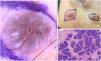
A skin-colored papule located on the left scapular region, previously unnoticed and of uncertain duration, in a 45-year-old woman (Fig. 1A). Dermoscopic examination revealed fine, well-focused telangiectasias traversing the lesion on a pink-whitish background (Fig. 1B). The lesion was surrounded by a pigment network, consistent with its location in an area of intense actinic damage. With an initial suspicion of basal cell carcinoma, a skin biopsy was performed, which confirmed the diagnosis (Fig. 1C).
Case report #2This is the case of a several-year history of an erythematous papule on the left nasal ala in a 60-year-old woman, with rapid growth in recent months (Fig. 2A). Dermoscopy revealed the presence of short, fine vessels and focused telangiectasias, along with rosettes and white-yellow globules corresponding to milia-like cysts (Fig. 2B). Histopathologic findings are shown in Fig. 2C.
Case report #3With clinical suspicion of a 2nd basal cell carcinoma, excision was performed on a recently appearing lesion on the left temple, associated with the growth of another immediately inferior lesion with occasional bleeding consistent with basal cell carcinoma (Fig. 3A). Dermoscopy demonstrated blue-gray dots and globules, focused telangiectasias and fine branching vessels, shiny white structures, and a central erosion over a blue-gray background (Fig. 3B). Histopathologic examination established the definitive diagnosis (Fig. 3C).
What is your diagnosis?
DiagnosisCase report #1Desmoplastic trichoepithelioma.
Case report #2Trichoepithelioma.
Case report #3Trichoblastoma.
CommentsCutaneous adnexal tumors include a diverse group of neoplasms arising from follicular or glandular skin structures.1 This group includes hamartomas as well as benign and malignant neoplasms, and they often pose a diagnostic challenge when differentiating them – clinically and histologically – from basal cell carcinoma (BCC), the most common malignant skin tumor.1–3
Trichoblastomas (TBs) are benign neoplasms with follicular differentiation arising from follicular germinative cells.2 There is controversy as to whether trichoepitheliomas (TEs) – including the desmoplastic variant (DTE) – represent histopathologic variants of TB or whether they constitute independent entities.1,3
As with other adnexal tumors, although the definitive diagnosis is histopathologic, several dermoscopic criteria have been proposed to aid in distinguishing TB/TE from BCC.3–6
TB usually presents as a solitary lesion and may occur anywhere except on non-hair-bearing skin, with a predilection for the face and scalp.1,2 Occasionally, TB may present as multiple lesions, be associated with other syndromes,3 or arise within a nevus sebaceus, where it is the most frequent associated neoplasm.4
TE shares similar clinical and epidemiologic characteristics and is notable for its desmoplastic histopathologic variant.2,4 Histologically, TB and TE are similar; however, some authors consider TE to represent the superficial variant of TB due to the location of its proliferative component.1
They differ from BCC in the presence of nests or islands of basaloid cells forming a well-circumscribed, symmetric tumor with vertical growth, surrounded by a loose stroma that separates them from the adjacent dermis. Retraction occurs between the stroma and surrounding dermis – unlike BCC, in which retraction is seen between the tumor and stroma and peripheral palisading is typically present.1–3,6
Dermoscopic criteria have been defined to help distinguish these tumors from BCC and from one another (TB/TE/DTE).3–7
In TE, various vascular patterns may be seen; the most common consists of small unfocused vessels, although fine and short arborizing vessels may also be present, resembling BCC.3,6,7 When the lesion is nonpigmented, these vessels appear over a white-pink background which, in the case of DTE, may show a whiter, “ivory-like” marbled appearance (Fig. 1B), sometimes with central umbilication. White-yellow globules representing milia-like cysts (Fig. 2B) and even rosettes are a common finding.6,7
TB, however, more commonly shows vessels similar to those of BCC, although punctate and glomerular vessels have been described in the adamantinoid variant.1,2 A characteristic feature of TB is its pigmented variant: a solitary blue-gray background (described as a “large blue-gray ovoid nest”), often accompanied by blue-gray dots and globules (Fig. 3B).6
This helps differentiate it from pigmented BCC, in which ovoid nests are generally multiple and smaller, contributing to clinical pigmentation but not typically forming a uniform pigmented background on dermoscopy.6,7
The definition of these dermoscopic structures has been guided by histopathologic correlation.8 Pigmented structures correspond to basaloid cell nests containing pigment; shiny white structures and “ivory-like” backgrounds correspond to dense, altered collagen in the abundant stroma of these tumors; and white globules/pseudocysts correspond to cystic structures such as milia-like cysts.
Therefore, although histopathology remains the diagnostic gold standard, dermoscopy significantly improves the ability to distinguish trichoblastic tumors from BCC and supports characterization of the different subtypes (TB/TE/DTE).1,4,6,7
Conflict of interestThe authors declare no conflict of interest.