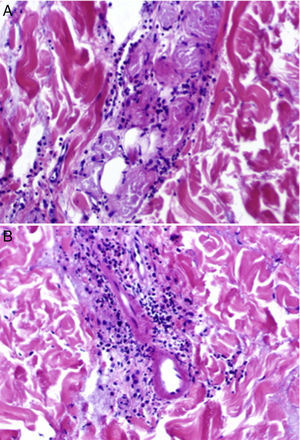
The histopathologic examination showed a subepidermal blister with foci of reepithelialization (Fig. 2) and focal epithelial necrosis of eccrine coils, with periglandular infiltration of neutrophils (Fig. 3A). Additional findings included dermal, perivascular, and periadnexal infiltrates, which were predominantly neutrophilic, together with foci of fibrinoid necrosis in the walls of the small dermal capillaries and neutrophilic infiltration of the walls (Fig. 3B).
A, Focal epithelial necrosis in the eccrine coils with neutrophilic periglandular infiltration (hematoxylin-eosin, original magnification ×20). B, Predominantly neutrophilic perivascular and periadnexal infiltrates and foci of fibrinoid necrosis in the walls of dermal capillaries, with neutrophilic infiltration of the walls (hematoxylin-eosin, original magnification ×20).
Administration of topical antibiotics led to resolution of the lesions within 3 weeks, and there were no signs of scarring or recurrence.
The clinical presentation and histopathologic findings were consistent with a diagnosis of coma blisters.
Clinically, coma blisters are characterized by tense clear or hemorrhagic blisters that develop on erythematous-violaceous macules or plaques of varying size. The lesions typically appear within 24hours of the intake of drugs and within 48 to 72hours of the loss of consciousness. They primarily develop on pressure points, such as fingers and toes, elbows, knees, ankles, and heels. They are self-limiting and heal within days or weeks, without causing scarring or atrophy. The only treatment indicated thus is topical treatment to prevent secondary infections.2,8
Multiple factors have been implicated in the etiology and pathogenesis of coma blisters, including local pressure or friction, generalized hypoxia and tissue ischemia, direct toxicity due to drugs excreted in sweat, immune mechanisms, and vasomotor changes in comatose states.9
Although a diagnosis can be established on clinical grounds only, a histopathologic study can be of great use. The main histopathologic findings are subepidermal or intraepidermal blisters and eccrine gland necrosis, mainly affecting the secretory portion. The secretory coils and ducts of the eccrine glands show a granular eosinophilic cytoplasm, ghost nuclei, and irregular membranes. However, the absence of necrosis in these glands does not necessarily rule out a diagnosis of coma blisters. Other possible findings are neutrophil exocytosis, necrosis of dermal or subcutaneous tissue or epidermal appendages, predominantly neutrophilic perivascular infiltrates, focal fibrinoid necrosis of the walls of small capillaries and arterioles, and thrombi in the lumen of dermal vascular structures.10
The vascular damage observed in drug-induced coma blisters is probably a consequence rather than a cause of the blisters. Furthermore, the absence of an epidermal infiltrate and the presence of thrombi in the dermal vessels are mainly observed in coma blisters not induced by drugs.10
Direct immunofluorescence studies performed in certain cases of coma blisters have shown patched intercellular staining for immunoglobulin (Ig) G, IgA, and C3, together with IgG, IgM, and C3 deposits in dermal vessel walls and epidermal keratinocytes. These findings, however, are nonspecific and are not considered to result from an immune-mediated response.4,10
In conclusion, coma blisters are a benign, self-limiting condition that should be suspected in patients who develop pressure blisters several hours after an altered state of consciousness. Although the diagnosis is mainly clinical, correlation of clinical and pathologic findings is necessary to rule out other blistering dermatoses.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vázquez-Osorio I, Gonzalvo-Rodríguez P, Rodríguez-Díaz E. Ampollas del coma tras sobredosis de fármacos depresores del sistema nervioso central. Actas Dermosifiliogr. 2017;108:81–83.