Lipedematous alopecia (LA) is a rare, non-scarring acquired alopecia, that characterizes by an increasing in scalp thickness and that typically appears in women around the fourth decade. Its origin is still unknown. No trichoscopic features have been described in the literature and reports focusing on the ultrasound are scarce. We report the case of a patient with lipedematous alopecia with trichoscopic, magnetic resonance imaging and ultrasounds features.
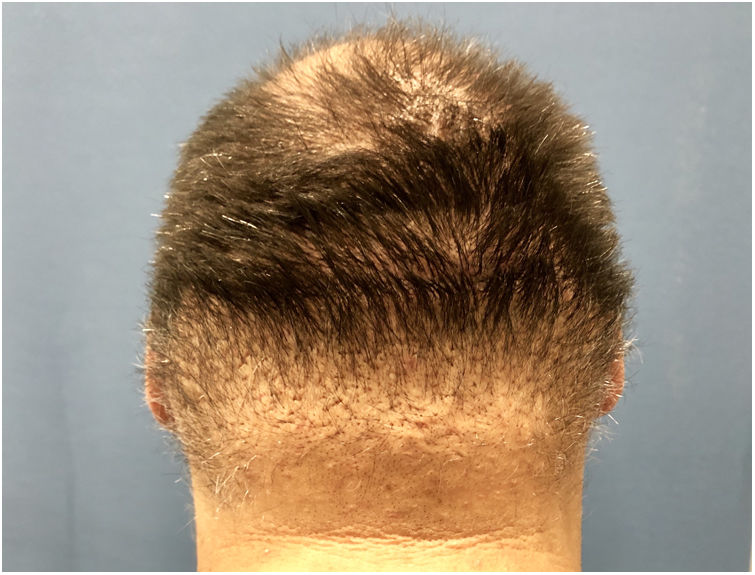
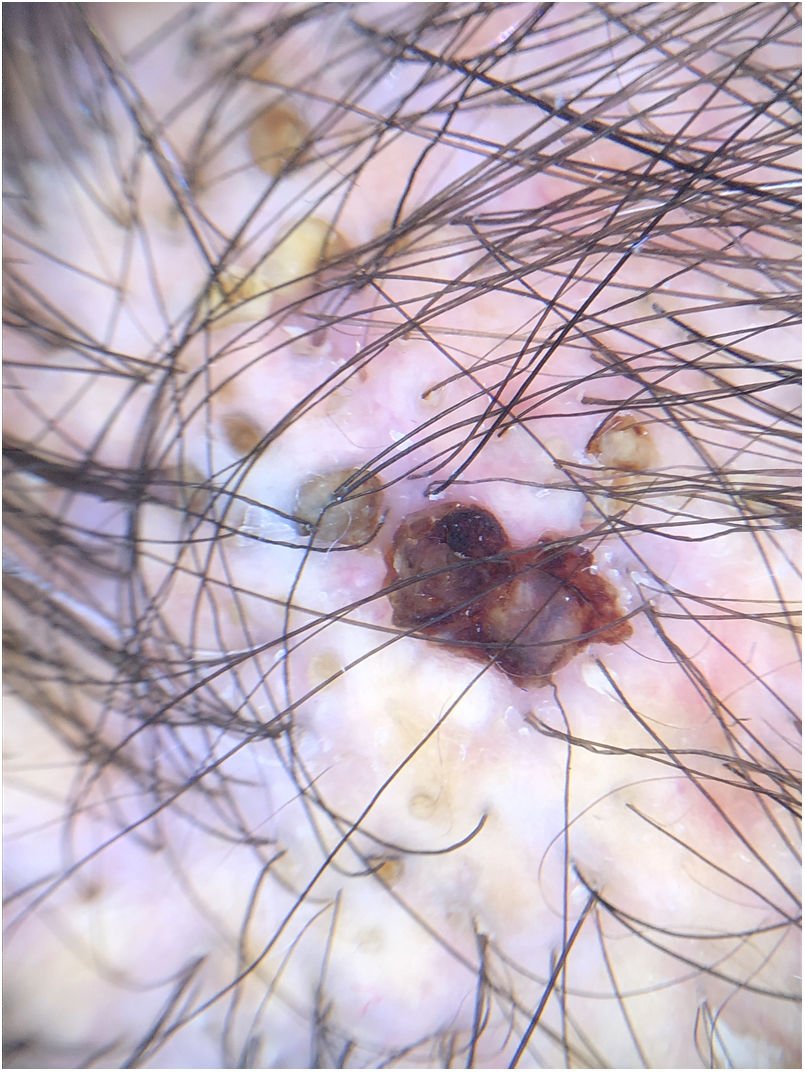
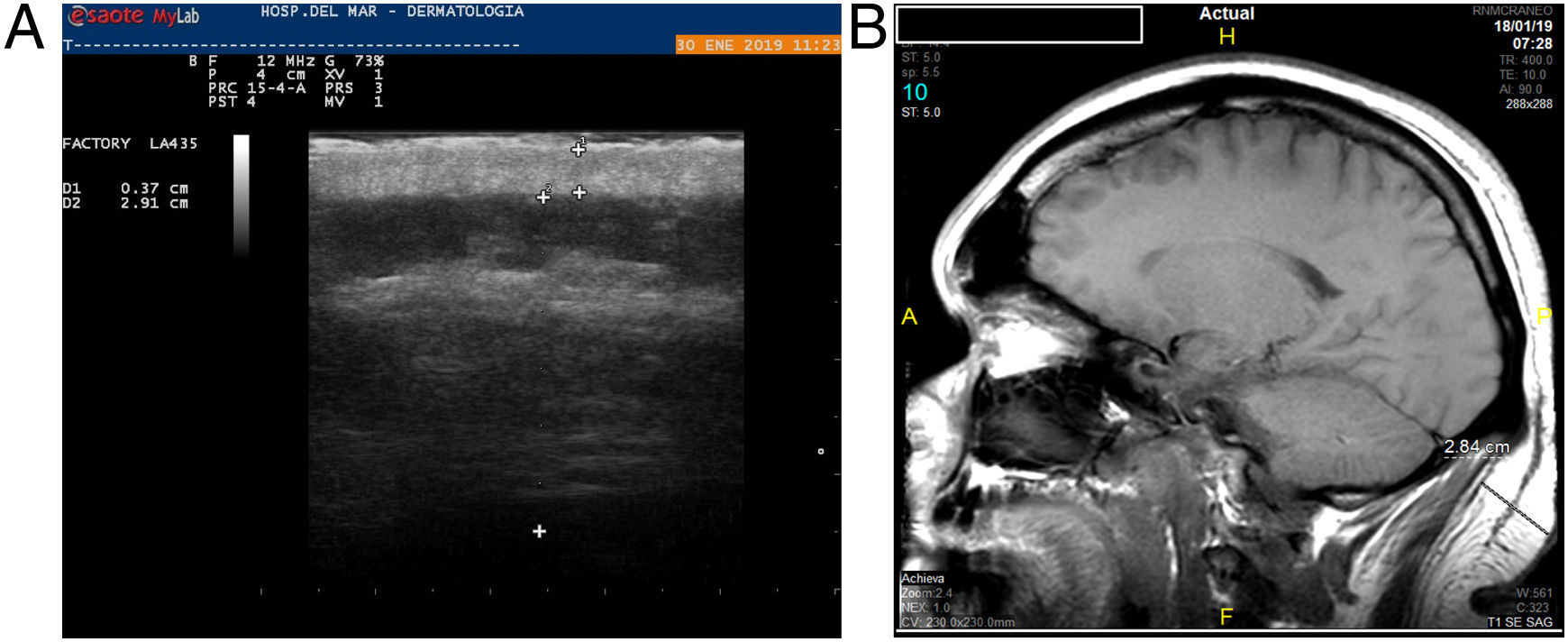
A 33-year-old man presented with many years of progressive hair loss. He had a mild mental retardation associated with epilepsy and he was treated with fluvoxamine and aripiprazole. He denied any history of trauma or surgery in the scalp. Physical examination revealed a diffusely thickened, boggy scalp, mainly localized in the occipital area, with no clinical signs of inflammation (Fig. 1). Androgenetic alopecia was associated with miniaturized hairs in the interparietal area. Trichoscopy revealed areas with big orange to yellow dots, five or more hairs emerging from a single follicle orifice similar to tufted follicles (Fig. 2). Hair pull test was negative. Scalp biopsy showed normal epidermis and dermis, with reduced anagen tufted hair follicles and a mild chronic perifollicular inflammation. No signs of fibrosis, dermal edema, mucin deposition, panniculitis or alterations in collagen bundles or elastic fibers were seen. Magnetic resonance imaging and ultrasounds of the scalp, showed an important difference in the thickness between the vertex and the occipital area, with the latter measuring more than 25mm. Ultrasounds showed a blurry interface between dermis and hypodermis and a striking asymmetric fatty tissue thickness increase was observed. Some areas of the hypodermis were seen into the dermis (Fig. 3A, B). The patient declined any treatments.
LA and lipedematous scalp, are two rare conditions of unknown etiology that are thought to correspond to the same spectrum of a single scalp disorder.1
A review of 47 cases published in 2012, found that 90% were white women with a mean age of 43 years,2 although LA has also been described as congenital.3 This is the main reason why female sexual hormones are thought to play a role in the pathogenesis of LA, but evidence is still lacking. Other theories support that an increase of pressure on the hair follicles from thickening of the subcutaneous fat layer, may cause impairment of the hair bulb and the follicular papilla. Leptin hormone, metaplasia and displacement of adipose tissue have also been postulated as playing a role in the development of LA.1
Pathologic defining criteria of LA include: thickened layer of mature subcutaneous fat with variable disruption of fatty architecture, no visible panniculitis or lipoma, no inflammation and normal hair follicles and adnexae. Von Gieson, Masson's trichrome, Periodic acid-Schiff or alcian blue and D2-40-podoplanin stainings may help to rule out any elastic fiber and collagen fibers alterations, dermal mucin deposition or lymphatic vessels alterations, respectively.2
Magnetic resonance imaging was one of the best imaging diagnostic methods and, as far as we know, ultrasounds have only been used once by Martin et al. for assessing LA.4 Regular mean thickness of scalp is considered to be 5–8mm.5 Both imaging tools may reveal a 9–19 increase in scalp thickness in LA. Cutis verticis gyrate, that is the main differential diagnosis, could be ruled out with this imaging technique because this entity is characterized for an increased thickness of the scalp dermis with furrows or convolutions with a cerebriform resemblance.6
No trichoscopic findings have been reported in the literature. We found bundles of tufted hairs made up of more than 5 hairs arising from single preserved hair follicles. We did not find any other relevant trichoscopic findings. Tufted hairs are the manifestation of a fibrosis-induced gathering of adjacent follicular structures, as well as a follicular retention of telogen phase hairs over multiple cycles.7 In this case, we think that the pressure on the hair follicles from thickening of the subcutaneous fat layer might induce the fusion of the follicular structures.
According to the treatment, our patient did not experience any changes due to his denial. In fact, there are no consensus or guidelines reported for the treatment of LA. Systemic and intralesional steroids, surgical intervention with debulking and scalp reduction and mycophenolate mofetil have been tried with variable improvements.8 Owing to the limited number of cases of LA and the diversity of efficacy rates, further clinical evidence is needed to reach a consensus for treatment of LA.
We present a case of LA with distinct trichoscopic and ultrasounds findings and we would like to remark the usefulness of ultrasounds and dermoscopy in an outpatient department as handy imaging tools in assessing and following-up of LA.
The patients in this manuscript have given written informed consent to publication of their case details.