The reconstruction of surgical defects on the forehead and scalp is extremely challenging, especially when having to deal with large lesions. The windmill flap technique was first described by Russo et al. back in 2022,1 from a new experimental model that measures the tensions generated at each section of the flap.2 We hereby report a series of 4 patients in whom this brand-new reconstructive technique was used.
A total of 4 patients previously diagnosed with squamous cell carcinoma referred from 3 centers with Dermatology Surgery Units were selected. The lesions were excised through outpatient surgery, under local anesthesia and/or sedation. The surgical margin planning followed the recommendations made by the American Joint Committee on Cancer (AJCC) clinical practice guidelines.3 Finally, the reconstruction of the resulting defect was performed using the windmill flap technique.
Below, we describe the flap design and surgical technique used:
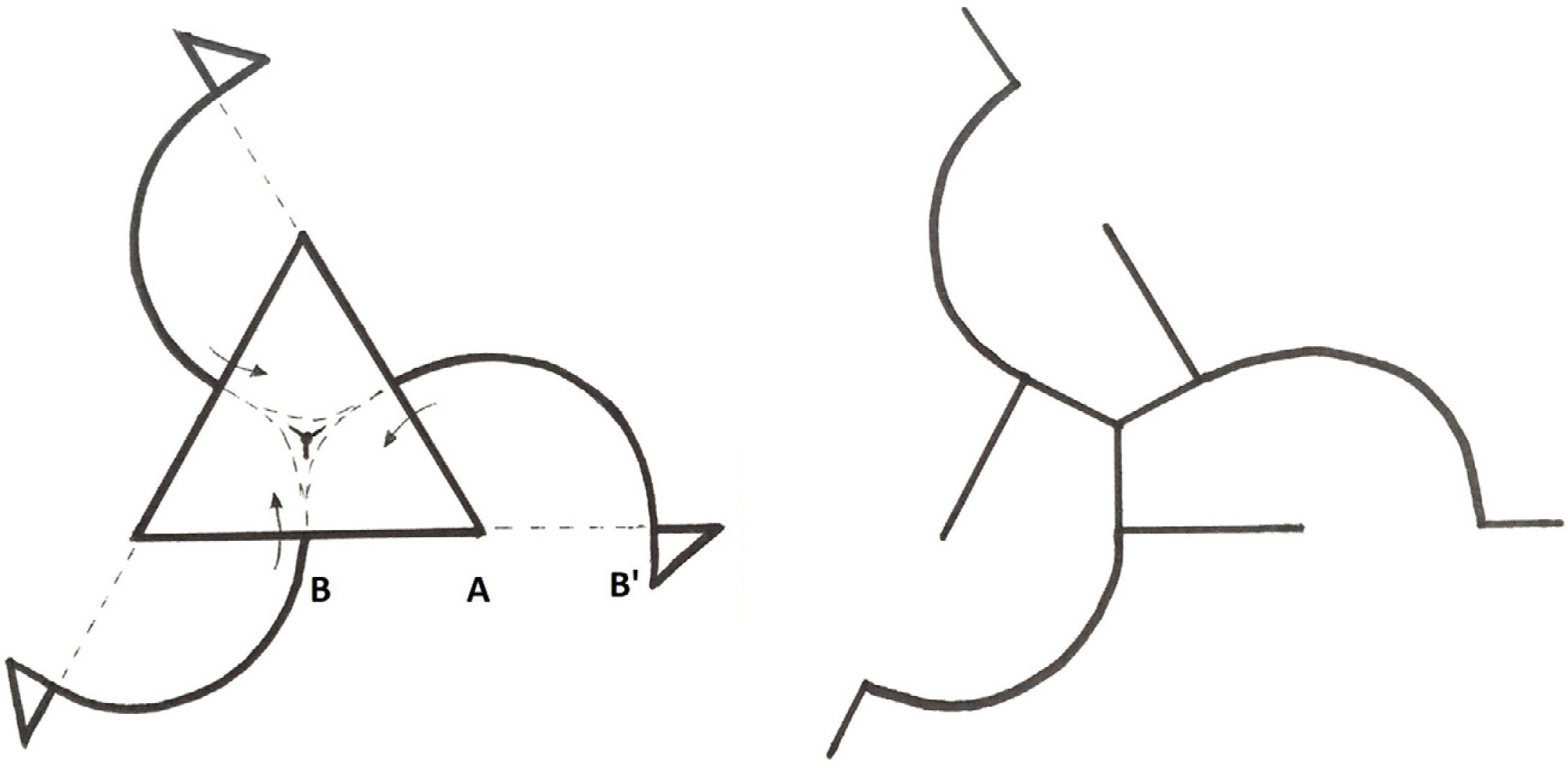
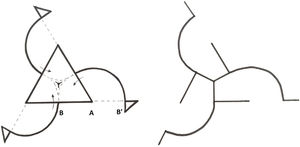
Flap design (Figure 1):
- 1.
We drew an equilateral triangle that should include the lesion and surgical margins, and labeled each of its vertices as A and the midpoint of its 3 corners as B. The distance between A and B should be projected from A to B.
- 2.
To design the 3 rotation lobes, we drew 2/6 of a circumference starting from B until it came across point B on the adjacent corner.
- 3.
Finally, we added a discharge triangle to each B point.
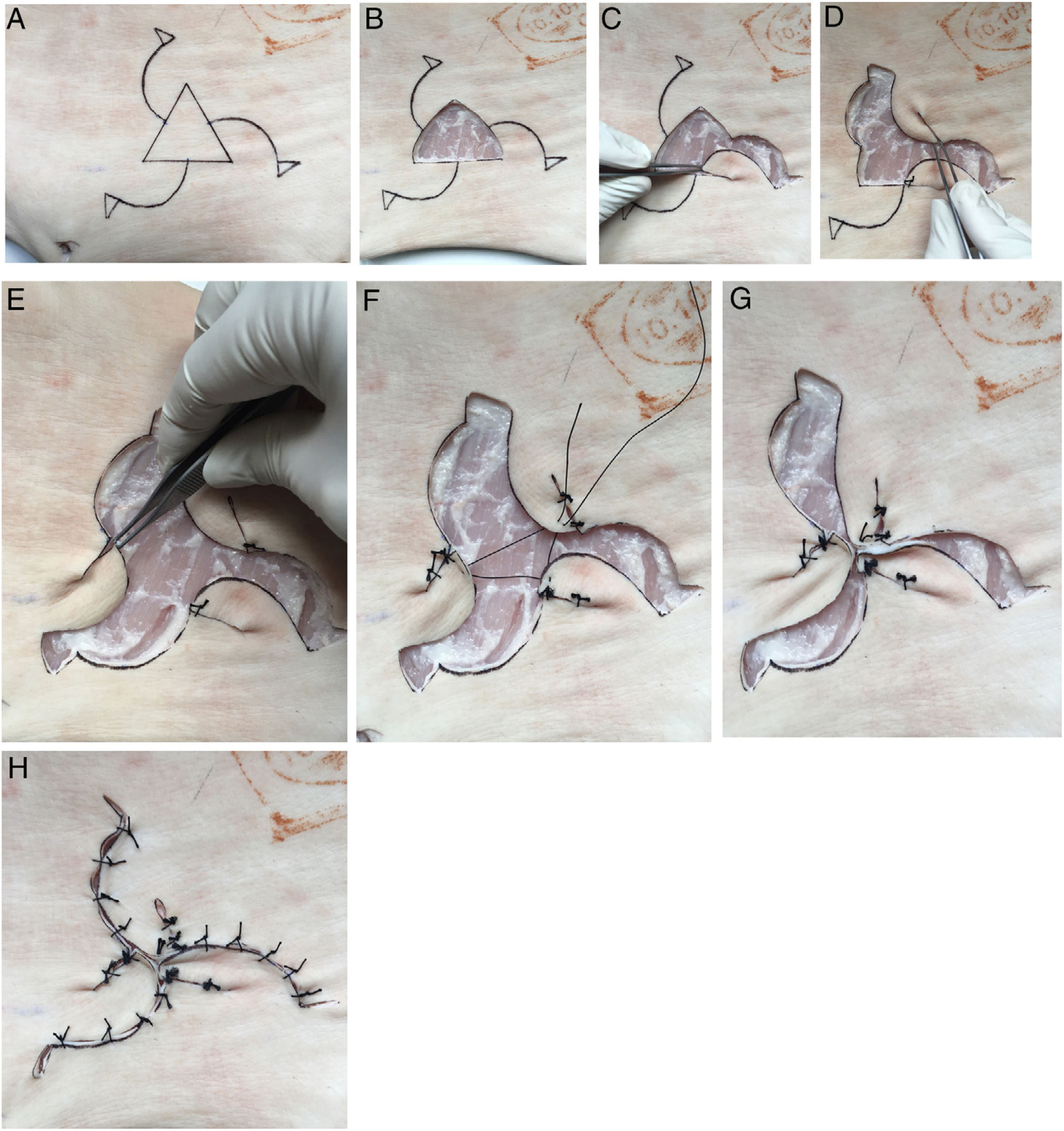
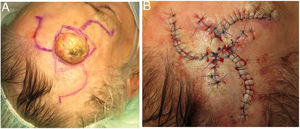
Surgical technique used (figure 2A-H):
- 1.
Once the flap was designed, our surgical technique started by removing the central equilateral triangle.
- 2.
Afterwards, we detached each of the lobes from the surgical bed and rotated them 60° in the same direction until they came into contact with the adjacent B point, thus creating a sinusoidal pattern made by 3 different waves.
- 3.
Finally, we connected the centers of the waves with a buried suture and moved on to suture their free edges creating a 3-helix windmill-like pattern.
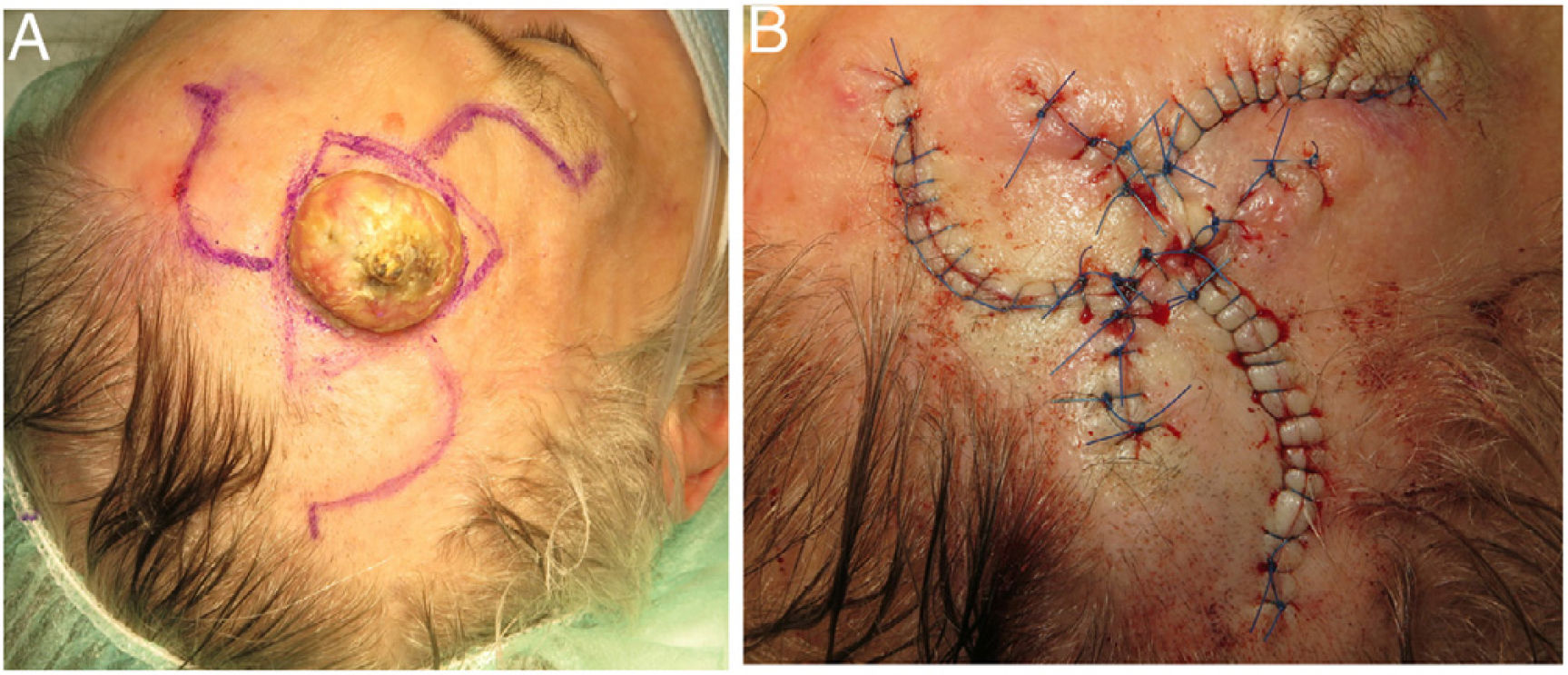
Overall, 3 men and 1 woman were included, with 2 lesions located on the forehead and 2 on the scalp (figure 3). The mean age at diagnosis was 82 years (range, 74-89). The mean tumor size was 2.7cm (range, 1.7cm to 4cm). There were no immediate or long-term complications resulting from the surgical technique used. The functional and aesthetic outcomes were considered satisfactory in all cases (Appendix B. See supplementary data).
Both the forehead and the scalp are sun-exposed areas prone to multiple skin tumors. In 2017, Russo et al.4 conducted a study that assessed the preferred reconstructive technique for different aesthetic medicine units through a survey submitted to a group of dermatologists. The techniques selected for the scalp, central forehead, and temple were the O to Z rotation flap, the bilateral advancement flap in a flag or H shape, and the rhomboid (Limberg) transposition flap, respectively. This study stresses the need for having multiple reconstructive options available for the same location, while considering each surgeon's skills, and adapting the reconstructive technique to the individual characteristics of each patient.
Biomechanical models have demonstrated that rotation flaps like the O to Z flap generate less tension than other advancement flaps like the A to T or flag flap, thus reducing the risk of ischemia and the possibility of necrosis.2 Although this flap was originally designed to repair triangular surgical defects, it has proven useful to treat circular defects inscribed within a triangle.1
Longer surgical times and more scars are among the main limitations of this kind of flap, although this did not result in more surgical complications.
In our series, we selected elderly patients with large lesions located in convex anatomical regions such as the forehead and the scalp. Still, the windmill flap technique can probably be used to reconstruct other defects in various locations.
In conclusion, we propose the windmill flap as a new and useful technique to reconstruct large defects in high-tension areas such as the forehead and scalp, with favorable functional and aesthetic outcomes.
Conflicts of interestNone declared.