We present the case of a 48-year-old heterosexual man who presented with a tuberous lesion of 1 month's duration on the penis. His personal history was remarkable for pulmonary tuberculosis 6 years earlier and an episode of herpes zoster with trigeminal nerve involvement 3 years earlier. The only symptom reported was occasional bleeding. He was not on immunosuppressant therapy and he denied sexual risk behavior and intravenous drug use. He had no past history of sexually transmitted disease.
Physical examination revealed a pink, round, pedunculated tumor with a soft consistency located in the balanopreputial sulcus. Of note was a hyperkeratotic component on the surface of the tumor (Fig. 1). The locoregional lymph nodes were not enlarged and there were no signs of oral mucosal involvement.
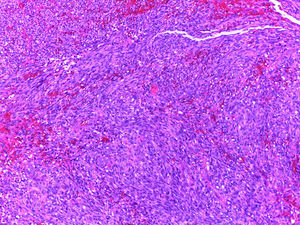
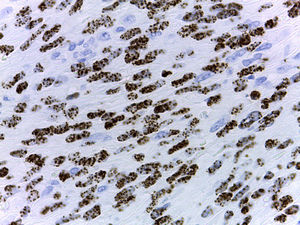
The histology study showed a proliferation of atypical spindle cells with an elongated nucleus, well-defined cytoplasm, and increased mitotic activity (Fig. 2). Immunohistochemistry showed CD31 positivity and intranuclear staining for human herpesvirus 8 (HHV-8) (Fig. 3). All these findings were consistent with a diagnosis of classic Kaposi sarcoma on the penis of a middle-aged, immunocompetent patient. Additional testing included blood tests with complete blood count, biochemistry, antinuclear antibodies, tumor markers, lymphocyte counts (B cells/type 1 helper (TH1) T cells/TH2 cells/natural killer [NK] cells), smears, β2-microglobulin levels, immunoglobulin counts, and viral serology tests (human immunodeficiency virus [HIV] 1, HIV-2, viral hepatitis A [VHA], VHC, VHB, HHV-6, HHV-7, HHV-8, Epstein-Barr virus, cytomegalovirus, human T-cell lymphotropic virus [HTLV] 1, HTLV-2, and varicella-zoster virus). All the results were normal, except for HHV-8 serology, which was positive. Computed tomography of the chest, abdomen, and pelvis showed no additional significant findings. The presence of an immunodeficiency disorder was ruled out in the immunology department.
The tumor was excised with disease-free margins, and the patient has not experienced any local recurrences or developed new lesions on other areas of the skin in 9 months of follow-up.
Kaposi sarcoma tumors are derived from endothelial cells. They follow a variable clinical course, ranging from minimal mucocutaneous involvement to systemic disease involving the internal organs. Disease progression varies according to the patient's origin, age, sex, and immune status. Four types of Kaposi sarcoma have been described: classic, endemic, iatrogenic, and HIV-related. Classic Kaposi sarcoma is typically more common in the Mediterranean region and Eastern Europe, and affects patients aged between 50 and 70 years. It occurs in both men and women, with reported male to female ratios ranging from 3:1 to 10:1, depending on the series. Skin lesions in classic Kaposi sarcoma are typically seen on the lower limbs, and penile involvement is very rare. Penile lesions are estimated to be the first manifestation of Kaposi sarcoma in 2% to 3% of patients with HIV infection and they are usually associated with a more aggressive course in this population.1 By contrast, according to reports in the English-language literature, just 15 cases of Kaposi sarcoma confined to the penis have been reported in HIV-negative patients in the past 20 years.2 In cases similar to ours (young patient with a history of a mycobacterial and herpes infection and classic Kaposi sarcoma), it is important to test T-cell (TH1, TH2), B-cell, NK-cell, and immunoglobulin levels to rule out a primary immunodeficiency disorder.3 To investigate the presence of secondary or acquired immunodeficiency, viral serology tests including HIV, HHV-8, HTLV-1 and 2, and Epstein-Barr virus, among others, should be performed, in addition to blood smears and tumor marker and antinuclear antibody tests.
The differential diagnosis should include pyogenic granuloma, molluscum contagiosum, genital warts, and Bowenoid papulosis.4 Bacillary angiomatosis should also be investigated in patients with multiple lesions. Local surgical excision is indicated in cases like ours that involve small, solitary lesions. Good results have also been described for intralesional vinblastine, cryotherapy, electrocoagulation, laser therapy, radiation therapy, intralesional interferon alfa and beta, photodynamic therapy, nitrogen mustards, and imiquimod. Chemotherapy and radiation therapy tend to be reserved for cases involving extensive lesions or internal organ involvement.5,6
Please cite this article as: Miguel-Gómez L, Pérez-Gala S, Jaén-Olasolo P. Lesión tuberosa en el pene. Actas Dermosifiliogr. 2015;106:680–681.