This article in the series “Safety in Dermatologic Procedures” deals with the accidental laceration of major blood vessels and nerve structures during surgery. We first look at the anatomic location and course of the blood vessels and nerve structures that are most at risk of injury and then describe the possible outcomes in each case. We finally offer some recommendations on how to avoid damage to structures in danger zones and how to repair them if they are accidentally compromised.
En el presente artículo de la serie «Seguridad en procedimientos dermatológicos» se aborda la sección quirúrgica accidental de grandes vasos sanguíneos y estructuras nerviosas. Se aborda, en primer lugar, la localización anatómica y recorrido de las distintas estructuras vasculares y nerviosas de más riesgo. A continuación, se explican las consecuencias de dicha lesión. Por último, se emiten algunas recomendaciones para evitar el daño accidental de las estructuras en dichas áreas de riesgo y se plantean algunas maniobras terapéuticas de reparación ante un eventual daño.
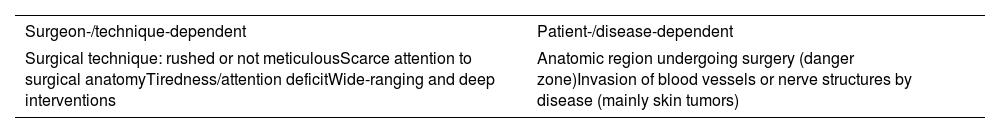
Knowledge of the location and course of blood vessels and nerve structures is the single most important anatomic factor for the dermatologic surgeon.1 Therefore, we highlight anatomic danger zones with emphasis on the face and neck, where both nerves and vessels come into close contact with superficial tissue, leaving them susceptible to damage. Motor nerve damage can cause functional or cosmetic deformities, permanent involuntary contractions, and muscle shortening. In addition, damage to sensory nerves can lead to definitive loss of sensitivity, dysesthesia, and untreatable pain. The various risk factors for damage to blood vessels and nerve structures during surgery depend on the surgeon and the technique applied, as well as on the patient and the disease (Table 1).
Risk Factors for Damage to Nerve Structures and Blood Vessels.
| Surgeon-/technique-dependent | Patient-/disease-dependent |
|---|---|
| Surgical technique: rushed or not meticulousScarce attention to surgical anatomyTiredness/attention deficitWide-ranging and deep interventions | Anatomic region undergoing surgery (danger zone)Invasion of blood vessels or nerve structures by disease (mainly skin tumors) |
The serious consequences resulting from injury to nerves and blood vessels mean that a precise knowledge of the anatomic risk areas is essential before undertaking any surgical procedure in the area affected.
Below, we address 5 danger zones on the face and neck based on those described by Seckel2 (see Table 2 for summary).
Description of the 5 Cervicofacial Zones at Risk Owing to the Presence of Major Blood Vessels and Nerve Structures.
| Location | Structure | Location with respect to SMAS | Disease | |
|---|---|---|---|---|
| Zone 1 | Triangle formed by the tragus, zygoma, and a point 2cm above the lateral eyebrow | Temporal branch of the facial nerve | Below | Paralysis of the frontalis muscle |
| Zone 2 | Mandible, 2cm posterior to the oral commissure | Marginal branch of the facial nerveFacial artery | Below | Paralysis of the lower lipNot significant |
| Zone 3 | Triangle located between the malar eminence, mandibular angle, and oral commissureCheek, middle third of the line joining the tragus and the philtrum | Buccal and zygomatic branches of the facial nerveParotid duct | Below | Paralysis of the upper lip and cheekSalivary pseudocysts (sialocele), fistulas, and/or abscesses |
| Zone 4 | Cervical, Erb point.6.5cm below the external auditory canal | Great auricular nerveAccessory nerve | Posterior | Anesthesia of lower two-thirds of the pinna and region adjacent to the cheek and neckDropped shoulder and chronic shoulder pain, difficulty with abduction of the arm, and atrophy of the deltoid and sternocleidomastoid muscles |
| Zone 5 | Preauricular, at the level of the zygomatic arch | Auriculotemporal nerveSuperficial temporal vessels | Posterior | Frey syndrome: gustatory hyperhidrosis and vasodilationNot significant |
Abbreviation: SMAS, superficial musculoaponeurotic system.
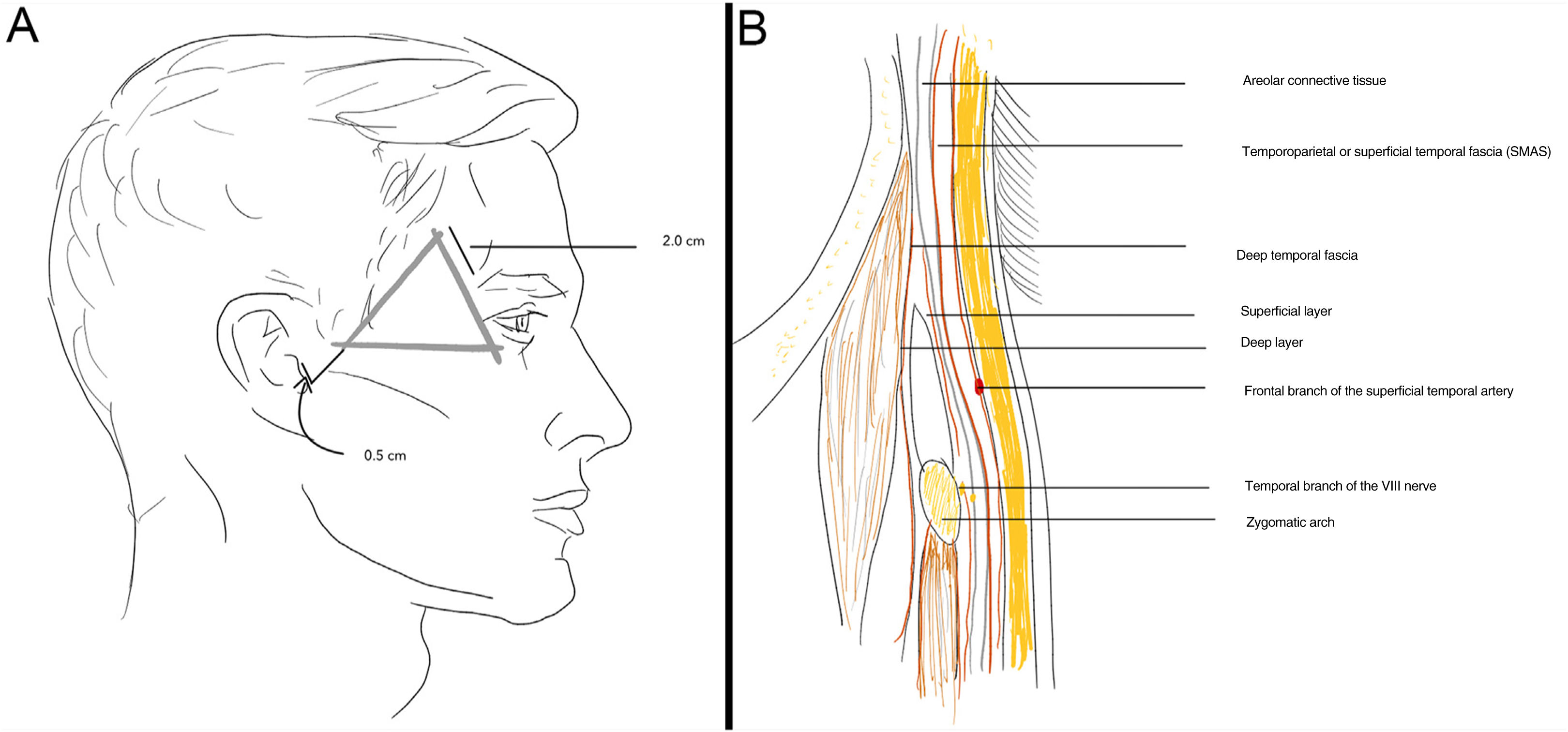
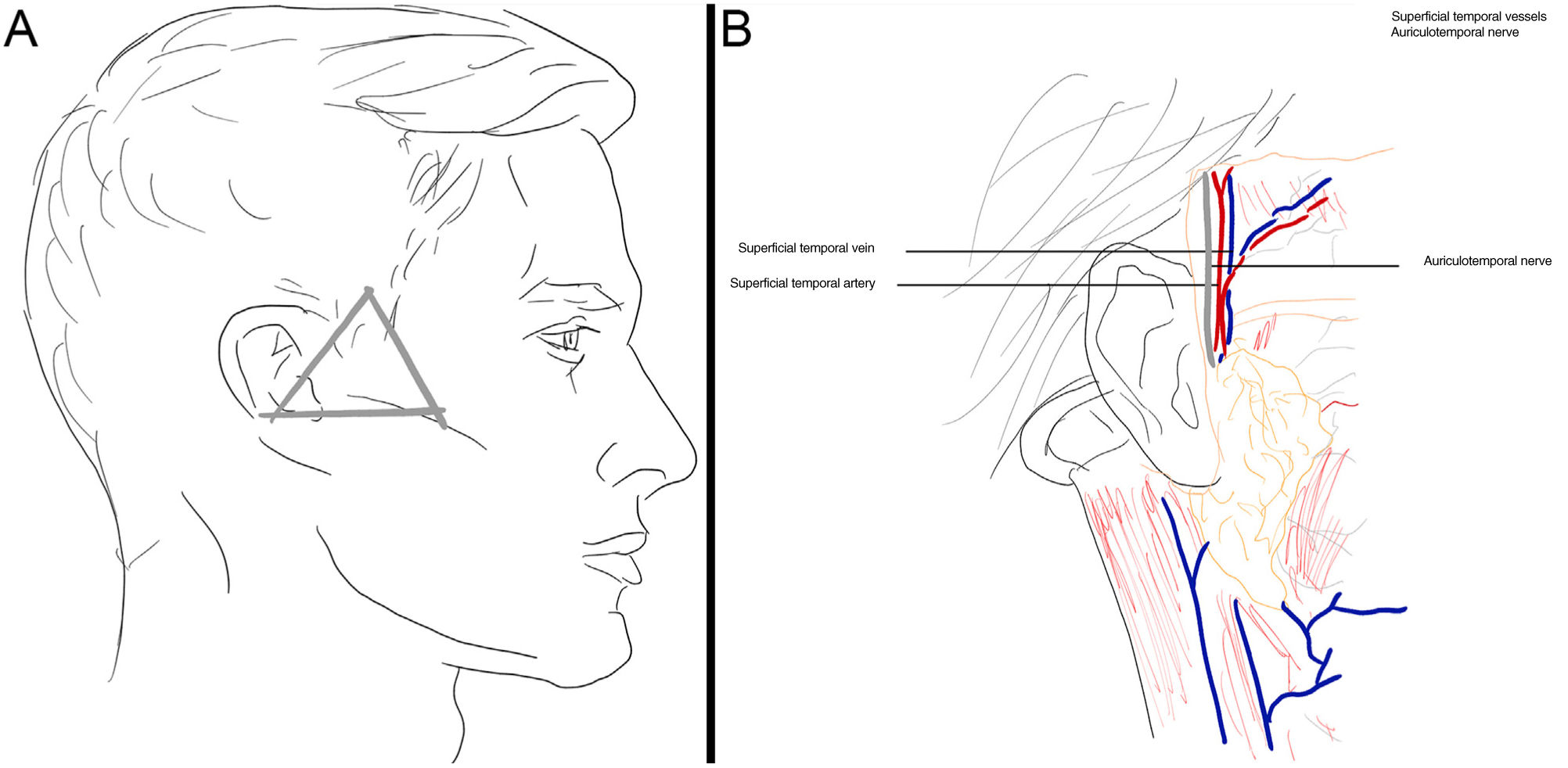
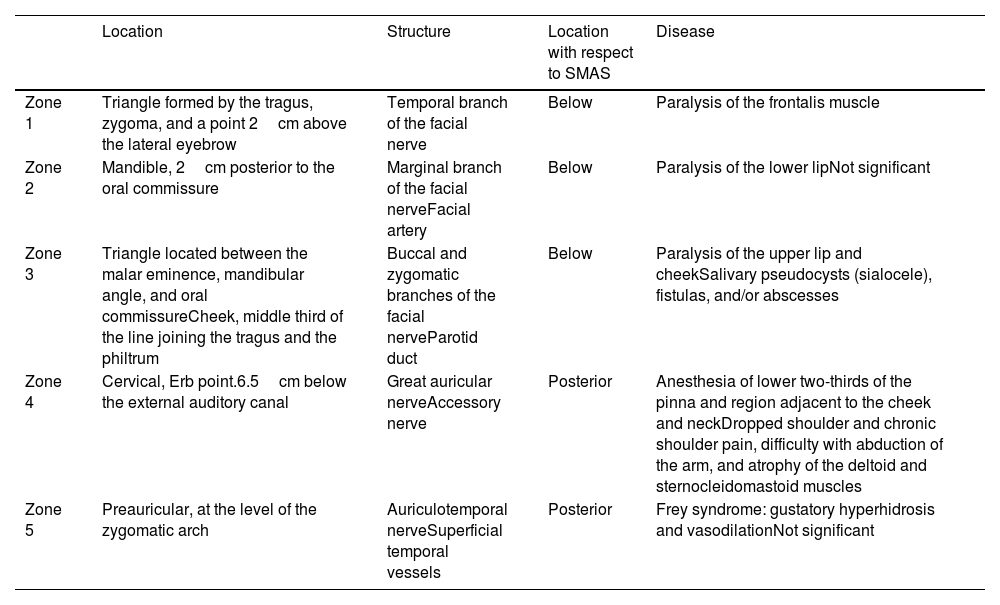
Zone 1 is where the temporal branch of the facial nerve (VII) emerges from the parotid gland. The danger zone is located in the temporal area above the zygomatic arch by drawing a line from a point 0.5cm below the tragus to a point 2cm above the lateral eyebrow. A second line follows the zygoma to the lateral orbital rim. The triangle is closed by a line running from the point 2cm above the lateral eyebrow to the outer orbital rim (Fig. 1A). In this zone, the temporal branch of the facial nerve is below the temporoparietal fascia and anterior to the deep temporal fascia, thus leaving it open to injury (Fig. 1B).
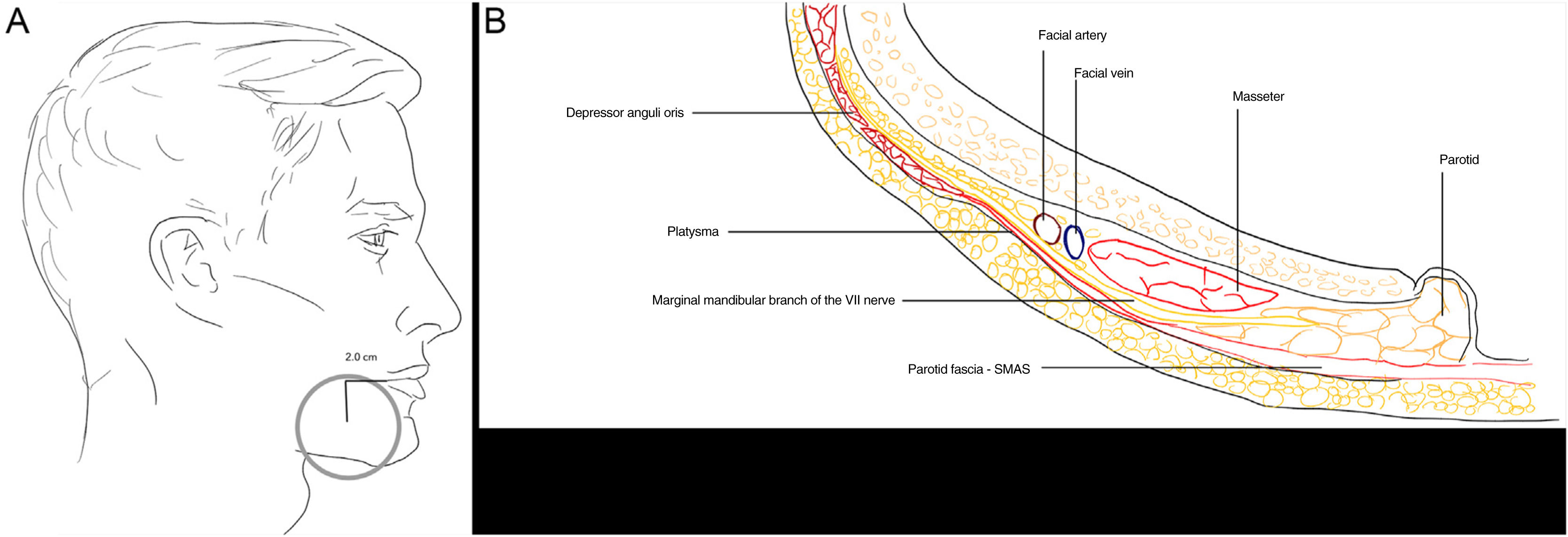
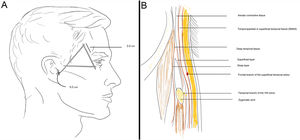
Zone 2Zone 2 is where the marginal branch of facial nerve is most vulnerable, since the platysma–superficial musculoaponeurotic system (SMAS) is thinner. The presence of the facial artery at this location acts as a reference point for locating the marginal branch of the facial nerve, which courses posterior to the artery after crossing it.
The danger zone is described by drawing a point 2cm posterior to the oral commissure and centered on the mandibular body. At this point, a circle with a radius of 2cm is drawn (Fig. 2). This circle defines the area of greatest risk, which also includes the facial vein and artery (Fig. 2B).
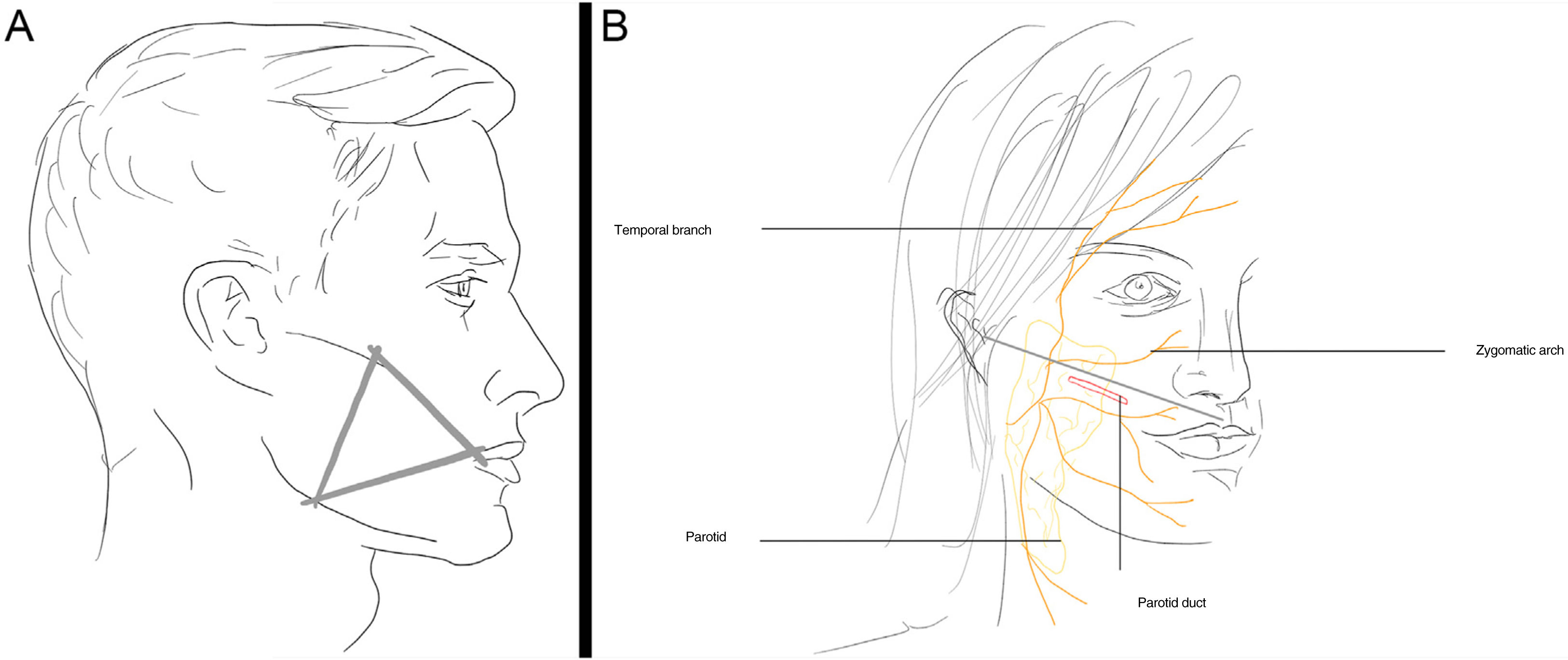
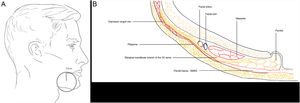
Zone 3Zone 3 contains the parotid (Stensen) duct and the zygomatic and buccal branches of the facial nerve, which lie superficial to and rest on the Bichat fat pad. These branches supply the major and minor zygomatic muscles, the levator labii superioris, and the nasal alar elevator. The parotid duct drains the content of the parotid gland to the interior of the mouth in the buccal mucosa.
The danger zone lies in the deep part of the SMAS and the parotid fascia and is well protected. The most vulnerable area comprises the triangle formed by the malar eminence, the posterior border of the angle of the mandible, and the oral commissure (Fig. 3A). The parotid duct is located more superficially in the middle third of the line joining the tragus and the philtrum (Fig. 3B).
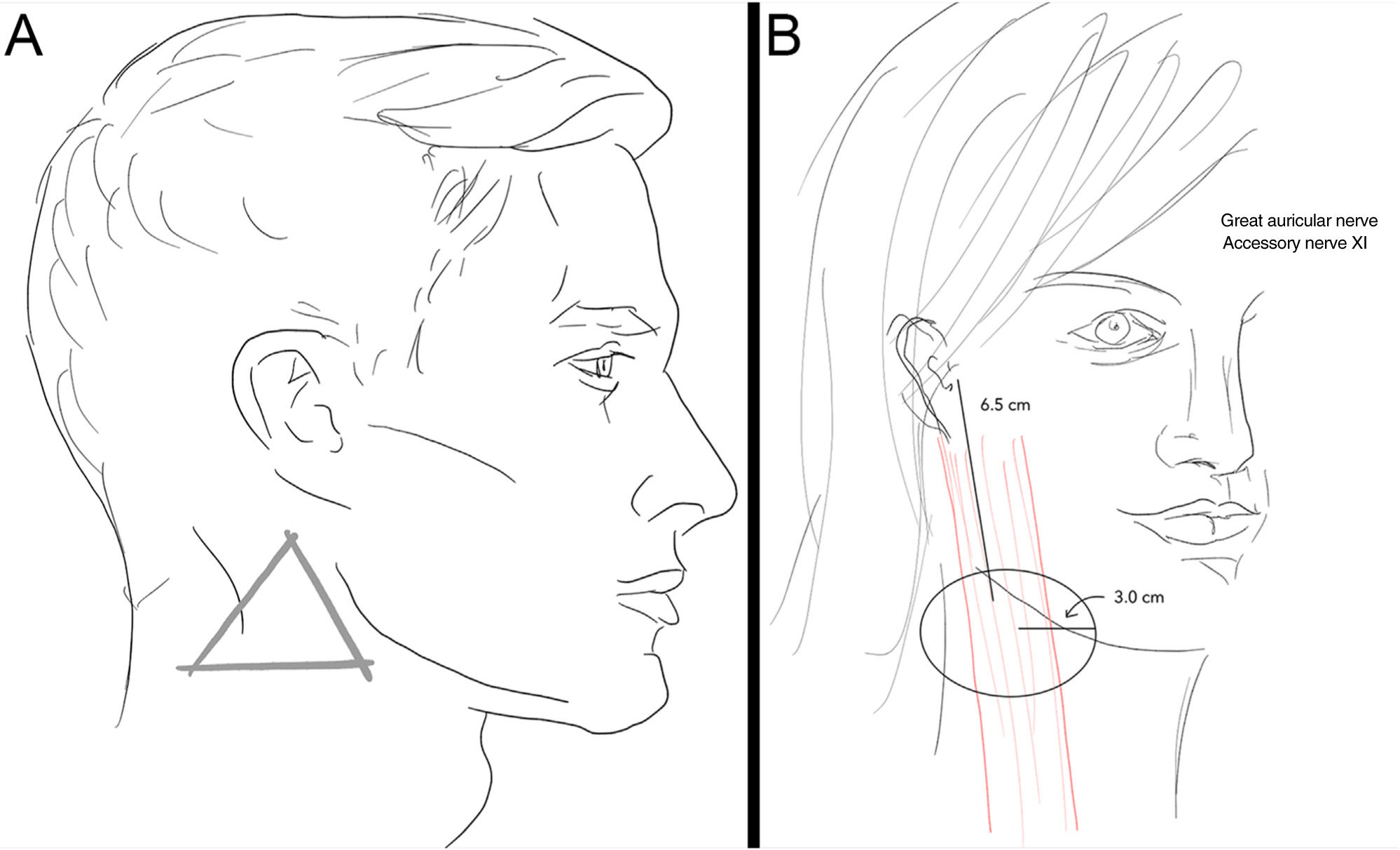
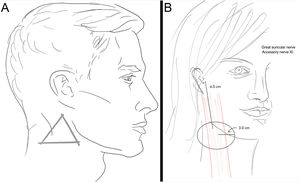
Zone 4Zone 4 includes the great auricular nerve and the accessory nerve (XI). The lateral part of the neck can be seen as a trapezoid, which is divided by the sternocleidomastoid muscle into 2 triangles (anterior and posterior). The posterior triangle contains both nerves. The danger zone is the Erb point, which is the area from which the great auricular nerve and accessory nerve emerge from behind the sternocleidomastoid muscle without the protection of the platysma-SMAS3,4 (Fig. 4A).
To determine the anatomic location of the danger zone, the sternocleidomastoid muscle is palpated with the patient's head turned to the opposite side, and a 6.5-cm line is dropped from the external auditory canal downward over the sternocleidomastoid to the midpoint of the muscle belly, approximately, until it reaches the laryngeal cartilage. At this point, we draw a circle with a radius of 3cm (Fig. 4B).
Zone 5Zone 5 includes superficial temporal vessels and the auriculotemporal nerve, which contains sympathetic fibers innervating the sweat glands of the scalp and parasympathetic fibers supplying the parotid.
The anatomic location of the danger zone includes the preauricular region at the level of the zygomatic arch, where the auriculotemporal nerve and the superficial temporal artery and vein course more superficially below the temporoparietal fascia-SMAS, once they have exited the parotid gland (Fig. 5).
Lastly, it is worth mentioning larger-caliber structures such as the external jugular vein in the cervical region, the long thoracic nerve, the thoracodorsal nerve, the axillary vein in the axilla, the femoral artery and vein in the groin, the sciatic nerve, the popliteal vessels in the popliteal fossa, and the posterior tibial vessels. Damage to these structures is infrequent in dermatologic surgery. When it does occur, it generally involves small lacerations during lymphadenectomy and broad and deep excisions/reconstructions in the areas of the head, neck, and limbs.
Consequences and Treatment of Damage to Nerve Structures and Blood VesselsBelow, we detail the consequences of damage to nerve structures and blood vessels and its repair according to the danger zones set out above.
Zone 1Damage to the temporal branch of the facial nerve can cause paralysis of the frontalis muscle, with sparing of the function of the orbicularis oculi owing to dual innervation from the zygomatic branches. Clinically, we observe ptosis of the brow, eyelid asymmetry, and forehead asymmetry during facial movements. Repair is by supraciliary half-moon incision on the affected side and fixing the eyebrow to the periosteum of the frontal bone. However, the voluntary mobility that enables the eyebrow to be raised is lost.
Zone 2Damage to the marginal branch of the facial nerve paralyzes the depressor anguli oris muscle, causing noticeable deformity, especially when the patient smiles, since it is not possible to show the teeth below the affected side. Repair is difficult and is carried out using microsurgery. Damage to the facial artery has no relevant consequences, although the artery must be ligated.
Zone 3Damage to the buccal and zygomatic branches of the facial nerve can result in facial asymmetry in the case of complete lesion owing to drooping of the oral commissure, especially when smiling. Fortunately, the presence of numerous connections between the buccal and zygomatic branches means that paresis is generally transient and resolves after a few months.
Laceration of the parotid duct leads to salivary pseudocysts (sialocele), fistulas, and/or abscesses. Repair involves surgery, in which the ends are sutured using microsurgery, with the possibility of using a double J stent urethral catheter as a guide.5
Zone 4Damage to the great auricular nerve can cause anesthesia or dysesthesia and pain in the case of neuroma affecting the inferior two-thirds of the pinna and the skin adjacent to the cheek and neck. Damage to the accessory nerve, on the other hand, can lead to dropped shoulder and chronic shoulder pain, difficulty in abduction of the arm, and atrophy of the deltoid and sternocleidomastoid muscles. In order to avoid damaging these nerves, the appropriate plane of dissection should lie superficial to the platysma in the upper part of the neck and in the subcutaneous fat in the posterior part.
Zone 5Laceration of superficial temporal vessels is not significant, requiring only ligation. In contrast, damage to the auriculotemporal nerve is associated with Frey syndrome, which is characterized by vasodilation and gustatory hyperhidrosis on the cheek. The damage can be repaired using botulinum toxin injection.
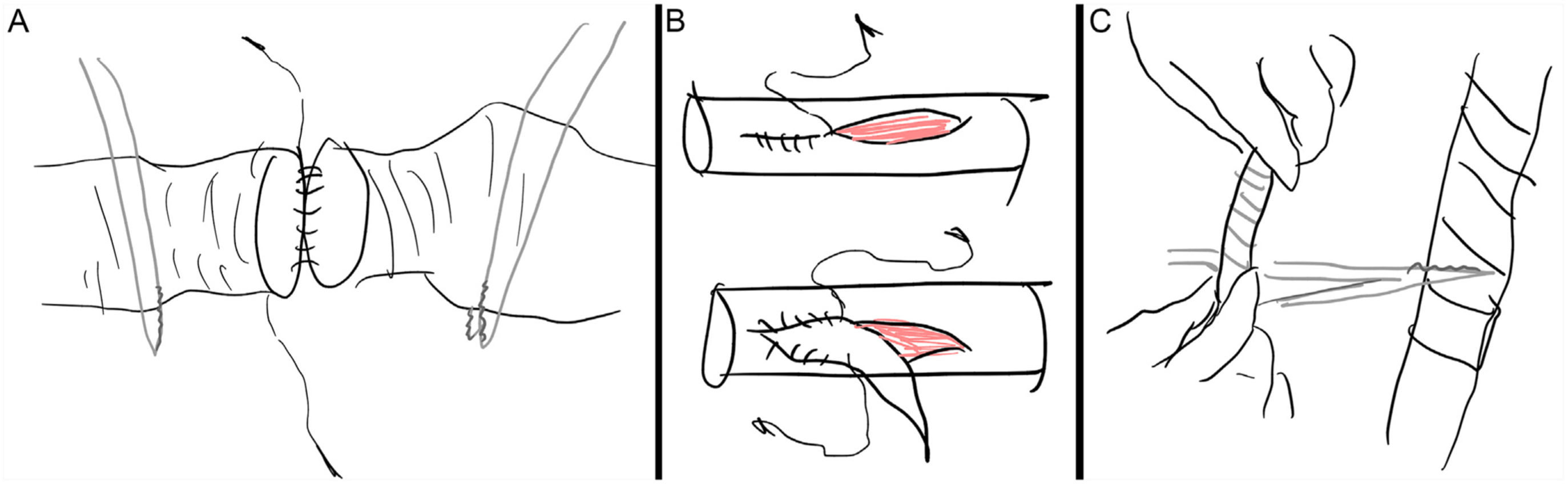
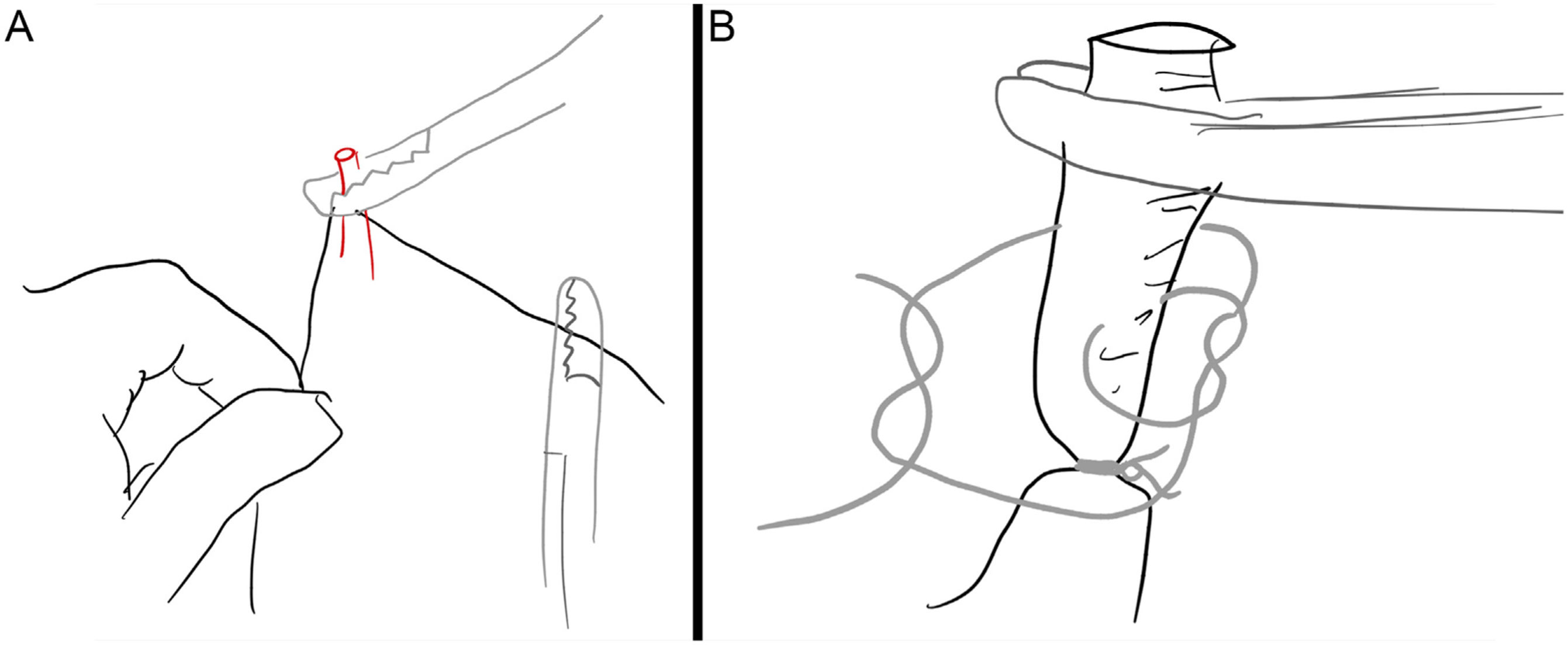
Damage to the large vessels can lead to major bleeding (which may require blood transfusion), thrombosis, arteriovenous fistula, pseudoaneurysm, loss of function, and limb ischemia. When a vessel has been completely lacerated, it is necessary to perform anastomosis or, if this is not possible, placement of a venous graft or a synthetic prosthesis (Fig. 6A). Lacerations of the arteries can be sutured, although if signs of tension are observed, arterioplasty with a venous or synthetic patch is preferred (Fig. 6B). In the case of lacerations of veins, the indication for repair or ligation is controversial. The options include suture, anastomosis, spiral vein graft using the saphenous vein or cephalic vein (Fig. 6C), or ligation combined with elevation of the limb and compression. Suture of large vessels may be continuous and bidirectional with a circular needle using monofilament 5/0 and 6/0 (e.g., with polypropylene). The procedure should be performed using atraumatic devices such as DeBakey forceps and clamps, always remembering to flush the vessel before complete closure in order to avoid thrombosis. Ligation should be performed 5mm from the laceration. In large vessels, a transfixion suture crossing the vascular lumen is recommended (Fig. 7).
The authors declare that they have no conflicts of interest.
We are grateful to Blanca Idoate Iglesias, a student of the Escuela Técnica Superior de Arquitectura of the Universidad Politécnica de Valencia, for her help and infinite patience with the design of the figures that illustrate the present work.