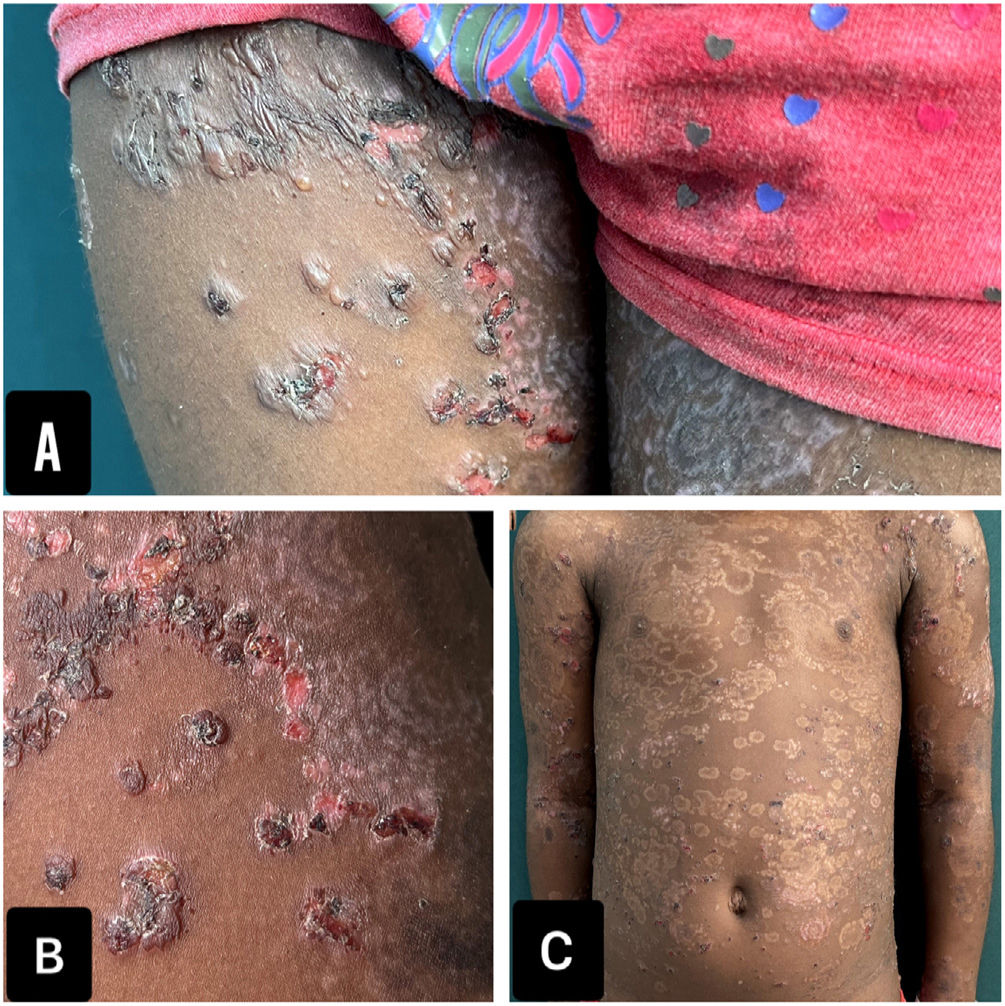
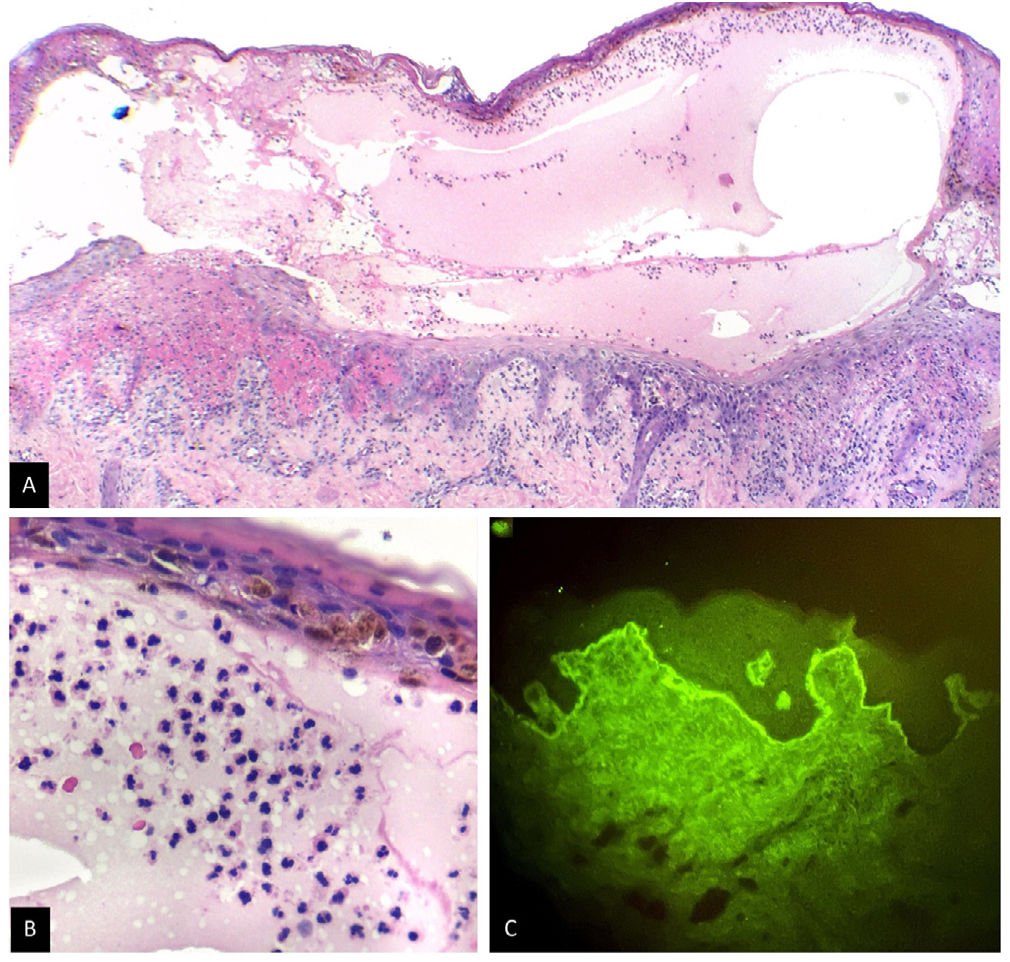
A 6-year-old girl, residing in a rural area, presented with a 2-month history of tense, slightly pruritic blisters on her face, neck, trunk, and limbs associated with oral and vulvar lesions. She had been given multiple systemic antibiotics and topical steroids without improvement. Her mother emphasized that lesions had started a day after the administration of the 2nd dose of CoronaVac. The only relevant piece of information in the patient's medical history was a diagnosis of sickle cell trait, which had remained asymptomatic until then. Skin phototype V was confirmed on the physical examination, with presence of multiple tense blisters distributed in rosettes, associated with hemorrhagic crusts and residual hypopigmented macules (Fig. 1). Notably, the supplementary tests performed confirmed the presence of microcytic anemia with anisocytosis. A skin biopsy confirmed the presence of a subepidermal blister with a neutrophil-rich inflammatory infiltrate, and a negative direct immunofluorescence (DIF) for IgG, IgM, and C3, but positive for IgA with a linear pattern at the basement membrane zone (Fig. 2). Indirect immunofluorescence and other antigenic tests were not performed because they were not available at the center.
What is your diagnosis?
DiagnosisThe generalized, symmetrical blisters on the skin and mucous membranes, with histopathology and DIF compatible with linear IgA, along with 3 Naranjo criteria, led to the diagnosis of post-vaccinal linear IgA dermatosis.
Due to the patient's microcytic anemia and sickle cell trait, dapsone was not administered. Instead, a 2-week course of prednisolone at 1mg/kg/day resulted in the complete resolution of the lesions. Given the vaccination-associated etiology, clinical follow-up without systemic immunosuppressants was considered. The patient remains asymptomatic at the 12-month follow-up.
CommentsLinear IgA dermatosis is a rare autoimmune blistering disease that presents with tense blisters on the skin of children and adults with, sometimes, mucosa involvement. Most cases of linear IgA dermatosis are of idiopathic etiology, but it has also been associated with drugs, vaccines, neoplasms, and autoimmune diseases.1 Among the pediatric population, cases associated with vaccination against measles-mumps-rubella and human papillomavirus have been reported. The clinical signs of post-vaccinal linear IgA dermatosis may be similar to idiopathic cases, show greater mucosal involvement, or resemble lesions of erythema multiforme or Stevens-Johnson syndrome. Regarding histopathology and DIF, no etiology-related significant differences have ever been reported, which is why a complete medical history establishes the differential diagnosis.1
The pathophysiological mechanism of post-vaccinal linear IgA dermatosis is still to be elucidated. One theory proposes molecular mimicry, where immune system activation mediated by vaccine antigens induces specific autoantibodies. Additionally, vaccines may stimulate the production of interferons and interleukins, which increase the synthesis of IgA antibodies. Unlike the 2 mentioned theories, it has also been suggested that vaccination could increase the production of autoantibodies in patients with pre-existing subclinical levels, which would explain the occurrence of rapid-onset diseases, as in the case presented here.3
Up until now, 4 cases of post-SARS-CoV-2 vaccine-related linear IgA dermatosis have been described, all in individuals older than 60 years (in 2 patients vaccinated with Moderna, 1 with Pfizer, and 1 with AstraZeneca).4–6 Our case is the only case ever described in a pediatric patient vaccinated with CoronaVac. The distinction between idiopathic and drug or vaccine-induced linear IgA dermatosis is that the former typically requires systemic immunosuppressants for longer periods of time, while the latter usually improves after drug discontinuation and short courses of topical or systemic immunosuppressants. In our patient, who lives in a dispersed rural area and had a past medical history of sickle cell trait, the diagnosis of post-vaccinal linear IgA dermatosis conditioned the use of short-term systemic immunosuppressants, avoiding the risks of prolonged systemic therapy.