Acral melanoma is associated with poor prognosis. Studying the characteristics and prognosis of Caucasian patients is crucial to understand the distinct features of this tumor.
ObjectivesTo analyze the epidemiological, clinicopathological, and prognostic features of acral melanoma in Caucasian patients.
MethodsWe conducted a retrospective, multicenter, cohort study of acral melanoma from a database across 20 hospitals from South Europe from January 2000 to December 2019.
ResultsA total of 733 acral melanomas were identified (median age, 67.5 years; 95.2%, Caucasians; 77.5% of which were located on the feet). Overall, 77.5% of cases were invasive melanomas. Foot melanomas had a higher proportion of invasive cases (80.8% vs 69.8%; p=0.003), stages III and IV at diagnosis (24.8% vs 11.7%; p<0.001), thicker Breslow depth (2.8mm vs 2.0mm; p=0.021) and a higher rate of positive sentinel lymph node biopsy (SLNB) (30.7% vs 15.7%; p=0.012). Thicker Breslow depth and later age of onset were risk factors for melanoma-specific survival. Thicker Breslow depth and ulceration were independent prognostic factors of relapse-free survival. Melanoma location and histopathological subtype were not associated with worse prognosis. Recurrences were a common finding (27.7%), with distant metastases appearing earlier than locoregional recurrences (1.32 years [IQR, 1.12–1.87] vs 2.14 years [IQR, 1.68–2.70]; p=0.015).
ConclusionThis study, the largest in a predominantly Caucasian population, underscores the unfavorable outcomes of acral melanoma. Foot melanomas exhibited delayed detection, increased invasiveness, thicker Breslow depth, increased SLNB involvement, and higher AJCC stages. The high recurrence rate and early distant metastases emphasize the critical role of intensive follow-up and routine imaging modalities to detect asymptomatic relapses.
El melanoma acral está asociado con un pronóstico desfavorable. El estudio sobre las características y el pronóstico en los pacientes caucásicos puede ser crucial para comprender las características distintivas de este tumor.
ObjetivosAnalizar las características epidemiológicas, clinicopatológicas y pronósticas del melanoma acral en los pacientes caucásicos.
Material y métodosEstudio de cohorte retrospectivo de melanoma acral a partir de una base de datos multi-institucional en 20 hospitales españoles, entre enero de 2000 y diciembre de 2019.
ResultadosSe identificaron un total de 733 melanomas acrales (edad media: 67,5 años, el 95,2% caucásicos y el 77,5% en los pies). En general, el 77,5% de los casos fueron invasivos. Los melanomas localizados en los pies tuvieron una mayor proporción de casos invasivos (80,8 vs. 69,8%; p=0,003), estadios III y IV al diagnóstico (24,8 vs. 11,7%; p<0,001), valores de Breslow más altos (2,8 vs. 2,0mm; p=0,021) y una mayor tasa de positividad de biopsia selectiva del ganglio centinela (BSGC) (30,7 vs. 15,7%; p=0,012). Un mayor grosor de Breslow y una edad de aparición más tardía fueron factores de riesgo para menor supervivencia específica por melanoma. Un mayor grosor de Breslow y la ulceración fueron los factores pronósticos independientes menor supervivencia libre de recaída. La localización del melanoma y el subtipo histopatológico no se asociaron con un peor pronóstico. Las recurrencias fueron frecuentes (27,7%), con a distancia apareciendo antes que las recurrencias locorregionales (1,32 años [IQR: 1,12-1,87] vs. 2,14 años [IQR: 1,68-2,70]; p=0,015).
ConclusiónEste estudio, el mayor en una población predominantemente caucásica, subraya los resultados desfavorables del melanoma acral. Los melanomas en los pies mostraron una detección tardía, mayor proporción de melanomas invasivos, valores de Breslow más profundos, mayor positividad o afectación de BSGC y estadios AJCC más altos. La alta tasa de recurrencia y las metástasis a distancia tempranas enfatizan el papel crítico del seguimiento intensivo y las pruebas de imagen rutinarias para detectar recaídas asintomáticas.
Acral melanoma affects all populations worldwide and is recognized as a distinct melanoma subgroup due to its unique characteristics including epidemiological, clinicopathological, molecular and prognostic features.1–8
According to the World Health Organization (WHO), acral melanoma are those occurring on the glabrous (non-hair-bearing) skin of the volar aspects of the fingers and toes, palms, soles, and nail beds.8 In addition, acral lentiginous melanoma (ALM) is a histopathological subtype of melanoma, characterized by specific morphological features as well.8–10
Acral melanoma is clearly associated with poorer prognosis vs cutaneous melanoma found in other locations.1,2,6,8,10,11 This adverse prognosis has been attributed to several factors, such as thicker Breslow depth and more advanced stages, which could be attributed to delayed diagnosis in part due to older age and non-visible anatomic locations, but also to a more aggressive behavior of the histopathological subtype or molecular background on non-sun exposed areas.1,2,4,6,8,10–12
In the present study, we used a large series of acral melanoma cases from a Southern European multicentre melanoma network over two decades to assess the epidemiological, clinicopathological and prognostic characteristics focusing on melanoma location, and analyze the recurrence patterns, melanoma-specific survival (MSS) and relapse-free survival (RFS) which can influence the follow-up and management of patients with acral melanoma.
Materials and methodsThe Network of Melanoma Centers of Catalonia database (Xarxa Melanoma Catalunya),13–15 a collaborative, prospective, multicenter database project including more than 20 hospitals from Northeast Spain was used to perform a retrospective study of patients with acral melanoma from January 2000 to December 2019 and followed up until August 2023.
All patients diagnosed with melanoma on acral sites with confirmed and properly registered melanoma diagnosed at these centers were initially considered to be included in the study. Data collection and analysis of all patients were approved under the protocol reference No. (HCB IRB; approval #2015/0298). Cases that were not consistent with the WHO definition of acral melanoma were excluded, keeping only those localized on the glabrous skin of hands and feet, including the nail apparatus. Cases were also excluded when location was not concordant, or when poorly defined.
The main variable used to analyze data was the anatomical location between hand and foot. Information on demographics, melanoma attributes, and prognostic data were recorded. Variables analyzed included gender, age at diagnosis, race and number of primary melanomas. Melanoma features included location (foot vs hand); stage (in situ vs invasive), staging according to the American Joint Committee on Cancer (AJCC) 8th edition, histopathological subtype (ALM, superficial spreading melanoma (SSM), lentigo maligna melanoma (LMM), nodular melanoma [NM] and other subtypes), Breslow depth, presence of mitotic figures, ulceration, associated nevi and satellitosis, sentinel lymph node biopsy (SLNB) performance and status. Prognostic data included recurrence patterns: timing and location (locoregional [lymph node or in-transit/satellitosis] and distant organs). Survival analysis was performed using 5-year and across the years MSS and RFS using the Kaplan–Meier method. Melanoma-related deaths were determined based on the patients’ death certificates and clinical history. MSS alludes to the time from melanoma excision to the date of death directly attributed to the disease. RFS alludes to the period from melanoma excision to disease detection in patients who had no residual disease after surgical procedures.
Statistical analysisThe frequencies and percentages were used to portray the distributions of categorical variables, while the distributions of continuous variables were expressed as median and interquartile range (IQR). The analysis of categorical variables included the Chi-squared test, or Fisher's exact test when any expected cell count was <5. Meanwhile, ordinal variables were expressed using the trend test. In the context of comparing independent continuous variables, the Wilcoxon rank sum test was employed.
The cohort median follow-up was estimated using the reverse Kaplan–Meier estimator. This estimate was conducted by applying the prodlim package (version 2023.3.31) in R, using both prodlim and Hist functions.
We conducted univariate and multivariate survival analyses, presenting HRs with 95% confidence intervals from fitted Cox proportional hazard models. These models were created using the coxph function in the survival software package (version 3.5.5) in R. Hazard ratios (HRs) were estimated for acral melanoma location (feet vs hands), independently adjusted for age at diagnosis, gender, Breslow Index, ulceration, and histological subtype. A concise Cox regression table showed both univariate and multivariate hazard ratios for improved data visualization.
Within the metastatic patient subgroup, we evaluated the relapse timing of acral melanomas using a cumulative event plot, calculating the median survival time. Additionally, we used Sankey plots as a powerful visual tool to depict the first metastatic locations of acral melanoma patients. Furthermore, we performed computations to ascertain the proportions of patients in each group with disease progression.
All statistical analyses were performed using the computing environment R version 4.3.1 (2023-06-16) and RStudio (version 2023.6.1.524). p values<0.05 were considered statistically significant.
ResultsA total of 906 patients were identified out of 19,951 registered in the regional database (Network of Melanoma Centers of Catalonia). After per-protocol exclusions (melanomas located on non-glabrous skin of hands and feet, or locations not concordant-poorly defined), the number of total acral melanomas of this study were 733 from a total of 730 patients. The median follow-up time of the cohort calculated with the reverse Kaplan–Meier methods was 8.34 years with an IQR, of 4.89–13.01 years.
Demographic and histopathological featuresThe demographic and histopathological features of all melanomas are shown in Table 1. The features of invasive melanomas (N=568, 77.5%) are shown in Table 2. Overall, median age was 67.5 years (IQR, 53.7–78.6; 58.5%, women). The anatomic distribution of the tumors was 568 on the feet (77.5%) and 165 on the hands (22.5%). A total of 95% of the patients were Caucasian.
Demographic and histopathological features of all melanomas.
| Variable | Overall, N=733 | Location | p-Valuea | |
|---|---|---|---|---|
| Foot, N=568 | Hand, N=165 | |||
| Gender, n (%) | 0.645 | |||
| Female | 429 (58.5%) | 335 (59.0%) | 94 (57.0%) | |
| Male | 304 (41.5%) | 233 (41.0%) | 71 (43.0%) | |
| Age, median (IQR) | 67.5 (53.7–78.6) | 67.8 (53.9–79.4) | 65.7 (53.2–76.2) | 0.099 |
| Race, n (%) | 0.371 | |||
| White | 338 (95.2%) | 266 (96.0%) | 72 (92.3%) | |
| Latin | 8 (2.3%) | 5 (1.8%) | 3 (3.8%) | |
| Asian | 4 (1.1%) | 2 (0.7%) | 2 (2.6%) | |
| Indian | 2 (0.6%) | 1 (0.4%) | 1 (1.3%) | |
| Gipsy | 1 (0.3%) | 1 (0.4%) | 0 (0.0%) | |
| Black | 1 (0.3%) | 1 (0.4%) | 0 (0.0%) | |
| Missing | 379 | 292 | 87 | |
| Staging, n (%) | 0.003 | |||
| In situ | 157 (21.7%) | 108 (19.2%) | 49 (30.2%) | |
| Invasive | 568 (78.3%) | 455 (80.8%) | 113 (69.8%) | |
| Missing | 8 | 5 | 3 | |
| AJCC 2017, n (%) | <0.001 | |||
| 0 | 156 (21.5%) | 107 (19.0%) | 49 (30.2%) | |
| I | 186 (25.7%) | 139 (24.7%) | 47 (29.0%) | |
| II | 224 (30.9%) | 177 (31.4%) | 47 (29.0%) | |
| III | 145 (20.0%) | 128 (22.7%) | 17 (10.5%) | |
| IV | 14 (1.9%) | 12 (2.1%) | 2 (1.2%) | |
| Missing | 8 | 5 | 3 | |
| Number of primary melanomas, n (%) | 0.189 | |||
| Multiple primary melanomas | 42 (5.7%) | 36 (6.3%) | 6 (3.6%) | |
| Single primary melanoma | 691 (94.3%) | 532 (93.7%) | 159 (96.4%) | |
| Associated nevus, n (%) | <0.001 | |||
| De novo melanoma | 363 (87.7%) | 265 (84.1%) | 98 (99.0%) | |
| Nevus-associated melanoma | 51 (12.3%) | 50 (15.9%) | 1 (1.0%) | |
| Missing | 319 | 253 | 66 | |
| Histological subtype, n (%) | 0.030 | |||
| Acral lentiginous | 666 (90.9%) | 509 (89.6%) | 157 (95.2%) | |
| Nodular | 67 (9.1%) | 59 (10.4%) | 8 (4.8%) | |
Data expressed as No. (%) unless otherwise indicated.
IQR, Interquartil range; AJCC, American Joint Committee on Cancer;
Demographic and histopathological features of invasive melanomas.
| Variable | Overall, N=568 | Location | p-Valuea | |
|---|---|---|---|---|
| Foot, N=455 | Hand, N=113 | |||
| Gender, n (%) | 0.573 | |||
| Female | 315 (55.5%) | 255 (56.0%) | 60 (53.1%) | |
| Male | 253 (44.5%) | 200 (44.0%) | 53 (46.9%) | |
| Age, median (IQR) | 69.5 (56.4–79.4) | 70.5 (56.4–79.9) | 68.8 (56.6–77.7) | 0.375 |
| AJCC 2017, n (%) | 0.014 | |||
| I | 185 (32.6%) | 138 (30.3%) | 47 (41.6%) | |
| II | 224 (39.4%) | 177 (38.9%) | 47 (41.6%) | |
| III | 145 (25.5%) | 128 (28.1%) | 17 (15.0%) | |
| IV | 14 (2.5%) | 12 (2.6%) | 2 (1.8%) | |
| Number of primaries melanomas, n (%) | 0.854 | |||
| Multiple primary melanomas | 27 (4.8%) | 22 (4.8%) | 5 (4.4%) | |
| Single primary melanoma | 541 (95.2%) | 433 (95.2%) | 108 (95.6%) | |
| Breslow, median (IQR) | 2.7 (1.3–5.0) | 2.8 (1.3–5.0) | 2.0 (1.0–4.2) | 0.021 |
| Missing | 5 | 4 | 1 | |
| Ulceration, n (%) | 0.109 | |||
| Absent | 290 (52.3%) | 225 (50.6%) | 65 (59.1%) | |
| Present | 265 (47.7%) | 220 (49.4%) | 45 (40.9%) | |
| Missing | 13 | 10 | 3 | |
| Mitotic index mm2, n (%) | 0.743 | |||
| ≥1 mitosis | 316 (73.5%) | 254 (73.8%) | 62 (72.1%) | |
| 0 mitosis | 114 (26.5%) | 90 (26.2%) | 24 (27.9%) | |
| Missing | 138 | 111 | 27 | |
| Histological subtype, n (%) | 0.092 | |||
| Acral lentiginous | 502 (88.4%) | 397 (87.3%) | 105 (92.9%) | |
| Nodular | 66 (11.6%) | 58 (12.7%) | 8 (7.1%) | |
| Satellitosis, n (%) | 0.096 | |||
| Absent | 541 (95.2%) | 430 (94.5%) | 111 (98.2%) | |
| Present | 27 (4.8%) | 25 (5.5%) | 2 (1.8%) | |
| Associated nevus, n (%) | 0.011 | |||
| De novo melanoma | 307 (91.4%) | 233 (89.3%) | 74 (98.7%) | |
| Nevus-associated melanoma | 29 (8.6%) | 28 (10.7%) | 1 (1.3%) | |
| Missing | 232 | 194 | 38 | |
| Sentinel lymph node biopsy, n (%) | 0.256 | |||
| Direct lymphadenectomy | 17 (3.2%) | 16 (3.8%) | 1 (0.9%) | |
| Not indicated | 102 (19.2%) | 76 (17.9%) | 26 (24.3%) | |
| SLNB not performed | 94 (17.7%) | 77 (18.1%) | 17 (15.9%) | |
| SLNB performed | 319 (60.0%) | 256 (60.2%) | 63 (58.9%) | |
| Missing | 36 | 30 | 6 | |
| Sentinel lymph node biopsy status, n (%) | 0.012 | |||
| Affected | 93 (27.6%) | 82 (30.7%) | 11 (15.7%) | |
| Not affected | 244 (72.4%) | 185 (69.3%) | 59 (84.3%) | |
| Missing | 231 | 188 | 43 | |
Data are expressed as No. (%) unless otherwise indicated; IQR, interquartil range; AJCC, American Joint Committee on Cancer.
Considering the whole series, all cases were histopathologically categorized as ALM (N=666, 90.9%) and NM (N=67, 9.1%), with the foot melanoma group having more NM (10.4% vs 4.8%; p=0.030). The hand melanoma group had more in situ and stage I cases (59.2% vs 43.7% on feet; p<0.001), while the foot melanoma group had more advanced cases at diagnosis (stages III and IV) (24.8% vs 11.7%; p<0.001). Significant differences were observed regarding the number of invasive cases when foot and hand tumors were compared (80.8% vs 69.8%, respectively; p=0.003). Overall, 42 patients (5.7%) exhibited multiple primary melanomas, while only 3 patients of this cohort developed>1 acral melanoma. Moreover, foot melanomas had a higher percentage of nevus-associated melanoma vs the hand melanoma group (15.9% vs 1.0%; p<0.001).
Histopathological features of invasive melanomasRegarding invasive melanomas, the hand melanoma group had a higher percentage of stage I and II melanomas (83.2% vs 69.2%; p=0.014). Median Breslow of the series was 2.7mm (IQR, 1.3–5.0) with the foot melanoma group having thicker Breslow depth [2.8mm (IQR, 1.3–5.0) vs 2.0mm (IQR, 1.0–4.2); p=0.021)]. Ulceration was present in 47.7% of all cases; no significant differences were detected between hand and foot acral melanoma. The distribution of the histological subtypes was 88.4% for ALM and 11.6% for NM, with no differences being reported between hand and foot acral melanoma. Foot melanomas had a higher percentage of nevus-associated melanoma vs the hand melanoma group (10.7% vs 1.3%; p=0.011). Regarding stage III patients, we observed that 93 patients (64.1%) were diagnosed via SLNB and 52 cases (35.9%) via visible locoregional disease at the time of diagnosis. SLNB was performed in 319 cases (60%) with affected status in 93 cases (27.6%). A statistically significant difference in SLNB status was observed with a higher number of positive SLNB in the foot melanoma group (30.7% vs 15.7%; p=0.012).
Survival analysisOverall, the 5-year MSS rate was 71.5% (95%CI, 67.4–75.8). These survival rates were 69.1% (95%CI, 64.6–74.0) for the foot group and 81.2% (95%CI, 73.1–90.2) for the hand melanoma group. Overall, the 5-year RFS rate was 61.8% (95%CI, 57.5–66.5); 59.5% (95%CI, 54.6–64.8) for the foot group and 70.9% (95%CI, 61.4–81.6) for the hand melanoma group. The Kaplan–Meier curves showed that foot melanomas had statistically significant lower MSS (p=0.019) and RFS rates (p=0.011) vs hand melanomas. In this series, no patients with in situ melanoma died of melanoma-related deaths. The results are shown in Fig. 1.
Univariate Cox regression analysis of MSS showed that foot location of melanoma, later age of onset, male gender, thicker Breslow depth, presence of ulceration and nodular melanoma subtype were associated with worse prognosis.
The multivariate Cox regression analysis confirmed that later age of onset (>75 years; HR, 1.61; 95%CI, 1.05–2.46; p=0.030), and thicker Breslow depth (>1.0–2mm; HR, 5.85; 95%CI, 1.76–19.45; p=0.004; >2.0–4mm; HR, 11.18; 95%CI, 3.41–36.70; p<0.001; >4mm; HR, 14.20; 95%CI, 4.28–47.06; p<0.001) were independent predictors of worse MSS.
Regarding RFS, the overall 5-year RFS rate was 61.8% (95%CI, 57.5–66.5) with 5-year RFS rates of 59.5% (95%CI, 54.6–64.8) for the foot group and 70.9% (95%CI, 61.6–81.6) for the hand melanoma group. Univariate Cox regression analysis showed that foot location of melanoma, thicker Breslow depth, presence of ulceration and nodular melanoma subtype were associated with worse RFS. Nevertheless, multivariate regression models found that only Breslow depth (>1.0–2mm; HR, 3.91; 95%CI, 1.62–9.45; p=0.002; >2.0–4mm; HR, 7.68; 95%CI, 3.23–18.29; p<0.001; >4mm; HR, 10.12; 95%CI, 4.19–24.41; p<0.001) and the presence of ulceration (HR, 1.57, 95%CI 1.11–2.22; p=0.011) were independent risk factors of RFS.
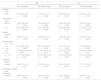
Data associated with univariate and multivariate Cox regression models for MSS and RFS are shown in Table 3.
Univariate and multivariate Cox regression analysis of melanoma-specific survival (MSS) and relapse-free survival (RFS).
| MSS | RFS | |||
|---|---|---|---|---|
| HR (univariable) | HR (multivariable) | HR (univariable) | HR (multivariable) | |
| Location | ||||
| Foot | • | • | • | • |
| Hand | 0.59 (0.37–0.92, p=0.020) | 0.70 (0.44–1.12, p=0.139) | 0.59 (0.39–0.89, p=0.012) | 0.72 (0.47–1.09, p=0.119) |
| Age (tertiles) | ||||
| <58.3 | • | • | • | • |
| 58.3–75 | 1.64 (1.08–2.48, p=0.019) | 1.43 (0.94–2.18, p=0.099) | 1.29 (0.90–1.86, p=0.166) | 1.03 (0.71–1.49, p=0.882) |
| >75 | 2.02 (1.33–3.06, p=0.001) | 1.61 (1.05–2.46, p=0.030) | 1.40 (0.96–2.02, p=0.077) | 1.17 (0.81–1.70, p=0.410) |
| Gender | ||||
| Female | • | • | • | • |
| Male | 1.58 (1.17–2.15, p=0.003) | 1.28 (0.94–1.76, p=0.122) | 1.29 (0.97–1.72, p=0.075) | 1.03 (0.77–1.39, p=0.819) |
| Breslow depth | ||||
| ≤1.0mm | • | • | • | • |
| >1.0–2mm | 5.31 (1.85–15.21, p=0.002) | 5.85 (1.76–19.45, p=0.004) | 3.41 (1.57–7.41, p=0.002) | 3.91 (1.62–9.45, p=0.002) |
| >2.0–4mm | 11.95 (4.32–33.10, p <0.001) | 11.18 (3.41–36.70, p<0.001) | 7.81 (3.74–16.31, p<0.001) | 7.68 (3.23–18.29, p<0.001) |
| >4mm | 17.77 (6.51–48.50, p<0.001) | 14.20 (4.28–47.06, p<0.001) | 11.44 (5.54–23.61, p<0.001) | 10.12 (4.19–24.41, p<0.001) |
| Ulceration | ||||
| Absent | • | • | • | • |
| Present | 2.94 (2.11–4.10, p<0.001) | 1.37 (0.94–1.99, p=0.100) | 3.14 (2.31–4.27, p<0.001) | 1.57 (1.11–2.22, p=0.011) |
| Histological subtype | ||||
| Acral lentiginous | • | • | • | • |
| Nodular | 2.08 (1.42–3.07, p<0.001) | 1.22 (0.81–1.84, p=0.348) | 1.52 (1.02–2.27, p=0.040) | 0.86 (0.57–1.31, p=0.490) |
HR, hazard ratio
For the recurrence pattern, the median time to the index metastasis was 1.74 years (IQR, 1.48–2.17) (Fig. 2). Most patients (81.7%) who recurred developed the first metastasis within the first 4 years of follow-up.
A total of 202 patients (27.7%) developed recurrences after a mean follow-up of 100 months. The most common site of relapse was locoregional (n=121; 59.9%), while 81 patients (40.1%) developed distant metastases. For the location of the index metastasis, Kaplan–Meier curves showed that distant metastases appeared earlier than locoregional metastases did (median time, 1.32 years (IQR, 1.12–1.87) vs 2.14 years (IQR, 1.68–2.70); p=0.015) (Fig. 2). Most distant metastases were pulmonary (34.6%), followed by hepatic (13.6%), associated with the central nervous system (12.3%), and distant lymphatic (12.3%) metastases. The distribution of the index metastases is illustrated in Fig. 3.
DiscussionAs far as we know, the present 20-year retrospective study of acral melanoma in Europe is the largest series conducted in a predominantly white population.
Melanoma on the acral regions affects all populations worldwide. However, represents a significant number of cases (20% up to 70%) in countries with a lower incidence of sun-related melanoma, such as those in Asian, African, and Latin American regions.8,16–19 Given its importance, most studies on acral melanoma focus on non-Caucasian populations.
Acral melanoma is a rare entity with distinctive peculiarities associated with poorer prognosis vs cutaneous melanoma found in different locations.2,6,10,11,20,21 This adverse prognosis has been attributed to several factors, as mentioned. In our cohort, a significant number of cases were diagnosed with thicker Breslow depth, high prevalence of ulceration and advanced stages, as most studies reported.2,6,10–12,21,22 Notably, 21.9% of our cohort was diagnosed with non-localized AJCC 8th edition stage disease (stage III and IV), which is consistent with other series.6,21,23 This percentage of non-localized stages is considerably higher than that of the series of non-acral melanomas.11 Moreover, acral melanoma is associated with older age and most cases occurred on the feet, as we have already seen.2,6,10–12,20,22,24 These findings collectively suggest a notable delay in diagnosis, predominantly attributed to the less conspicuous location of melanomas, such as the feet, a factor that is particularly pertinent in older populations, as proposed by other authors.2,4,10–15Overall, about 20% up to 30% of melanomas are originated from a melanocytic nevus precursor.25–27 Nevus-associated melanomas have been associated with a younger age at diagnosis, higher nevus counts, thinner melanomas, and intermittently sun-exposed body locations such as the trunk. Histopathologically, they develop SSM and harbor BRAF mutations.25–27 It is remarkable that in our population the prevalence of nevus-associated melanomas was only 1% on the hand melanoma group and 16% on the foot melanoma group, which could be explained by the relatively older population of the cohort, the absence of SSM and the low incidence of BRAF mutations that acral melanomas tend to associate. Moreover, a few studies on ALM have indicated that melanomas tend to occur in areas of the hands and feet prone to mechanical stress.22,28–31 Pressure, trauma and physical stress on the feet could play a role in the pathogenesis of nevus-associated melanomas and explain the differences between hand and foot melanoma group.
Histological subtype and melanoma location have been a matter of discussion regarding their impact on prognosis. Some studies suggest that ALM or acral melanoma location are associated with a poorer prognosis2,6,10,11,20,21 while other indicate that their prognosis is similar to that of other melanoma subtypes and locations.4,12,22–24,32,33 In our series, when comparing hands vs feet melanomas, we observed that melanomas on the feet exhibited thicker Breslow depths, more prevalent SLNB involvement, and higher AJCC 8th edition stages. However, the location of melanoma and its histopathological subtype were not associated with poorer prognosis in terms of MSS or RFS. Thicker Breslow depth and later age of onset (>75 years) were the only independent prognostic factors for MSS, while thicker Breslow depth and ulceration were independent risk factors for RFS.
Former studies suggest that there could be differences in the dynamics of metastatic spread between acral and non-acral melanoma, particularly in terms of higher rates of both recurrence and distant metastases in acral melanoma.2,6,10,12,34–43 Moreover, it has been reported that risk factors for lymphatic or hematogenous metastases may vary,44,45 where thicker Breslow depths have been reported as a predictor for hematogenous metastases.45 Furthermore, patients with earlier stages developed relapses later than those with more advanced stages, which was clearly marked in distant metastasis.42,46,47 In our research, we observed a high rate of melanoma relapses with predominance of locoregional metastases; however, a significant proportion of cases also developed distant metastases. Notably, distant metastases showed earlier than locoregional metastases and did so in a shorter period of time vs other series published to this date,42,48–50 which could be explained by the thick Breslow depths reported in the study leading to a major risk for distant and earlier metastasis. As far as we know, there are no other specific studies on this phenomenon in acral melanoma series. These observations underscore the complexity and variability of the metastatic behavour of melanomas and highlight the importance of considering routine imaging modalities to detect asymptomatic recurrences or metastases 3–5 years after diagnosis, depending on the risk of relapse, according to the National Comprehensive Cancer Network (NCCN) guidelines.51
This study has the limitations inherent to its retrospective design. However, data were prospective and multicentrically collected. There are missing values in significant data points, such as the exact location on acral zones, the socioeconomic factors, the genetic testing of the tumors, and the margins obtained in melanoma-related surgical procedures. In the case of recurrences, we did not explore whether these patients developed synchronous metastases or subsequent distant metastases in patients initially presenting with locoregional metastases. Due to the heterogeneity of surgical procedures and systemic therapies throughout 2 decades, we did not delve into the outcomes based on the therapies received.
In conclusion, we present the largest study conducted on acral melanomas in a predominantly Caucasian population. A significant number of cases were diagnosed with thick Breslow depth, high prevalence of ulceration, advanced stages and low prevalence of nevus-associated melanomas. Melanomas originating on the feet were later detected—were more associated with nevus—had a higher proportion of nodular subtype, and more advanced AJCC 8th edition stages vs those arising on the hand. Thicker Breslow depth and later age of onset were independent prognostic factors for MSS, while thicker Breslow depth and ulceration were independent risk factors for RFS. Melanoma location and histopathological subtype were not associated with a poorer prognosis. Recurrences were a common finding, with distant metastases appearing earlier than locoregional recurrences, which highlights the importance of intensive follow-up and routine imaging modalities to monitor asymptomatic recurrences.
FundingMelanoma research at Hospital Universitari Arnau de Vilanova of Lleida was supported by grants from ISCIII/FEDER “Una manera de hacer Europa” (PI18/00573 & PI21/00294 to R.M. Marti), CIBERONC-CB16/12/00231, and Generalitat de Catalunya (2021/SGR0093). The research at the Melanoma group in Hospital Clinic Barcelona is supported by the CIBER de Enfermedades Raras of the Instituto de Salud Carlos III, Spain; AGAUR 2017_SGR_1134 and CERCA Programme by Generalitat de Catalunya, Spain; a Research Grant from “Fundación Científica de la Asociación Española Contra el Cáncer” GCB15152978SOEN, Spain; European Commission under the sixth Framework Programme, Contract No. LSHC-CT-2006-018702 (GenoMEL), by the European Commission under the seventh Framework Programme, Diagnoptics; the European Commision under the HORIZON2020 Framework Programme, iTobos and Qualitop; and European Commission under the Horizon Europe Programme, HORIZON-MISS-2021-CANCER-02, MELCAYA (reference 101096667). This research was in part supported by grants from Fondo de Investigaciones Sanitarias P.I. 18/00419 and 22/01467 Spain. Part of the work was carried out at the Esther Koplowitz Center, Barcelona. J. Angel-Baldo held a predoctoral fellowship from IRBLleida/Diputació de Lleida.
Conflict of interestsThe authors state that they have no conflict of interests.
Thanks to our patients and their families who are the main reason for our studies. Special thanks to all fellows and residents who contributed to keep updated our Network Database in daily clinical practice.
Clara Matas-Nadal, Xavier Soria, Sonia Gatius, Felip Vilardell (Hospital Universitari Arnau de Vilanova, Lleida), Inma Gil, Cristina Grau, Fani Martínez (Hospital Universitari Sant Joan de Reus), Nelson Lobos (Hospital Clínic de Barcelona, Barcelona), Oriol Yélamos, Joan Dalmau (Hospital de la Santa Creu i Sant Pau, Barcelona), Carlos González-Cruz, Helena Hilari (Hospital Universitari Vall d’Hebrón), Paola Pasquali (Pius Hospital de Valls), Marc Sagristà (Hospital de Calella), María Rosa Olivella-Garcés (Hospital Moisès Broggi, Consorci Sanitari Integral, Sant Joan Despí), Montserrat Bonfill-Ortí, Josep Ramón Ferreres (Hospital Universitari de Bellvitge), Ane Jaka, Ariadna Quer, Nina Richarz (Hospital Universitari Germans Trias i Pujol, Badalona), Inés Zarzoso Muñoz, Emili Masferrer (Hospital Universitari Mútua Terrassa), Pedro Zaballos (Hospital Sant Pau i Santa Tecla, Tarragona), Manel Formigon (Consorci Sanitari de Terrassa), Loida Galvany (Hospital Dos de Maig), Marta Alegre (Hospital Plató, Barcelona), Anna Sánchez-Puigdollers, Nerea Mohino-Farré (Hospital Joan XXIII, Tarragona).
The members of the Melanoma Centers Network of Catalonia are presented in Appendix 1.