Livedoid vasculopathy (LV) is a noninflammatory thrombotic disease that affects the small blood vessels of the skin and is characterized by livedo racemosa and painful skin ulcers on the lower extremities.1,2 We report 2 cases of LV in which treatment with rivaroxaban achieved a full and sustained response. We also review novel oral anticoagulants with potential applications in dermatology.
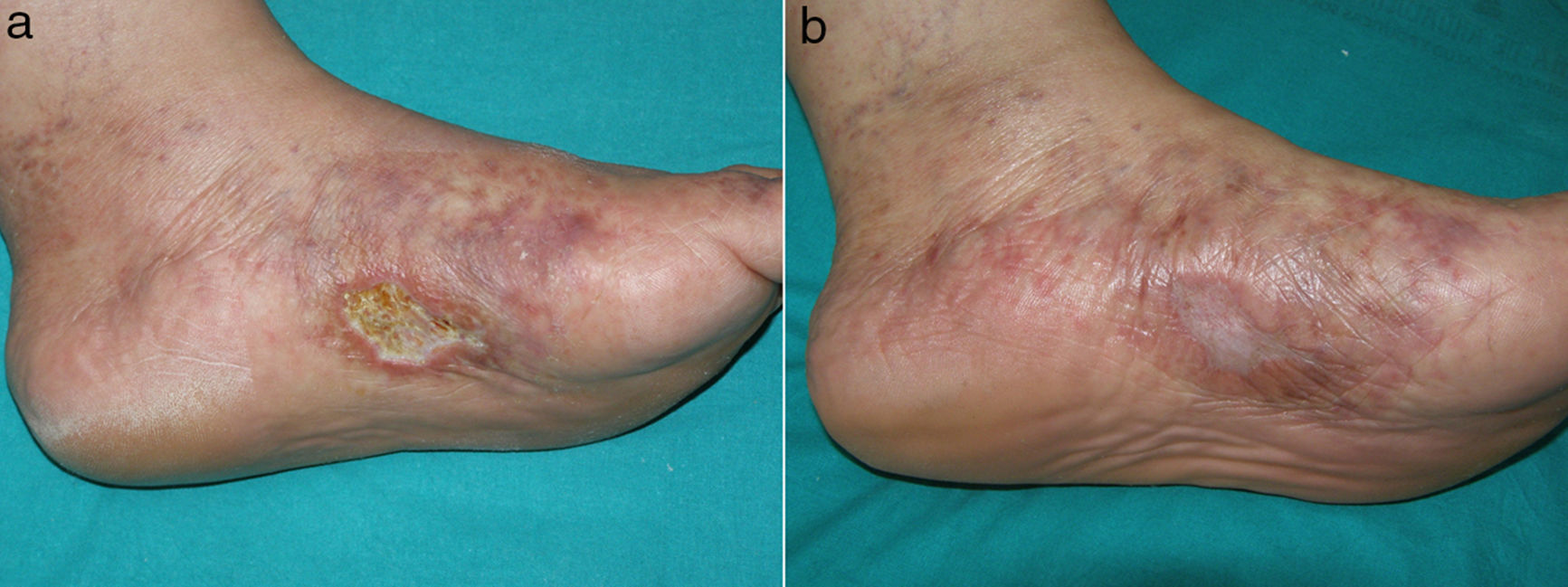
Case Description 1A 53-year-old woman with no relevant past history presented with multiple skin ulcers on her feet. The ulcers were painful and had been present for 2 years. Physical examination revealed an ulcer measuring approximately 3cm on the medial aspect of the left foot against a background of livedo racemosa and retiform purpura (Fig. 1A). The patient's medical history and exploratory tests ruled out hypercoagulability, systemic inflammatory disease, and infection. In the evaluation of peripheral arterial disease, no alterations were observed in the ankle-brachial index or in the Doppler ultrasound scan. Skin biopsy showed fibrin clots in the dermal vessels, extravasated red blood cells, hyalinization of the vessel walls, and neovascularization consistent with LV. Treatment was initiated with acetylsalicylic acid 300mg/d, intravenous alprostadil 60μg/d, and subcutaneous enoxaparin 1mg/kg/d. These treatments resulted in a mild reduction of pain and had almost no effect on ulcer healing. The patient was subsequently started on rivaroxaban 10mg/d, which resulted in full resolution of pain after a week and healing of the ulcer at 3 months (Fig. 1B). Twelve months after initiation of treatment with rivaroxaban, the patient was free of pain and ulcers, although there were no changes to the livedo racemosa.
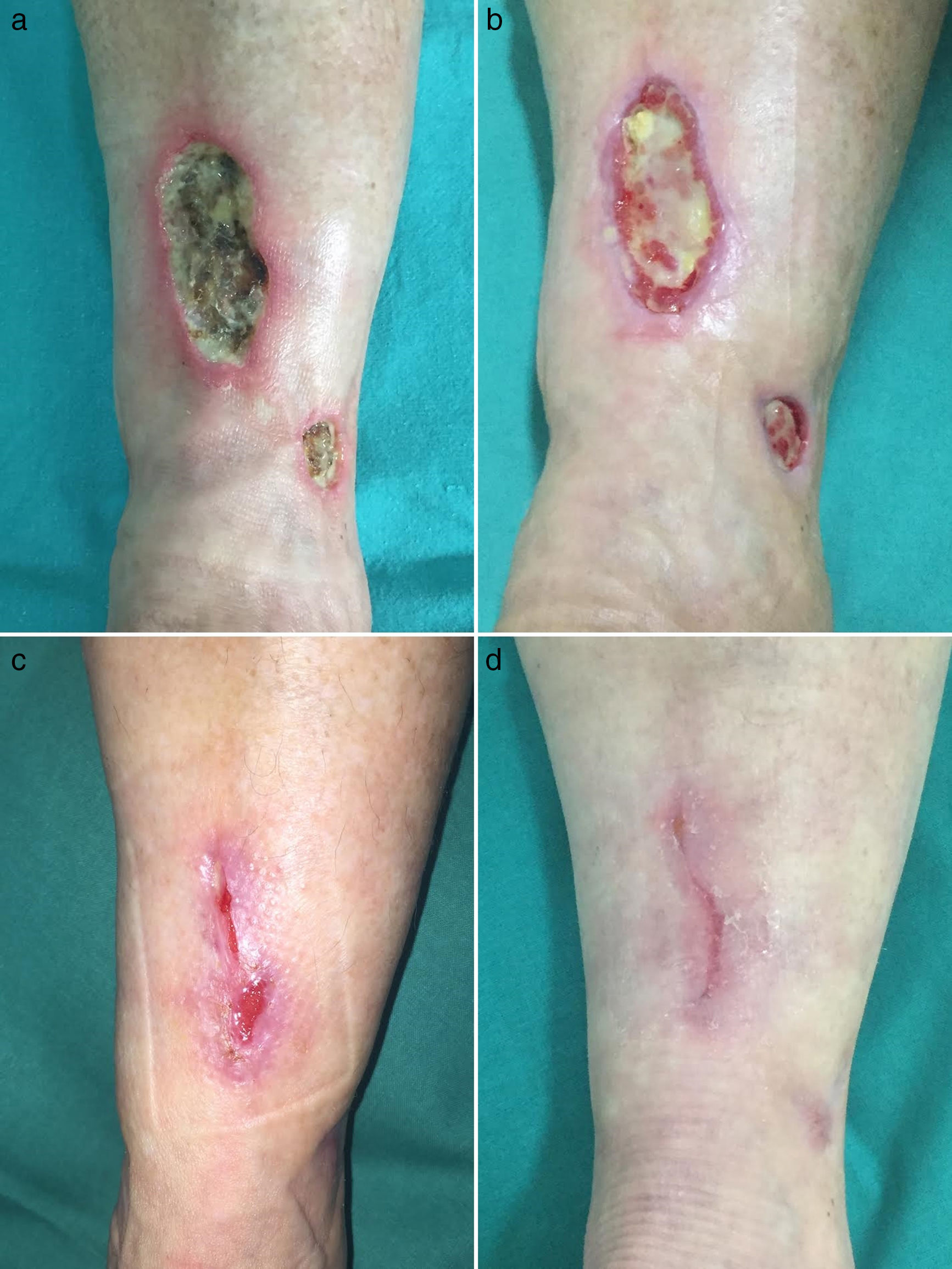
Case Description 2A 55-year-old woman with no past history of interest presented with multiple painful cutaneous ulcers of 12 years’ duration on the lower legs. Physical examination revealed multiple ulcers, some measuring up to 10cm, with a necrotic base and a livedo racemosa pattern extending up to the knees (Fig. 2A). Based on the patient's medical history and tests, a secondary cause was ruled out. Skin biopsy findings were consistent with LV. The lesions were refractory to treatment with oral prednisone, hydroxychloroquine, acetylsalicylic acid, and pentoxifylline. Treatment with rivaroxaban 10mg/d led to reversal of pain after 2 weeks and full resolution of ulcers by month 4 (Fig. 2B-D). After 9 months of treatment with rivaroxaban, the patient remained pain free and ulcer free. Similarly to the first case described, there were no changes to the livedo racemosa.
LV can occur as a primary idiopathic condition or secondary to hypercoagulability states, (e.g., presence of lupus anticoagulant, anticardiolipin, type I cryoglobulinemia, factor V Leiden mutation, protein C deficiency, hyperhomocysteinemia, and antithrombin III deficiency).1,2 It can also occur in association with systemic inflammatory diseases, such as systemic lupus erythematosus and rheumatoid arthritis.2,3 The hallmark clinical findings in LV are livedo racemosa, skin necrosis, and on occasions, noninflammatory vascular thrombosis.3 The characteristic scarring pattern left by ulcers in LV is known as atrophie blanche, which appears as a porcelain-white scar with red dots (prominent capillaries).1
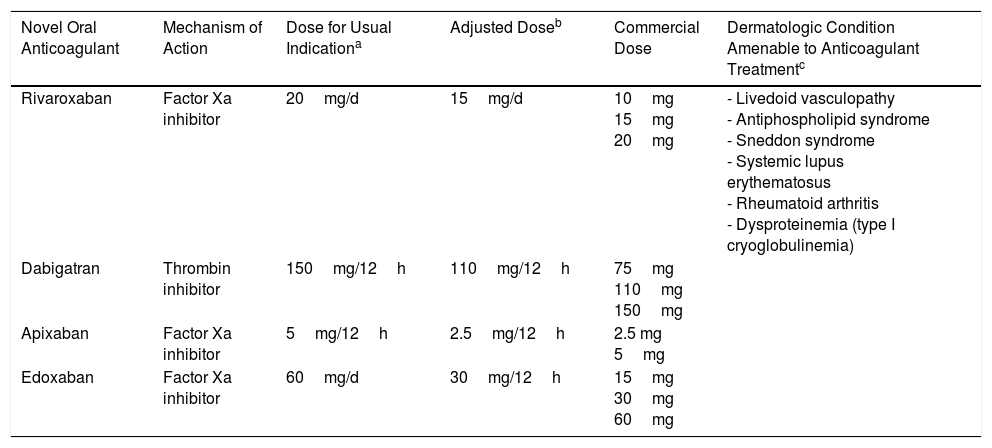
There is evidence of reduced fibrinolytic and increased thrombin activity in the vessel walls in LV.1 This thrombotic microvascular state is a histopathologic feature of LV. A perivascular lymphocytic infiltrate may also be observed, but it is considered to be a secondary finding and does not cause vasculitis.1,4 The most novel, and effective, treatments for LV are thus anticoagulants rather than immunomodulatory drugs. Table 1 provides a list of these anticoagulants together with a summary of their potential applications and doses.3,5 Thanks to these new anticoagulants, dermatologists are now better positioned to manage microcirculatory thrombotic disorders, essentially because they eliminate the need for hematologic control. Rivaroxaban is a novel factor X inhibitor that has proven effective in different clinical cases and a phase II multicenter clinical trial. The 10-mg dose has been found to achieve rapid relief of ischemic pain and complete remission of ulcers.6–8
Novel Oral Anticoagulants With Potential Therapeutic Applications in Dermatology.
| Novel Oral Anticoagulant | Mechanism of Action | Dose for Usual Indicationa | Adjusted Doseb | Commercial Dose | Dermatologic Condition Amenable to Anticoagulant Treatmentc |
|---|---|---|---|---|---|
| Rivaroxaban | Factor Xa inhibitor | 20mg/d | 15mg/d | 10mg 15mg 20mg | - Livedoid vasculopathy - Antiphospholipid syndrome - Sneddon syndrome - Systemic lupus erythematosus - Rheumatoid arthritis - Dysproteinemia (type I cryoglobulinemia) |
| Dabigatran | Thrombin inhibitor | 150mg/12h | 110mg/12h | 75mg 110mg 150mg | |
| Apixaban | Factor Xa inhibitor | 5mg/12h | 2.5mg/12h | 2.5 mg 5mg | |
| Edoxaban | Factor Xa inhibitor | 60mg/d | 30mg/12h | 15mg 30mg 60mg |
There have also been recent success stories with the use of dabigatran 220mg/d9 and apixaban 10mg/d in patients10 with LV refractory to vasodilators and/or antiplatelet agents. It should be noted that the doses used for LV tend to be lower than those established for the approved indications of these new anticoagulants. Formulations containing lower doses are also commercially available (Table 1).
In conclusion, we have described 2 new cases of cutaneous ulcers due to LV that did not respond to treatment with vasodilators or antiplatelet agents but that were successfully treated with rivaroxaban. This anticoagulant resulted in rapid pain resolution and complete and lasting resolution of ulcers. Dermatologists should be familiar with the existence and use of these novel oral anticoagulants in view of their potential applications in thrombotic disorders of cutaneous microcirculation.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank Professor José María Báez Perea from the University of Cadiz, also a pathologist at Hospital Universitario Puerta del Mar, for his expert contribution to the histopathologic study of the cases presented.
Please cite this article as: Jiménez-Gallo D, Villegas-Romero I, Rodríguez-Mateos ME, Linares-Barrios M. Vasculopatía livedoide tratada con rivaroxabán. Potenciales usos de los nuevos anticoagulantes orales para el dermatólogo. Actas Dermosifiliogr. 2018;109:278–281.