We review the current treatments available for superficial mycoses and discuss recent developments in pharmacotherapy and the most useful adjuvant treatments. Special emphasis is placed on the proper use of conventional therapies and a number of pharmacoeconomic issues. The review also offers an update on the best treatment choices in particular circumstances. Finally, we discuss some novel contributions found in the literature.
Se revisa la terapéutica disponible actualmente para el tratamiento de las micosis superficiales, las novedades existentes en el campo de la quimioterapia y los tratamientos coadyuvantes más útiles en este terreno. Se hace especial hincapié en el adecuado uso de los tratamientos convencionales y en algunos aspectos farmacoeconómicos relacionados con el tema. Se actualizan los procedimientos terapéuticos más adecuados en circunstancias especiales. Finalmente, se discuten algunas aportaciones novedosas encontradas en la literatura revisada.
Treatment review articles usually focus on recently investigated drugs. However, these new drugs are sometimes of little use in routine clinical practice because they are not first-line options. In Spain, as in the rest of Europe, the most common mycoses are pityriasis versicolor,1 the various clinical forms of dermatophytosis,2–4 and candidiasis. In this review of current treatments, we focus on these 3 groups of mycoses and their first-line treatments.
Our aim is to answer several questions: Are any new treatments available for superficial mycoses? Are new treatments needed, or are the conventional treatments adequate? And finally, do we make good use of the available resources, or do we need to be more efficient in our treatment of superficial mycoses?
What is needed, we believe, is not merely a list of recently developed treatments but a review of ways to improve clinical outcomes through the proper use of conventional drugs. We also believe that costs can be reduced without sacrificing outcome quality.
We draw on our personal experience as well as evidence from 3 types of publications: experimental research, clinical trials, and pharmacoeconomic studies.
In routine clinical practice, the treatment of superficial mycoses with antifungals differs from that of infections treated with antibiotic therapy in that susceptibility testing is only useful in infections caused by Candida organisms.5,6 In the case of other yeasts, such as Malassezia7 and dermatophytes,8 susceptibility tests are difficult to perform, poorly standardized, and purely of academic interest.
Available Treatments Are Well Known But Poorly UsedSince the appearance of griseofulvin and the polyenes in the 1950s, the pharmacopeia for superficial mycoses has seen the addition of topical treatments, such as the azoles, ciclopirox, and amorolfine as well as the oral triazoles and allylamines. Around 60 new antifungal substances are currently being investigated. These include new formulations and semisynthetic derivatives of polyenes and amphotericin, new peptides such as echinocandins and aerothricines, and novel substances such as amino acids, sordarins, macrolides, terpenes, saponins, and flavans.9,10 Although many of these drugs have been tested against dermatophytes in the laboratory, the specialized products that have been brought to market are expensive and are not indicated for superficial mycoses, except in extreme cases or in a hypothetical future.11
Moreover, despite the large number of clinical trials of antifungal agents conducted over recent decades, we found that the meta-analyses on this topic include a strikingly small number of trials, suggesting a lack of homogeneity in the methodologies used.12–14 Review articles on this subject therefore invariably conclude by indicating that further studies are needed in the field of superficial mycoses.15
How Much Is Being Spent on Antifungal Agents in Spain?A similar situation can be seen in pharmacoeconomic studies on antifungal agents. The results of these studies vary greatly depending on their objectives (cost-effectiveness, cost-utility, cost-benefit), the sponsoring institution (public body or private company), time frame and geographic scope, type of cost evaluated (only the drug or the entire medical intervention), and outcome (cure or disease-free days).16 Pharmacoeconomic studies identify, one way or another, the least expensive treatment, but they do not clearly demonstrate the importance of choosing the least expensive option.17
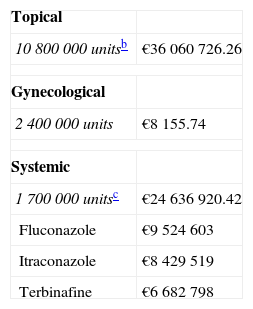
We requested data from the Spanish Ministry of Health for 2001, a year in which a complete census of Spain's population was conducted (Table 1). According to the data provided, 1 package of topical antifungal agent was used for every 4 people and 1 package of oral antifungal agent was used for every 24 people in the country in 2001. Although a more in-depth analysis is warranted,17 these data clearly suggest that antifungal agents are being overused in Spain.
Estimated Expenditure in Spain on Topical and Systemic Antifungal Agents, Based on Spanish Ministry of Health and Consumer Affairs Data From 2001 Provided in 2007.a
Recent studies of superficial mycoses have focused primarily on the best use of known resources,18 and on the search for efficacy enhancers, such as adjuvant therapies, for both topical and oral treatments.19,20
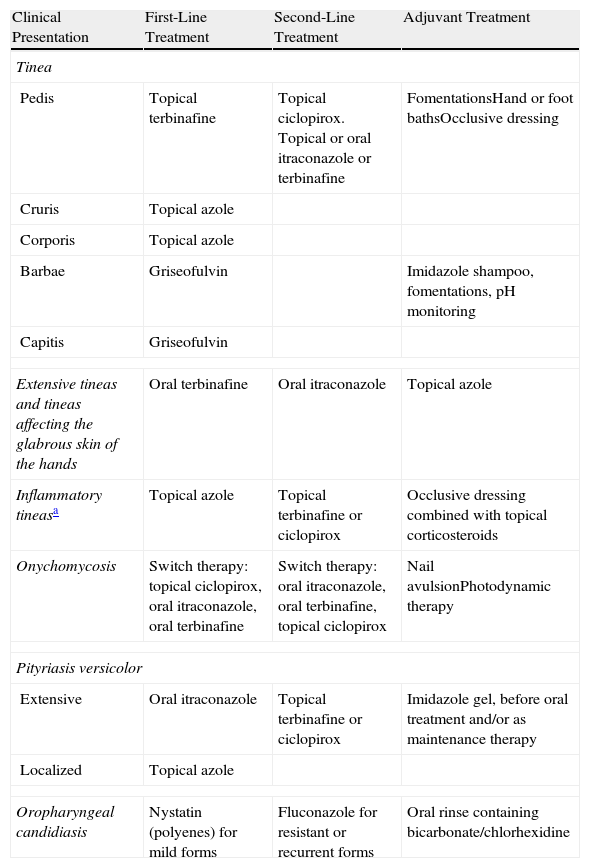
First-Line Treatments and Practical AspectsGriseofulvinFor more than 40 years, griseofulvin has been the first-line treatment for ringworm of the scalp in pediatric patients (Table 2).21–23 In that setting, griseofulvin is more effective than fluconazole and just as effective as itraconazole and terbinafine24 but much less expensive. The rate of adverse effects associated with griseofulvin is low and does not increase at high doses (15-20mg/kg/d in children).20,21 Current guidelines recommend continuing griseofulvin treatment for at least 6 weeks at a dose adjusted to body weight: in children weighing <10kg, the dose should not exceed 250mg/d; in patients weighing 10 to 20kg, the recommended dose is 375mg/d; in patients weighing 20 to 40kg, 500mg/d; and in patients weighing >40kg, 1000mg/d. Because the half-life of the drug is less than 24hours, the guidelines recommend administering the daily dose in 2 doses.20,21
First-Line Treatments and Adjuvant Therapies.
| Clinical Presentation | First-Line Treatment | Second-Line Treatment | Adjuvant Treatment |
| Tinea | |||
| Pedis | Topical terbinafine | Topical ciclopirox. Topical or oral itraconazole or terbinafine | FomentationsHand or foot bathsOcclusive dressing |
| Cruris | Topical azole | ||
| Corporis | Topical azole | ||
| Barbae | Griseofulvin | Imidazole shampoo, fomentations, pH monitoring | |
| Capitis | Griseofulvin | ||
| Extensive tineas and tineas affecting the glabrous skin of the hands | Oral terbinafine | Oral itraconazole | Topical azole |
| Inflammatory tineasa | Topical azole | Topical terbinafine or ciclopirox | Occlusive dressing combined with topical corticosteroids |
| Onychomycosis | Switch therapy: topical ciclopirox, oral itraconazole, oral terbinafine | Switch therapy: oral itraconazole, oral terbinafine, topical ciclopirox | Nail avulsionPhotodynamic therapy |
| Pityriasis versicolor | |||
| Extensive | Oral itraconazole | Topical terbinafine or ciclopirox | Imidazole gel, before oral treatment and/or as maintenance therapy |
| Localized | Topical azole | ||
| Oropharyngeal candidiasis | Nystatin (polyenes) for mild forms | Fluconazole for resistant or recurrent forms | Oral rinse containing bicarbonate/chlorhexidine |
Imported cases of ringworm caused by Trichophyton tonsurans may be resistant to griseofulvin and require treatment with terbinafine. The likelihood of adverse reactions is very low and this possibility should only be taken into consideration in patients with a history of serious adverse reactions to other drugs.14
The efficacy of griseofulvin can be improved significantly by the simultaneous ingestion of fatty foods, which stabilize the gastric pH, and by the application of fomentations because local heat and moisture cause sweating, which in turn enhances the transcutaneous excretion of the drug.21
Oral TriazolesFluconazole is the first-line treatment for recurrent cases of oropharyngeal and genital candidiasis25 that respond poorly to topical treatments, and for severe subcutaneous and systemic mycoses (Table 2).26,27 It is the third-line treatment for tinea infections that affect terminal hair and/or the nails (onychomycosis) in adults. Failed candidiasis treatments are more often associated with incorrect administration than with resistance.18,19 The treatment of candidiasis should always be accompanied by dietary and hygiene measures, ranging from conventional iron metabolism monitoring to changes in eating habits.25,28 Itraconazole could be considered the German Shepherd of oral antifungal agents because it is second-best at nearly everything. It is better than terbinafine, though not as effective as griseofulvin, in the treatment of mycoses caused by Microsporum canis. It is the first-line monotherapy for extensive pityriasis versicolor (Table 2). Itraconazole is also used to reduce the cost of switch therapy for onychomycosis, as will be explained below (Table 3). The pharmacokinetic problems of itraconazole will probably be improved in the new formulation that is currently being tested.29,30
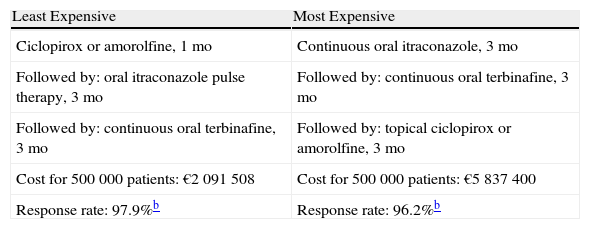
Switch Therapy for Onychomycosis: Comparison of Net Cost Per 500 000 Patients.a
| Least Expensive | Most Expensive |
| Ciclopirox or amorolfine, 1 mo | Continuous oral itraconazole, 3 mo |
| Followed by: oral itraconazole pulse therapy, 3 mo | Followed by: continuous oral terbinafine, 3 mo |
| Followed by: continuous oral terbinafine, 3 mo | Followed by: topical ciclopirox or amorolfine, 3 mo |
| Cost for 500 000 patients: €2 091 508 | Cost for 500 000 patients: €5 837 400 |
| Response rate: 97.9%b | Response rate: 96.2%b |
The topical azoles are a large, well-known group of substances to which new products are continually being added. Topical azole treatments are cheap, potent, and broad-spectrum, with activity against dermatophytes, molds, and yeasts (Table 2). The absorption and, therefore, the effectiveness of topical azoles can be increased with the application of occlusive dressings. The use of topical azoles in combination with topical corticosteroids has been recommended in the treatment of inflammatory tineas. The addition of a topical corticosteroid enhances efficacy by decreasing the inflammatory component, facilitating the restoration of the skin's barrier function and normal flora, and diminishing the Herxheimer reaction that sometimes occurs at the start of treatment.31 This combination should not be used to treat tineas caused by anthropophilic fungi because in such cases it can lead to the development of tinea incognito and Majocchi granulomas.18
AllylaminesIn adults, single-drug therapy with oral terbinafine is the first-line treatment for onychomycosis and extensive tineas that respond poorly to topical treatment (Table 2). In children, the use of oral terbinafine is limited to patients over 2 years of age with griseofulvin-resistant cases of T tonsurans. A regimen of 6 weeks is recommended for infections of the scalp or fingernails and of 12 weeks for onychomycosis of the toenails. The recommended regimen in the United States, which is based on the availability of scored 125mg tablets, calls for a) half a tablet daily for children weighing under 20kg, b) 1 tablet daily for children weighing 20 to 40kg, and c) 1 tablet twice daily for children weighing over 40kg.20
In Spain, oral terbinafine is sold in scored 250mg tablets and cannot therefore be prescribed to children weighing under 20kg.14,20,24 The role of oral terbinafine in switch therapy for onychomycosis is discussed below.
Topical terbinafine is the topical antifungal agent most effective against tinea pedis in young adults (Table 2); however, because it is more expensive than azoles, this drug has been relegated to the role of a rescue medication.32–34
Concerns regarding resistance in cases of M canis infection are inconsequential because infections caused by this microorganism tend to respond very well to griseofulvin.18
Morpholines and CiclopiroxMorpholines and ciclopirox are highly potent broad-spectrum drugs capable of penetrating both glabrous skin and nail plates. They are effective as monotherapy against white superficial onychomycosis and athlete's foot in older patients who are already taking multiple medications. They are also useful in switch therapy (Table 2). There have been reports of irritant reactions to these drugs, although most of these have been associated with excipients.35
Polyenes (Nystatin)Nystatin is highly effective against candidiasis of both the skin and the mucous membranes, even in cases that are resistant to fluconazole and all other azoles.36 Because of its good safety profile and the fact that most patients tolerate it well, nystatin is recommended for prolonged treatment (Table 2). In the United States, there have been reports of contact dermatitis associated with the topical excipients used in certain generic preparations.20
Recommendations for Reducing the Duration of Oral TreatmentLike the use of occlusive dressings, mentioned above, the use of switch therapy can significantly reduce the duration of systemic antifungal treatment. Switch therapy is particularly useful in elderly, immunodeficient, or polymedicated patients with onychomycosis or extensive mycosis of the terminal hair or glabrous skin. In switch therapy, topical antifungal treatment is initiated prior to the start of oral treatment.13,18–20,29
In patients with onychomycosis, the following procedure is recommended. Specimens should be obtained for direct examination and culture and a topical antifungal lacquer, to be applied once daily for 1 month, should be prescribed. After 1 month, depending on the results of the direct examination and culture, oral treatment may be initiated. Topical treatment should be enhanced by using fomentations or hand or foot baths to increase the permeability of the nail plate.29,30,37,38
The use of imidazole shampoo for at least 15 days prior to the start of a 7-day regimen of oral itraconazole can be effective against mycoses affecting hair-bearing areas as well as extensive pityriasis versicolor.20
In ringworm of the scalp, griseofulvin should be used at high doses for 6 weeks. The response rate increases considerably with the addition of fomentations and topical imidazole in a cream, solution, or shampoo.20,24 Noninflammatory trichophytic tineas in adults are treated with a continuous 1-month regimen of oral terbinafine plus the topical treatment described above (Table 2).24
Cost-Effectiveness in Specific SituationsThe most effective topical monotherapies for tineas, inflammatory or not, affecting hairless, glabrous, and inguinal skin in young adults are terbinafine and ciclopirox, while the least expensive are tolnaftate and undecylenic acid, both available in various presentations. However, we believe that topical azoles should be the first-line treatment because their efficacy is similar to that of terbinafine and ciclopirox but they are less expensive (Table 2). In order to increase drug penetration and effectiveness, shorten treatment duration, and prevent recurrence, the use of occlusive dressings, fomentations, and hand and foot baths is essential.20
As noted above, combination therapy with an azole and a topical corticosteroid is especially useful at the start of treatment against inflammatory ringworm, in the event of a Herxheimer reaction,31 and in patients who, on completion of treatment, present eczematous or irritative symptoms.20
Switch Therapy in OnychomycosisSwitch therapy is the first-line treatment approach in onychomycosis.9,13 The drugs used in a switch therapy regimen can be administered in different sequences, with little impact on the final efficacy but large variations in cost. It is important to focus not on the cost of treating a single patient but on the expenditure of a large group of doctors over many years. Table 3 shows the final cost for 500 000 patients of 2 regimens of similar efficacy, 1 significantly less expensive than the other.39
Another approach that reduces the cost of treating onychomycosis is oral pulse therapy, a method first used in the 1960s with griseofulvin.40,41 At present, pulse therapy with terbinafine is considered to be similar to continuous therapy in terms of efficacy and safety. The recommended regimens range from 500mg daily for the first week of each month for 3 months42 to 500mg daily for the first and third months of a 3-month regimen.43
Various topical response enhancers aimed at reducing the need for oral therapy in onychomycosis have been proposed.30 This group includes substances that enhance the penetration of the topical treatment into the nail, such as urea, urea hydrogen peroxide, salicylic acid, thioglycolic acid, acetylcysteine, 2-mercaptoethanol, 2-nonyl-1,3-dioxolane, keratinases, and phosphoric acid.29 Other methods used to increase nail penetration include abrasion of the nail surface by mechanical means or low-powered laser, total nail avulsion by laser, and conventional surgical avulsion.29,44
Recent studies have found no association between surgical avulsion and subsequent problems with nail regrowth, and no differences between total and partial avulsion.38,44 Outcomes improved, however, when surgical avulsion was accompanied by topical occlusive treatment until the nail had regrown completely. Overall, surgical avulsion was found to have similar efficacy to, and no advantage over, medical treatments.38,44
One of the most promising treatment options is photodynamic therapy. This technique is effective against mucocutaneous candidiasis,45–47 onychomycosis caused by Trichophyton rubrum,48–51 and extensive folliculitis caused by Pityrosporon organisms.52 The results of photodynamic therapy have, however, been less promising in cases of tinea cruris.53 We therefore believe that further studies are needed to determine dosages and treatment regimens.
Other alternatives for treating onychomycosis, such as boosted treatments54,55 and iontophoresis, are still in the experimental stage.56,57
ConclusionIn summary, we consider that the expenditure on topical and systemic antifungal agents in Spain is very high. Moreover, we believe that, in most cases, the proper use of conventional drugs makes the use of more expensive drugs unnecessary. In the case of onychomycosis, we believe that the use of the recommended switch therapy could lead to considerable savings.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pereiro Ferreirós Jr M, et al. Actualización en el tratamiento de las micosis cutáneas. Actas Dermosifiliogr. 2012;103:778-83.