In pustular psoriasis, hypocalcemia is viewed as the consequence of the dermatosis rather than being recognized as a trigger.1 In the other clinical presentations of psoriasis, hypocalcemia is not usually described, and the relationship between hypocalcemia and psoriasis flares is unclear.
An interesting aspect of this relationship is the observation of the dynamics of hypocalcemia remediation on the clinical remission of psoriasis. We report the case of a patient with surgical hypoparathyroidism in whom severe hypocalcemia precipitated typical pustular psoriasis of von Zumbusch which improved with calcium supplementation alone.
Case reportA 60 years old female patient, admitted in our structure for erythroderma. Her past medical history was related to a total thyro-parthyroidectomy 5 years ago complicated by hypocalcaemia, with irregular use of levothyroxine and calcium supplementation. This erythroderma which evolved since six weeks was associated with unmeasured fever, resting tremor, tetanies crises, dyspnea and a decrease in her general state of health.
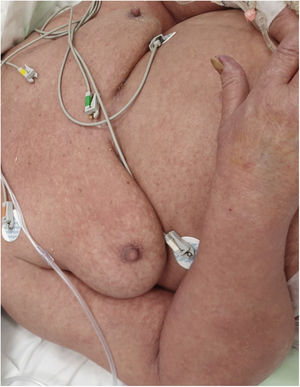
On admission, the patient was in a regular general state of health, feverish at 38.5 with sinus tachycardia, and discrete tachypnea. Physical examination revealed diffuse crackles and wheezing, resting tremor of the hands with positive trousseau and chvostek signs. The skin showed edematous erythroderma with diffuse pustular lesions (Fig. 1).
The laboratory examinations showed inflammatory syndrome with, elevated C-reactive protein (CRP) of 210mg/L, erythrocyte sedimentation rate of 150mm/h and inflammatory anemia. Severe hypocalcemia (total calcium 3.5mEq/dl). Albumin, liver enzymes, renal function and urinalysis were normal. The hormonal assessment had shown hypothyroidism with TSH at 10.1μIU/ml, free T4 at 1.3ng/dl and hypoparathyroidism with parathyroid hormone=5pg/ml.
A skin biopsy was per-formed for diagnostic purpose, with histopathological findings consistent with pustular psoriasis.
Correction of the serum calcium improved the severe skin lesions and no specific treatment was necessary, emphasizing that fluctuations in serum calcixim affect psoriasis (Fig. 2).
DiscussionCalcium has a role in keratinocyte differentiation and proliferation, and cell adhesion requires cadherins, which are calcium-dependent molecules but the mechanism operating between calcium and keratinocyte differentiation is not fully understood.2 The association between psoriasis and hypocalcemia is known, especially in pustular psoriasis.1,3 There are two hypotheses which can explain this association. It has been suggested that calcium homeostasis could be involved in the development or exacerbation of psoriasis, since hypocalcemia can damage cell adhesion molecules.1,4 In the other hand Hypocalcemia can be secondary to the extensive cutaneous inflammation resulting from an extravasation of albumin and albumin-bound calcium into the interstitial space.1,4 In our case, hypocalcemia appears to be a relevant factor in inducing this psoriasis flare because hypocalcemia was present before the psoriasis and correction of the serum calcium improved the severe skin lesions.
The link between calcium supplementation and improvement of pustular psoriasis has been reported previously.1,3–5 In some cases calcium supplementation alone was sufficient and in others correction of hypocalcemia brought improvement but specific treatment was subsequently necessary.
ConclusionWe illustrate through this observation the direct role of hypocalcemia in triggering pustular psoriarisis in genetically predisposed patients, but the exact mechanism is still poorly understood given the low number of cases reported in the literature.
Conflict of interestThe authors declare that they have no conflict of interest.