Scientific medical literature, sometimes, describes seborrheic keratosis (SK) as a seborrheic wart due to its clinical similarity to warts. However, microscopic examination is a significant tool to distinguish between these 2 entities.
There are several morphological types of SK recognized in the literature, being the acanthotic and reticulated types the most common of all. In addition to these, we would like to highlight a pattern we frequently encounter in our routine dermatopathology practice that, still, has not been described in the classic texts on SK: the coexistence within the same lesion of overlapping features of SK and a common wart. We have coined the term “seborrhuca” to describe this pattern.
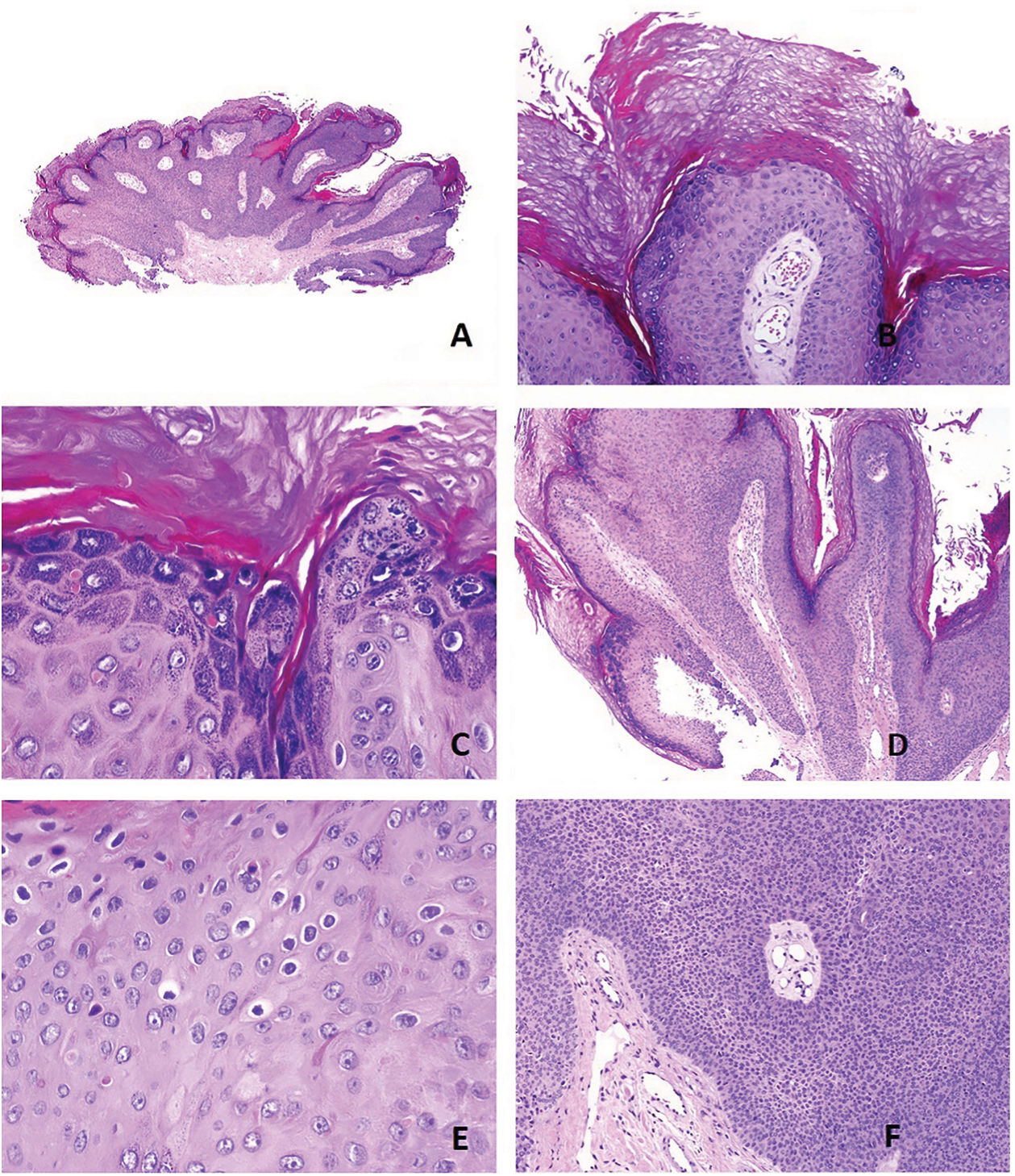
Seborrhucas exhibit characteristics of common warts: a papillomatous silhouette (fig. 1A), hyperkeratosis, columns of parakeratosis at the tips of the papillae (fig. 1B) with agranulosis underneath the parakeratotic column and a prominent granular layer in some other regions (fig. 1C). In the papillary dermis of the papillae, tortuous and often dilated capillaries become evident (fig. 1D). Focal koilocytic changes can sometimes be seen (fig. 1E). Many different characteristics of SK overlapping these wart-typical features are, also, evident. Excessive growth of monomorphic round cells, for example, is prominent (fig. 1F). Additionally, corneal pseudocysts or infundibular tunnels can sometimes be an accompanying feature, as well as the typical whorls of SK (fig. 2B).
Histopathological features observed in seborrhuca: A) papillomatous silhouette (H&E x20). B) parakeratotic columns at the tips of the papillae with agranulosis (H&E x100). C) thick keratohyalin granules (H&E x200). D) tortuous capillary vessels in the papillae (H&E x100). E) koilocytes (H&E x400). F) overgrowth of monomorphic basaloid cells (H&E x100).
Whether this type of SK is related to human papillomavirus (HPV) infection is still a matter of discussion. Studies on HPV associated with SK have included all types of SK without morphological selection of the seborrhuca type. Therefore, most of the cases included probably fall into the category of acanthotic SK. For example, Lee et al. studied a total of 40 non-genital SKs by polymerase chain reaction (PCR) and found no HPV of the types tested.1 However, their figure 1A—selected by them as representative of their series—clearly shows an acanthotic type of SK.1
Conversely, other studies have managed to find HPV in SK: HPV-like particles in ultrastructural studies of non-genital SK;2 HPV DNA detected in 20% of non-genital SKs by in situ hybridization;3 and 15% up to 30% of SK cases positive for HPV on the PCR.4
In the cases found in the genital area, the association with HPV infection seems even stronger, with the virus demonstrated in up to 72% of genital cases by PCR or immunohistochemistry4 to the point that some authors claim that genital SKs containing HPV are actually condylomas acuminata.1,5
In this regard, Zhu et al. presented a very interesting study of DNA amplification by PCR in lesions they called “benign verrucous acanthomas,” describing them with characteristic features of common warts but lacking koilocytes in the granular layer.6 They could not find any HPV DNA sequences in amplified samples of these benign verrucous acanthomas6 but found HPV in verrucous lesions with koilocytes. Consequently, they considered koilocytes as the critical histopathological sign distinguishing common warts from benign verrucous acanthoma.6 Admitting this, however, would grant koilocytes a specificity and sensitivity as high as HPV-PCR, which contrasts with what has been described in the scientific medical literature on this regard. For example, in a very comprehensive study on histopathological features and HPV types, Jablonska et al. confirmed the presence of koilocytes only in warts induced by certain viral types (such as HPV-4 or HPV-10) but not in others.7 As we know, HPV-4 and HPV-10 are related to flat warts, while common warts are usually caused by HPV-28 and condylomas by HPV-6 and HPV-119 (types 6 and 11 can also be found in common warts in adults9). Other HPV types sometimes found in common warts are HPV-16, 42, 43, or 44.9
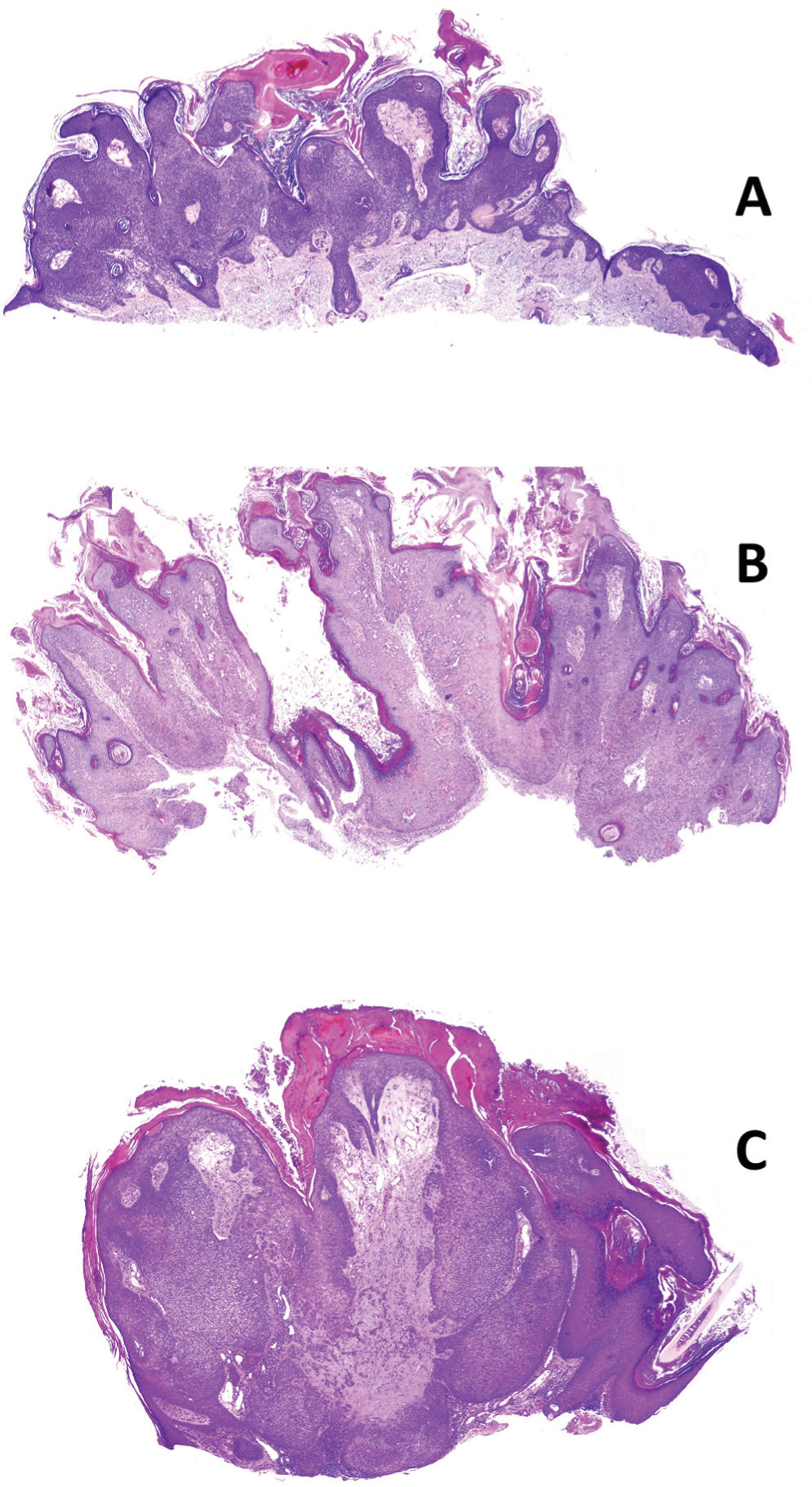
Figure 2 shows additional examples of seborrhucas at low magnification. But how significant is seborrhuca then? Is it a viral verrucous change (related to HPV) overlapping a SK, that is, a common wart-like SK? Or is it a seborrheic change occurring in a common wart, that is, a common wart-like SK? Or is it the collision of a SK and a common wart? Or is it merely a morphological change mimicking a wart but without the HPV infection? We’d rather stick to option #1 for 3 reasons: in the first place, common wart changes sometimes collide with SK areas (fig. 3A); also, when HPV is studied in collision cases, it is only seen in verrucous—not in SK—regions.10
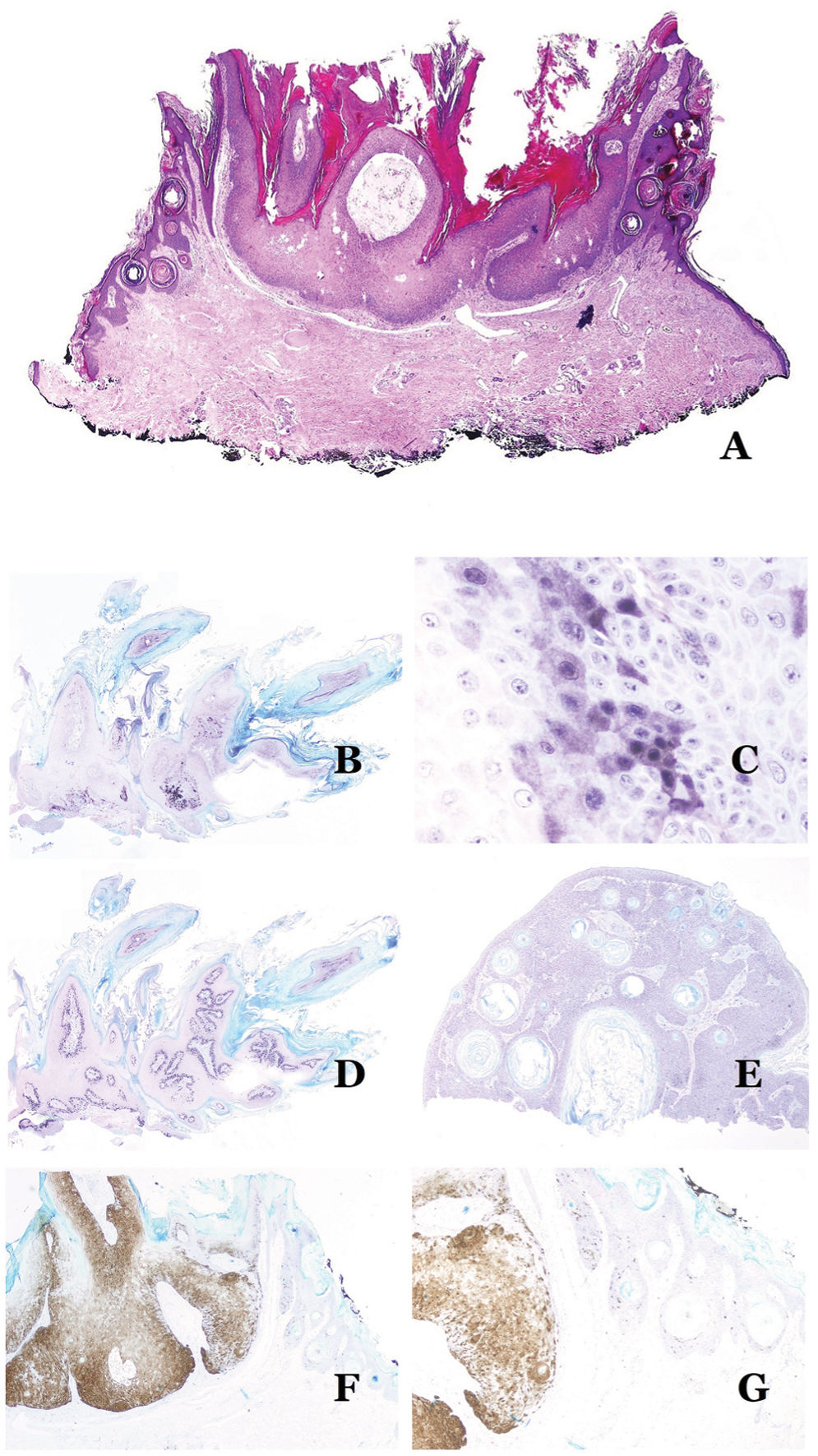
A) Changes of common wart in collision with peripheral areas of SK (H&E x20). B, C, and D) Typical features of seborrhuca in the immunohistochemical study. Seborrhuca shows patches of positive staining with p16 (B: p16, x20). The patches consist of more than 10 cells positive for p16, with both cytoplasmic and nuclear staining (C: p16, x400). Ki-67 shows positivity in the basal layer of the lesion only (D: Ki67, x20). In contrast, SK is p16 negative (E: p16, x20). When collision lesions between wart and SK are seen, the wart areas are p16-positive while the SK ones are p16-negative (F: p16, x20; G: p16 x40).
Therefore, we conducted several immunohistochemical studies with Ki67 and p16 in seborrhuca cases, and results are similar to those seen in a viral warts, i.e., patchy groups of more than 10 cells positive for p16 (fig. 3B and C), with a high proliferation index in the basal layers of the lesion (fig. 3D). This contrasts with what has been reported in SK cases (negative for p16) (fig. 3E). Furthermore, these findings contrast with what has been confirmed through evidence in obvious collision cases between common warts and seborrheic keratosis, in which only the common wart areas test positive for p16, while the seborrheic keratosis test negative for p16 (fig. 3F and G). All these findings support the idea that seborrhuca is a lesion with morphological characteristics of seborrheic keratosis that has sustained an HPV infection, eventually leading to the acquisition of additional wart-like features.
The term seborrhuca is intended for cases in which histopathological features overlap so much that a simple diagnosis of wart or SK would be arbitrary. It is not intended to replace either of those diagnoses when the morphological features are clear enough to the point of being able to achieve a specific diagnosis of one of these entities.