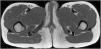
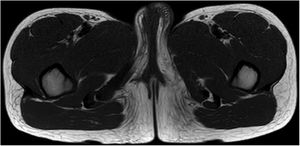
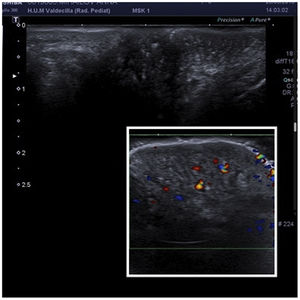
A 9-year-old Moldovan girl with no personal history of interest was referred from pediatrics for left vulvar hypertrophy that had developed over the preceding 6 months and had not responded to topical treatment with corticosteroids and antifungals. The patient reported no local trauma and had not undergone abdominal surgery. The hypertrophy was not accompanied by vaginal exudate and was completely asymptomatic. The patient had maintained excellent general health at all times. Physical examination revealed clear vulvar asymmetry. The left labium majus was enlarged and perifollicular accentuation and mild scaling were evident. No other local inflammatory signs or associated extragenital skin alterations were observed. On palpation the affected area had a soft consistency similar to that of the contralateral labium majus. No palpable subcutaneous lesions were detected. Examination of the rest of the genital area revealed no findings of interest. The patient was prepubertal (Tanner stage I) (Fig. 1). Soft tissue ultrasound showed an unencapsulated, heterogeneous structure with poorly defined margins, with increased vascularity in Doppler mode and no evidence of inguinal hernia (Fig. 2). A T1-weighted magnetic resonance imaging study confirmed the aforementioned findings and ruled out the presence of focal lesions (Fig. 3).
What Is Your Diagnosis?
DiagnosisAsymmetric hypertrophy of the left labium majus.
CommentOnce underlying neoplastic and inflammatory processes had been ruled out, the patient was diagnosed with asymmetric hypertrophy of the left labium majus based on clinical signs and radiological findings. It was decided not to treat the patient. The patient underwent repeated check-ups every 6 months consisting of a detailed physical examination and an ultrasound study. No further alterations were detected within a year of the initial consultation. Annual check-ups were scheduled during puberty until the patient reaches sexual maturity.
Asymmetric hypertrophy of the labium majus is rare, although its incidence is likely underestimated due to misdiagnosis and a lack of familiarity with this condition. Like asymmetric breast growth, it is considered a physiological response to prepubertal hormonal variations. Its detection is important in order to rule out more severe conditions. The mean age of onset is 8.3 years, and most cases are unilateral.1 Clinical signs consist of enlargement of the labium majus, giving rise to a mass of the same consistency as the surrounding tissue with poorly defined borders; no palpable solid or cystic lesions; and normal skin.2 It is not accompanied by systemic clinical signs and physical examination reveals no other alterations. Diagnosis is based on clinical and radiological findings. Biopsy may also be required in cases that are difficult to diagnose or have a prolonged course, or if an underlying tumor is suspected. The main histological findings are a marked proliferation of fibroblasts, positive staining for estrogen receptor, and an abundant extracellular matrix containing elements commonly found in normal vulvar tissue, including adipocytes, blood vessels, and nerves. Three typical radiological findings are described: heterogeneity; poorly defined borders; and increased vascularity.3 The differential diagnosis includes tumors such as mesenchymal tumors, solitary mastocytoma of the vulva, and aggressive angiomyxoma; congenital vascular and lymphatic malformations; infections such as schistosomiasis; inguinal hernias; Bartholin cyst; and inflammatory processes such as granulomatous vulvitis.1,2,4 In this case an underlying tumor was ruled out based on the results of the imaging studies, in which the bluish coloration typical of vascular malformations was absent, and the ultrasound examination, which showed no compatible findings. An infectious process was not suspected owing to the absence of local discomfort, secretion, and inflammation. Inguinal hernia becomes more pronounced when standing, and was ruled out by radiography. Finally, Bartholin cyst is rare in prepubertal children and granulomatous vulvitis has a recurrent course in the initial stages and is accompanied by progressive induration and, usually, erythema.
The prognosis is favorable: this condition tends to stabilize and can resolve spontaneously at puberty. Treatment is conservative. Although there is no consensus on the frequency of follow-up examinations or the requisite additional tests, Soyer et al. propose close follow-up consisting of physical examination and skin ultrasound every 3 months during the prepubertal period and annually after puberty.2 In patients with cosmetic and psychological repercussions, the treatment of choice is surgery once the individual has reached full sexual development, although the rate of recurrence is high. Asymmetric hypertrophy of the labia minora is another recently described variant of normal genital anatomy that also occurs during puberty and, due to its location, tends to cause greater local discomfort.5 Pediatricians and dermatologists should be familiar with these conditions in order to avoid unnecessary invasive diagnostic and therapeutic procedures.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors thank Dr. Vanesa Gómez Dermit of the Pediatric Radiology Department, Marqués de Valdecilla University Hospital.
Please cite this article as: Reguero-del Cura L, Durán-Vian C, Navarro-Fernández I, López-Sundh AE, Gómez-Fernández C. Hipertrofia asimétrica de labio mayor en una niña de 9 años. Actas Dermosifiliogr. 2021;112:535–536.