Numerous diets for losing weight, building strength, and managing a range of cardiovascular, neurologic, and skin diseases have become popular in recent years. The ketogenic diet and intermittent fasting in particular have shown promising results in clinical and sports medicine. The Mediterranean diet, in turn, is widely recognized for its numerous health benefits. Also popular are the paleo diet and vegan and gluten-free diets. Positive effects on inflammatory conditions, such as psoriasis, atopic dermatitis, hidradenitis suppurativa, and acne, have been observed in patients who practice intermittent fasting or follow ketogenic or Mediterranean diets. This last choice may also protect against certain skin cancers. We review the role of several popular diets in the management of skin disorders.
Se han popularizado diversas dietas para perder peso, incrementar la capacidad física y para el manejo de múltiples enfermedades crónicas: cardiovasculares, neurológicas o cutáneas. Destacan la dieta cetogénica y el ayuno intermitente, con resultados prometedores en la medicina tradicional y deportiva. Además, la dieta mediterránea se ha consolidado como una forma de alimentación de impacto positivo muy significativo en la salud. Otras dietas populares son la dieta «paleo», la dieta vegana y la libre de gluten. La dieta cetogénica, el ayuno intermitente y la dieta mediterránea aportan resultados favorables en dermatosis inflamatorias como la psoriasis, dermatitis atópica, hidradenitis supurativa o acné. La dieta mediterránea podría actuar también como factor protector para el desarrollo de algunas neoplasias cutáneas. En este artículo presentamos una revisión del papel de diversas dietas populares en el manejo de dermatosis.
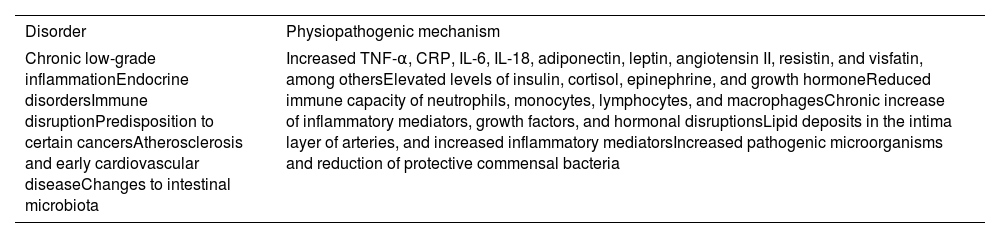
Obesity is a systemic disease characterized by chronic low-grade inflammation (Table 1).1–3 Also, obesity is one of the most prevalent non-communicable diseases worldwide. In the United States, it has doubled over the past decades, reaching a prevalence of 40% in adults, and an estimated 50% by 2030.4 In Spain, the current prevalence of obesity in adults is nearly 17%. Obesity is associated with an increase in inflammatory markers, such as tumor necrosis factor-alpha (TNF-α), C-reactive protein (CRP), and multiple cytokines, such as interleukins (IL) 6 and 18. Adipose tissue releases numerous proinflammatory mediators such as adiponectin, leptin, angiotensin II, resistin, visfatin, and IL-6.5 Obesity can also be considered an immunological disorder, as it is associated with a reduced immune capacity, and changes to the function of neutrophils, monocytes, lymphocytes, and macrophages.5 Additionally, it is associated with certain tumors (such as endometrial or colorectal cancer), cardiovascular disease, and changes to the microbiota.2,3 Given the complex pathophysiology of obesity and its association with an increase in proinflammatory mediators, hormones, and immune changes, it is not surprising that nearly 50% of obese patients present skin disorders.6
Obesity as a systemic disease.
| Disorder | Physiopathogenic mechanism |
|---|---|
| Chronic low-grade inflammationEndocrine disordersImmune disruptionPredisposition to certain cancersAtherosclerosis and early cardiovascular diseaseChanges to intestinal microbiota | Increased TNF-α, CRP, IL-6, IL-18, adiponectin, leptin, angiotensin II, resistin, and visfatin, among othersElevated levels of insulin, cortisol, epinephrine, and growth hormoneReduced immune capacity of neutrophils, monocytes, lymphocytes, and macrophagesChronic increase of inflammatory mediators, growth factors, and hormonal disruptionsLipid deposits in the intima layer of arteries, and increased inflammatory mediatorsIncreased pathogenic microorganisms and reduction of protective commensal bacteria |
IL, interleukin; CRP, C-reactive protein; TNF-α, tumor necrosis factor-alpha.
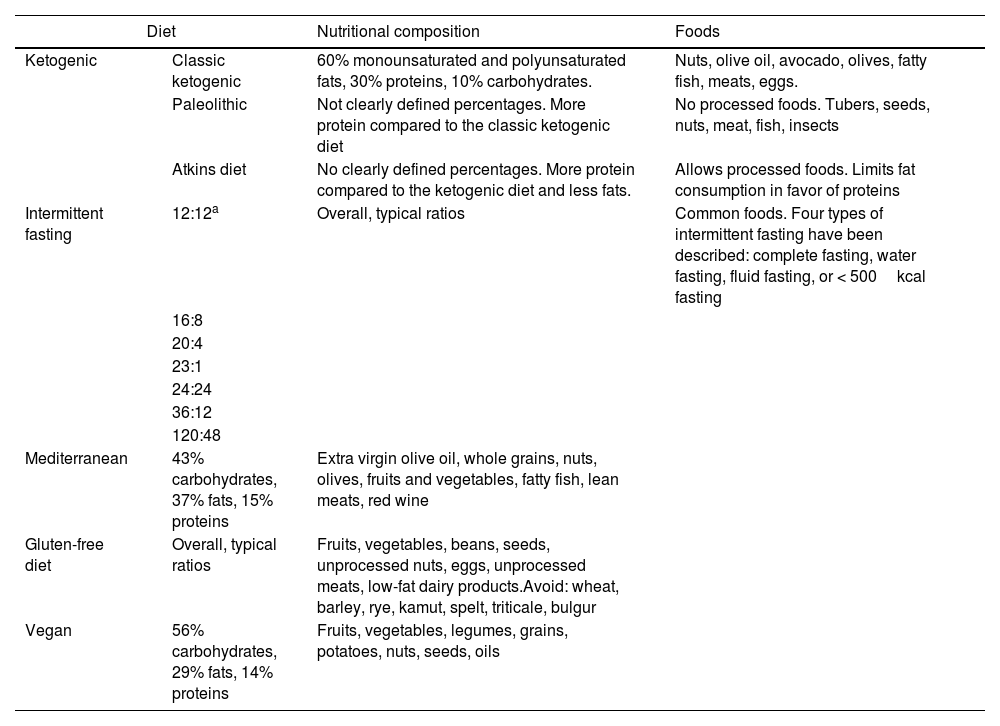
In recent years, a set of diets aimed at weight loss, improved physical capabilities, and management of various chronic diseases, whether cardiovascular, neurological, or dermatological, have proliferated. Among these diets, the ketogenic diet and intermittent fasting have shown very promising results in both traditional and sports medicine.7,8 Additionally, the Mediterranean diet has been established as a healthy eating pattern with a significant positive impact on health.9 Other popular diets include the “paleo” diet, the vegan diet, and the gluten-free diet (Table 2).
Characteristics of the most popular diets.
| Diet | Nutritional composition | Foods | |
|---|---|---|---|
| Ketogenic | Classic ketogenic | 60% monounsaturated and polyunsaturated fats, 30% proteins, 10% carbohydrates. | Nuts, olive oil, avocado, olives, fatty fish, meats, eggs. |
| Paleolithic | Not clearly defined percentages. More protein compared to the classic ketogenic diet | No processed foods. Tubers, seeds, nuts, meat, fish, insects | |
| Atkins diet | No clearly defined percentages. More protein compared to the ketogenic diet and less fats. | Allows processed foods. Limits fat consumption in favor of proteins | |
| Intermittent fasting | 12:12a | Overall, typical ratios | Common foods. Four types of intermittent fasting have been described: complete fasting, water fasting, fluid fasting, or < 500kcal fasting |
| 16:8 | |||
| 20:4 | |||
| 23:1 | |||
| 24:24 | |||
| 36:12 | |||
| 120:48 | |||
| Mediterranean | 43% carbohydrates, 37% fats, 15% proteins | Extra virgin olive oil, whole grains, nuts, olives, fruits and vegetables, fatty fish, lean meats, red wine | |
| Gluten-free diet | Overall, typical ratios | Fruits, vegetables, beans, seeds, unprocessed nuts, eggs, unprocessed meats, low-fat dairy products.Avoid: wheat, barley, rye, kamut, spelt, triticale, bulgur | |
| Vegan | 56% carbohydrates, 29% fats, 14% proteins | Fruits, vegetables, legumes, grains, potatoes, nuts, seeds, oils | |
Kcal, kilocalories.
Below we will be reviewing the impact of these popular diets on the skin and dermatological conditions.
Material and methodsThis was a narrative review of the scientific medical literature currenty available. From May through June 2023, were conducted searches on Medline and Google Scholar using the keyterms “diets,” “nutrition,” “skin,” “dermatoses,” “paleo,” “fasting,” “intermittent fasting,” “ketosis,” “ketogenic,” “gluten,” “vegan diet,” “psoriasis,” “acne,” “atopic dermatitis,” and “hidradenitis suppurativa.” This search was conducted in both Spanish and English. Articles were screened based on their abstracts and selected based on their relevance after a thorough review of the studies. Two authors (MMP, and JPC) conducted the search, article selection, and initial manuscript drafting. A third author (DMC) completed the search, and the manuscript drafting.
Ketogenic diet and intermittent fastingThe ketogenic diet involves the restriction of carbohydrate-rich foods (at least, 30g/day to 50g/day) such as cereals, ultraprocessed foods, and sugar, in favor of a diet based on proteins and healthy fats, such as monounsaturated fats (nuts, avocado, and olives), and polyunsaturated fats (fish). There are multiple variations of this diet, including the Atkins diet, the modified Atkins diet (60% fats, 30% proteins, and 10% carbohydrates), and the low-glycemic index diet, among many others.7 The goal of the diet is to induce ketosis to obtain the required energy from stored body fat.
Intermittent fasting involves the voluntary abstention from food, or liquids for some time. It should be differentiated from starvation, which results in a lack of essential nutrients and severe complications. There are numerous wasy of fasting, being the most common of all 12-hour fasting, 16-hour fasting (with an 8-hour eating window), 23-hour fasting (with a 1-hour eating window), 24-24 (24-hour fasting followed by 24hours of regular eating), 36-12 hour fasting (36hours of fasting followed by 12hours of regular eating), and 5:2 fasting (2 days of fasting followed by 5 days of regular eating), among many others.7,10 Intermittent fasting> 12hours induces fatty acid metabolism and ketone production.10
Adverse events and contraindications of the ketogenic diet and intermittent fastingAdverse events of these diets include dehydration, lethargy, hypoglycemia, acidosis, hydroelectrolyte and GI disorders.8 In recent years, numerous cases of prurigo pigmentosa associated with ketogenic diets have been described, popularly referred to as “keto rash.” It is characterized by pruritic and erythematous papules, plaques, or vesicles typically located on the trunk or neck evolving into retiform hyperpigmented plaques (Fig. 1). The appearance is characteristic, but the diagnosis can be challenging in the early stages of the disease (Fig. 2). The clinical picture often develops in just 1 month (ranging from 6 days to 4 months) after starting a strict ketogenic diet. The most widely recommended treatment is tetracyclines. Post-inflammatory hyperpigmentation is a complication in most patients.11
Prurigo pigmentosa, keto rash. Multiple coalescing erythematous papules of reticular appearance located on the back. Hyperpigmented reticular plaques can be seen on the lower back region. The patient suffered from an eating disorder and was undergoing treatment for depression. Complete resolution of pruritus and erythematous plaques was seen after a 1-month course of doxycycline 100mg/day.
Prurigo pigmentosa, keto rash. Highly pruritic erythematous plaques on the dorsal back region. Note the subtle reticulated post-inflammatory hyperpigmentation on the central dorsal back region. The patient had been following a strict ketogenic diet for 4 months, resulting in significant weight loss. The clinical condition completely resolved after a 1-month course of doxycycline 100mg/day, along with diet discontinuation.
Absolute contraindications for the ketogenic diet include porphyrias and pyruvate carboxylase deficiency, a rare neurometabolic disorder characterized by developmental delay, metabolic acidosis, and recurrent seizures in infancy.8 Some relative contraindications include certain mitochondrial cytopathies or carnitine deficiency.8 It is ill-advised for pregnant or breastfeeding women, young children, or patients with low weight, sepsis, liver or pancreatic failure, or severe lipid metabolism disorders.7
Systemic benefits of the ketogenic diet and intermittent fastingThe beneficial effects of the ketogenic diet and intermittent fasting can be categorized into anti-inflammatory effects, including the reduction of proinflammatory cytokines such as TNF-α, IL-6, and the suppression of the NLRP3 inflammasome, a key player in the activation of IL-1;8 metabolic effects, such as increased adiponectin and leptin, decreased ghrelin, increased insulin sensitivity, decreased fasting glucose and insulin, decreased glycosylated hemoglobin, and neuronal effects, with an increased brain-derived neurotrophic factor (BDNF), and enhanced neuronal plasticity, and regeneration.7 The ketogenic diet and intermittent fasting have shown promising results, although still in preliminary studies, in the management of diabetes, polycystic ovary syndrome, cancer, and various cardiovascular, neurodegenerative, and respiratory diseases.10,12
Ketogenic diet and intermittent fasting in cancer patientsA recent medical literature review of clinical trials and prospective case-control studies and cohorts with large samples revealed that ketogenic diet and intermittent fasting could be useful to optimize responses in cancer patients undergoing chemotherapy or radiotherapy, and therefore, improve quality of life for these individuals. However, these findings need to be confirmed in larger clinical trials to establish recommendations in the routine clinical practice.13.
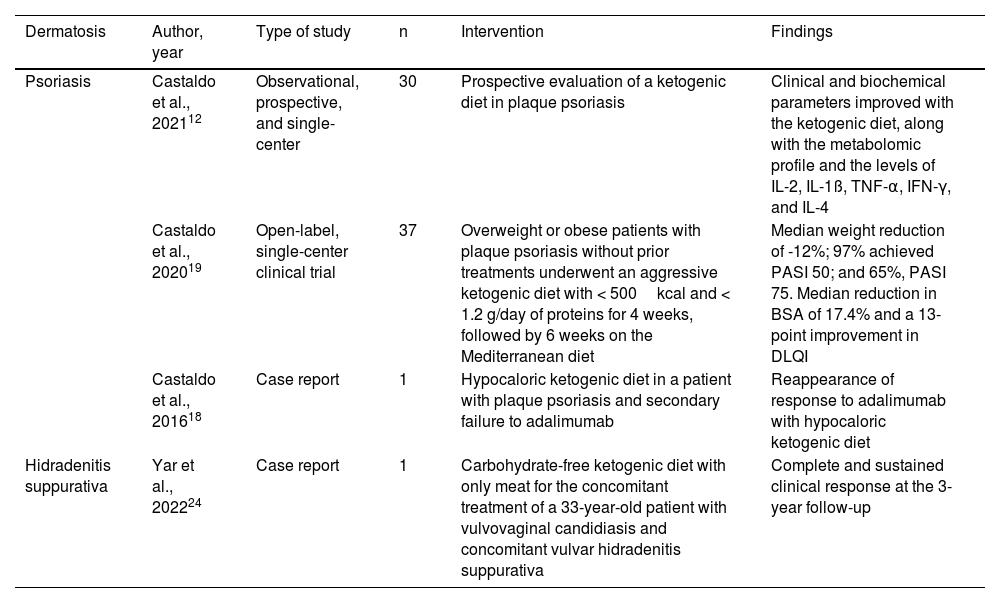
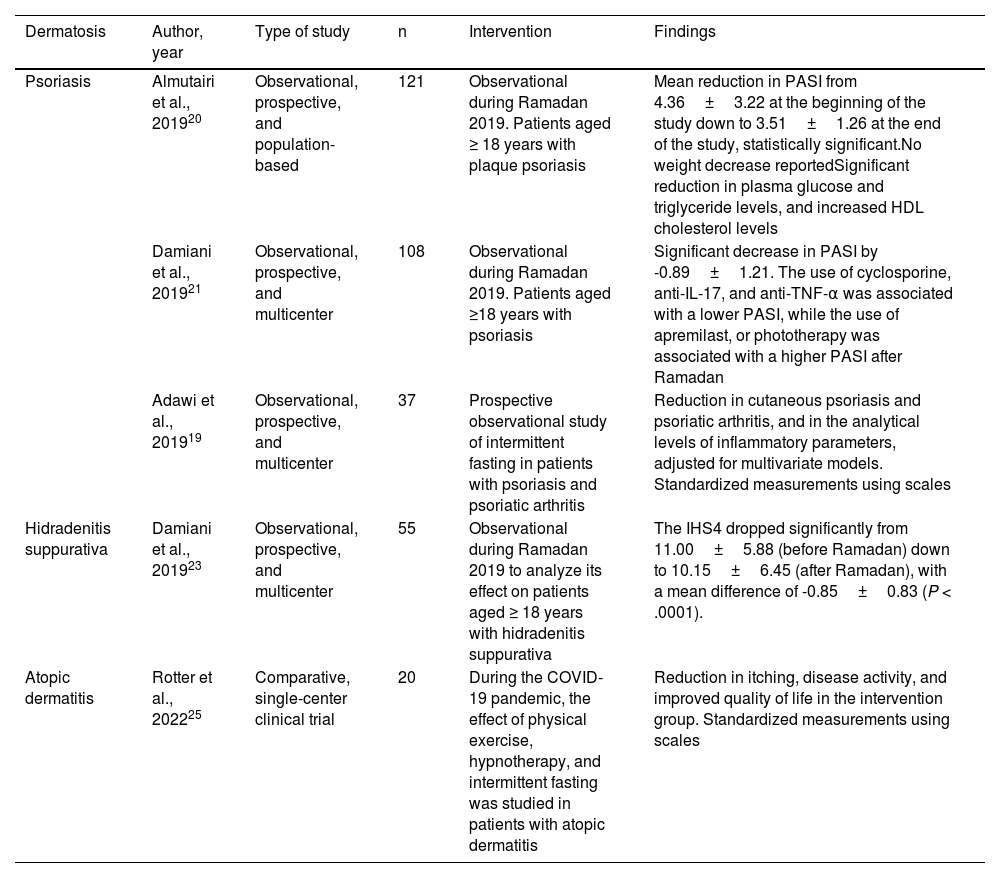
The impact of ketogenic diet and intermittent fasting on various dermatological conditions is shown in Tables 3 and 4.
Studies on the impact of the ketogenic diet on several dermatoses.
| Dermatosis | Author, year | Type of study | n | Intervention | Findings |
|---|---|---|---|---|---|
| Psoriasis | Castaldo et al., 202112 | Observational, prospective, and single-center | 30 | Prospective evaluation of a ketogenic diet in plaque psoriasis | Clinical and biochemical parameters improved with the ketogenic diet, along with the metabolomic profile and the levels of IL-2, IL-1ß, TNF-α, IFN-γ, and IL-4 |
| Castaldo et al., 202019 | Open-label, single-center clinical trial | 37 | Overweight or obese patients with plaque psoriasis without prior treatments underwent an aggressive ketogenic diet with < 500kcal and < 1.2 g/day of proteins for 4 weeks, followed by 6 weeks on the Mediterranean diet | Median weight reduction of -12%; 97% achieved PASI 50; and 65%, PASI 75. Median reduction in BSA of 17.4% and a 13-point improvement in DLQI | |
| Castaldo et al., 201618 | Case report | 1 | Hypocaloric ketogenic diet in a patient with plaque psoriasis and secondary failure to adalimumab | Reappearance of response to adalimumab with hypocaloric ketogenic diet | |
| Hidradenitis suppurativa | Yar et al., 202224 | Case report | 1 | Carbohydrate-free ketogenic diet with only meat for the concomitant treatment of a 33-year-old patient with vulvovaginal candidiasis and concomitant vulvar hidradenitis suppurativa | Complete and sustained clinical response at the 3-year follow-up |
BSA, body surface area; DLQI, Dermatology Life Quality Index; HDL, high-density lipoproteins; IFN-γ, interferon gamma; IHS-4, Severity of International Hidradenitis Suppurativa Severity Score System; IL, interleukin; Kcal, kilocalories; PASI, Psoriasis Area and Severity Index; TNF-α, tumor necrosis factor-alpha.
Studies on the impact of intermittent fasting on several dermatoses.
| Dermatosis | Author, year | Type of study | n | Intervention | Findings |
|---|---|---|---|---|---|
| Psoriasis | Almutairi et al., 201920 | Observational, prospective, and population-based | 121 | Observational during Ramadan 2019. Patients aged ≥ 18 years with plaque psoriasis | Mean reduction in PASI from 4.36±3.22 at the beginning of the study down to 3.51±1.26 at the end of the study, statistically significant.No weight decrease reportedSignificant reduction in plasma glucose and triglyceride levels, and increased HDL cholesterol levels |
| Damiani et al., 201921 | Observational, prospective, and multicenter | 108 | Observational during Ramadan 2019. Patients aged ≥18 years with psoriasis | Significant decrease in PASI by -0.89±1.21. The use of cyclosporine, anti-IL-17, and anti-TNF-α was associated with a lower PASI, while the use of apremilast, or phototherapy was associated with a higher PASI after Ramadan | |
| Adawi et al., 201919 | Observational, prospective, and multicenter | 37 | Prospective observational study of intermittent fasting in patients with psoriasis and psoriatic arthritis | Reduction in cutaneous psoriasis and psoriatic arthritis, and in the analytical levels of inflammatory parameters, adjusted for multivariate models. Standardized measurements using scales | |
| Hidradenitis suppurativa | Damiani et al., 201923 | Observational, prospective, and multicenter | 55 | Observational during Ramadan 2019 to analyze its effect on patients aged ≥ 18 years with hidradenitis suppurativa | The IHS4 dropped significantly from 11.00±5.88 (before Ramadan) down to 10.15±6.45 (after Ramadan), with a mean difference of -0.85±0.83 (P < .0001). |
| Atopic dermatitis | Rotter et al., 202225 | Comparative, single-center clinical trial | 20 | During the COVID-19 pandemic, the effect of physical exercise, hypnotherapy, and intermittent fasting was studied in patients with atopic dermatitis | Reduction in itching, disease activity, and improved quality of life in the intervention group. Standardized measurements using scales |
IHS-4, Severity of International Hidradenitis Suppurativa Severity Score System; IL, interleukin; PASI, Psoriasis Area and Severity Index; TNF-α, tumor necrosis factor-alpha.
Several studies have shown that dietary restriction and intermittent fasting have antioxidant and anti-inflammatory effects, and could be beneficial for health. Studies in animal models suggest that they may even reduce skin aging,14 and extend survival.15 A recent clinical trial (n=45) demonstrated more skin hydration and optimization of skin texture in a group treated with intermittent fasting. Additionally, these individuals reported higher levels of happiness and confidence.16
PsoriasisGiven the association described among psoriasis, obesity, and chronic inflammation, the ketogenic diet—one of the most effective interventions for weight and chronic inflammation markers reduction—may be an effective alternative in the management of this dermatosis.17,18 A 30-patient prospective study followed for 1 month showed a reduction of the Psoriasis Area Severity Index (PASI) by nearly 50%. There was also a significant reduction of the Dermatology Life Quality Index (DLQI), pruritus, and pain scales in patients treated with a calorie-restricted, high-protein diet for 4 weeks. These individuals also exhibited lower serum levels of IL-2 and IL-1β, and total cholesterol, LDL cholesterol, insulin, and liver enzyme levels.12 A previous clinical trial (n=37) of patients with treatment-naïve psoriasis had already shown a significant reduction in PASI, with 97% of individuals reaching PASI 50, and 65% PASI 75 just with a 10-week dietary regimen consisting of a 4-week very-low-calorie ketogenic diet (< 500kcal/day), followed by a 6-week low-calorie Mediterranean diet.19
Regarding intermittent fasting, a prospective study (n=121) conducted during the 2019 Ramadan fasting period revaled a significant reduction of psoriasis (initial baseline PASI of 4.36±3.22, and final PASI of 3.51±1.26).20 Previously, a different multicenter prospective trial (n=108) had already described a significant reduction in PASI in patients with moderate-to-severe psoriasis during the month of Ramadan.21 The results of a randomized clinical trial (n=24) comparing a regular diet (n=12) to intermittent fasting (n=12) for 12 weeks in the management of psoriasis are pending publication.22
Hidradenitis suppurativaIn a multicenter prospective trial (n=55), intermittent fasting during the Ramadan month was associated with a modest reduction in the Severity of International Hidradenitis Suppurativa Severity Score System (IHS4), from 11.00±5.88 points (before Ramadan) down to 10.15±6.45 (after Ramadan) (P <.0001). Also, the number of severe lesions, such as draining fistulas and abscesses, dropped> 70% of the study participants.23 Recently, the case of a 33-year-old obese woman with genital hidradenitis was reported. After starting a strict ketogenic diet, she experienced complete resolution of her skin condition, which was maintained across the 3-year follow-up.24
AcneA recent narrative review of prospective and retrospective trials with varying sample sizes and methodological quality (case reports, case series, prospective and retrospective cohort studies) suggested that ketogenic diet could reduce acne by decreasing insulin secretion compared to the Western diet, which induces insulin spikes.8,25
Atopic dermatitisA recent single-center randomized clinical trial (n=20) conducted during the SARS-CoV-2 pandemic found a reduction in itching, disease activity, and quality of life in patients treated with intermittent fasting and hypnotherapy vs the control group at 16 weeks.26
Autoinflammatory dermatoses and NLRP3 inflammasome suppressionIn a preclinical study, Youm et al.27 reported that β-hydroxybutyrate, a ketone body naturally circulating in humans, specifically suppresses the NLRP3 inflammasome, which activates IL-1β and is associated with multiple dermatoses including familial cold-induced autoinflammatory syndrome, Muckle-Wells syndrome, neonatal-onset multisystemic inflammatory disease, chronic infantile neurological cutaneous and articular syndrome, hyperimmunoglobulinemia D with periodic fever, tumor necrosis factor receptor-associated periodic syndrome (TRAPS), juvenile idiopathic arthritis, relapsing polychondritis, Schnitzler syndrome, Sweet's syndrome, Behçet's disease, gout, and hidradenitis suppurativa. Therefore, they proposed that the ketogenic diet could be used therapeutically to treat all these dermatoses, although confirmatory clinical trials are still lacking.27
Paleo dietThe paleolithic diet, also known as the “paleo” diet, argues that our body has not successfully adapted to the changes occurred after the adoption of agriculture and sedentary lifestyle. Paleo diet can be considered a variant of the ketogenic diet: the only foods allowed are those obtained through hunting and gathering, such as fruits, vegetables, fish, meat, and eggs.28 Dairy products, refined flours, cereals, legumes, refined sugar, processed food, and alcohol are prohibited. A recent 12-week randomized clinical trial of 32 participants demonstrated its benefits in increasing insulin sensitivity, reducing plasma lipids, and promoting weight loss, meaning it could be part of the management of diseases associated with metabolic disorders and obesity.29 Additionally, a cross-sectional study (n=435) conducted in Iran associated the paleo diet with lower levels of depression, anxiety, and stress.30 However, no studies have confirmed its specific utility in dermatological diseases.
Mediterranean dietMediterranean diet is characterized by the consumption of polyphenols from healthy foods such as fruits and vegetables, legumes, olive oil, grains, seeds, and fish, with a reduced amount of animal fats. Polyphenols have potent anti-inflammatory and antioxidant effects. Adherence to the Mediterranean diet has been shown to reduce cardiovascular events in long-term prospective trials,9 and be a valuable adjunct in the management of multiple chronic inflammatory diseases.31 Additionally, recent cross-sectional studies have associated it with greater well-being,32 and lower levels of depression and anxiety.30.
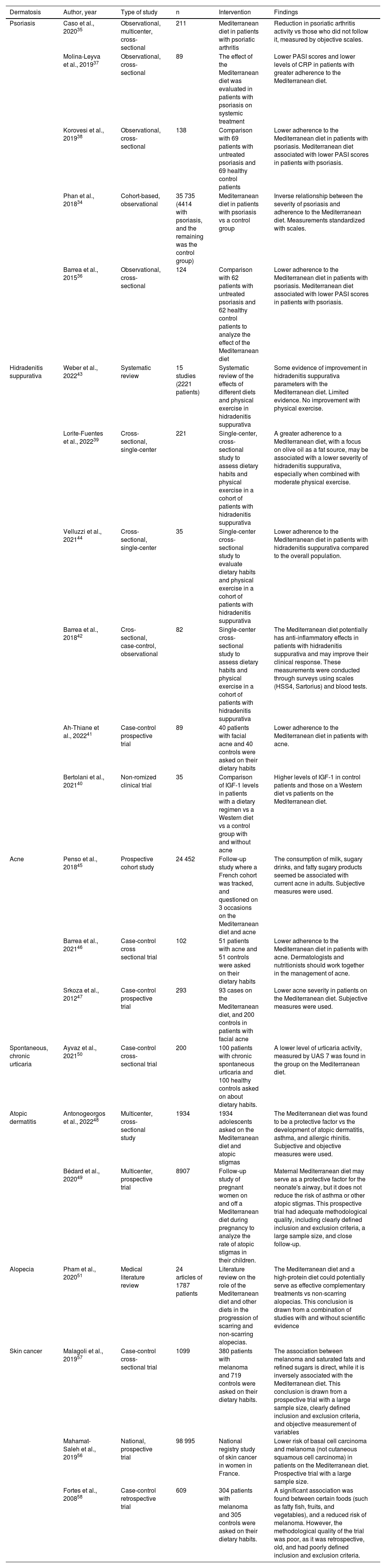
Mediterranean diet and dermatosis (Table 5)Psoriasisrecent narrative review suggested an association between diet and psoriasis activity.33 In a French cohort study, a questionnaire sent to 35 735 patients with psoriasis revealed a low adherence to the Mediterranean diet in these individuals.34 A recent multicenter cross-sectional trial (n=211) found an inverse association between following the Mediterranean diet and the activity of psoriatic arthritis measured through the Disease Activity index for Psoriatic Arthritis (DAPSA).35 Another comparative cross-sectional trial (n=124) of patients with psoriasis on the Mediterranean diet (n=62) vs those who did not follow it (n=62) revealed that higher consumption of extra virgin olive oil was associated with lower psoriasis severity, both in terms of PASI and inflammatory activity in blood tests. This was attributed to oleocanthal, a phenolic compound with potent anti-inflammatory effects.36 Other studies supporting the benefits of Mediterranean diet in the management of psoriasis are listed in Table 5.37,38
Studies on the impact of the Mediterranean diet on several dermatoses.
| Dermatosis | Author, year | Type of study | n | Intervention | Findings |
|---|---|---|---|---|---|
| Psoriasis | Caso et al., 202035 | Observational, multicenter, cross-sectional | 211 | Mediterranean diet in patients with psoriatic arthritis | Reduction in psoriatic arthritis activity vs those who did not follow it, measured by objective scales. |
| Molina-Leyva et al., 201937 | Observational, cross-sectional | 89 | The effect of the Mediterranean diet was evaluated in patients with psoriasis on systemic treatment | Lower PASI scores and lower levels of CRP in patients with greater adherence to the Mediterranean diet. | |
| Korovesi et al., 201938 | Observational, cross-sectional | 138 | Comparison with 69 patients with untreated psoriasis and 69 healthy control patients | Lower adherence to the Mediterranean diet in patients with psoriasis. Mediterranean diet associated with lower PASI scores in patients with psoriasis. | |
| Phan et al., 201834 | Cohort-based, observational | 35 735 (4414 with psoriasis, and the remaining was the control group) | Mediterranean diet in patients with psoriasis vs a control group | Inverse relationship between the severity of psoriasis and adherence to the Mediterranean diet. Measurements standardized with scales. | |
| Barrea et al., 201536 | Observational, cross-sectional | 124 | Comparison with 62 patients with untreated psoriasis and 62 healthy control patients to analyze the effect of the Mediterranean diet | Lower adherence to the Mediterranean diet in patients with psoriasis. Mediterranean diet associated with lower PASI scores in patients with psoriasis. | |
| Hidradenitis suppurativa | Weber et al., 202243 | Systematic review | 15 studies (2221 patients) | Systematic review of the effects of different diets and physical exercise in hidradenitis suppurativa | Some evidence of improvement in hidradenitis suppurativa parameters with the Mediterranean diet. Limited evidence. No improvement with physical exercise. |
| Lorite-Fuentes et al., 202239 | Cross-sectional, single-center | 221 | Single-center, cross-sectional study to assess dietary habits and physical exercise in a cohort of patients with hidradenitis suppurativa | A greater adherence to a Mediterranean diet, with a focus on olive oil as a fat source, may be associated with a lower severity of hidradenitis suppurativa, especially when combined with moderate physical exercise. | |
| Velluzzi et al., 202144 | Cross-sectional, single-center | 35 | Single-center cross-sectional study to evaluate dietary habits and physical exercise in a cohort of patients with hidradenitis suppurativa | Lower adherence to the Mediterranean diet in patients with hidradenitis suppurativa compared to the overall population. | |
| Barrea et al., 201842 | Cros-sectional, case-control, observational | 82 | Single-center cross-sectional study to assess dietary habits and physical exercise in a cohort of patients with hidradenitis suppurativa | The Mediterranean diet potentially has anti-inflammatory effects in patients with hidradenitis suppurativa and may improve their clinical response. These measurements were conducted through surveys using scales (HSS4, Sartorius) and blood tests. | |
| Ah-Thiane et al., 202241 | Case-control prospective trial | 89 | 40 patients with facial acne and 40 controls were asked on their dietary habits | Lower adherence to the Mediterranean diet in patients with acne. | |
| Bertolani et al., 202140 | Non-romized clinical trial | 35 | Comparison of IGF-1 levels in patients with a dietary regimen vs a Western diet vs a control group with and without acne | Higher levels of IGF-1 in control patients and those on a Western diet vs patients on the Mediterranean diet. | |
| Acne | Penso et al., 201845 | Prospective cohort study | 24 452 | Follow-up study where a French cohort was tracked, and questioned on 3 occasions on the Mediterranean diet and acne | The consumption of milk, sugary drinks, and fatty sugary products seemed be associated with current acne in adults. Subjective measures were used. |
| Barrea et al., 202146 | Case-control cross sectional trial | 102 | 51 patients with acne and 51 controls were asked on their dietary habits | Lower adherence to the Mediterranean diet in patients with acne. Dermatologists and nutritionists should work together in the management of acne. | |
| Srkoza et al., 201247 | Case-control prospective trial | 293 | 93 cases on the Mediterranean diet, and 200 controls in patients with facial acne | Lower acne severity in patients on the Mediterranean diet. Subjective measures were used. | |
| Spontaneous, chronic urticaria | Ayvaz et al., 202150 | Case-control cross-sectional trial | 200 | 100 patients with chronic spontaneous urticaria and 100 healthy controls asked on about dietary habits. | A lower level of urticaria activity, measured by UAS 7 was found in the group on the Mediterranean diet. |
| Atopic dermatitis | Antonogeorgos et al., 202248 | Multicenter, cross-sectional study | 1934 | 1934 adolescents asked on the Mediterranean diet and atopic stigmas | The Mediterranean diet was found to be a protective factor vs the development of atopic dermatitis, asthma, and allergic rhinitis. Subjective and objective measures were used. |
| Bédard et al., 202049 | Multicenter, prospective trial | 8907 | Follow-up study of pregnant women on and off a Mediterranean diet during pregnancy to analyze the rate of atopic stigmas in their children. | Maternal Mediterranean diet may serve as a protective factor for the neonate's airway, but it does not reduce the risk of asthma or other atopic stigmas. This prospective trial had adequate methodological quality, including clearly defined inclusion and exclusion criteria, a large sample size, and close follow-up. | |
| Alopecia | Pham et al., 202051 | Medical literature review | 24 articles of 1787 patients | Literature review on the role of the Mediterranean diet and other diets in the progression of scarring and non-scarring alopecias. | The Mediterranean diet and a high-protein diet could potentially serve as effective complementary treatments vs non-scarring alopecias. This conclusion is drawn from a combination of studies with and without scientific evidence |
| Skin cancer | Malagoli et al., 201957 | Case-control cross-sectional trial | 1099 | 380 patients with melanoma and 719 controls were asked on their dietary habits. | The association between melanoma and saturated fats and refined sugars is direct, while it is inversely associated with the Mediterranean diet. This conclusion is drawn from a prospective trial with a large sample size, clearly defined inclusion and exclusion criteria, and objective measurement of variables |
| Mahamat-Saleh et al., 201956 | National, prospective trial | 98 995 | National registry study of skin cancer in women in France. | Lower risk of basal cell carcinoma and melanoma (not cutaneous squamous cell carcinoma) in patients on the Mediterranean diet. Prospective trial with a large sample size. | |
| Fortes et al., 200858 | Case-control retrospective trial | 609 | 304 patients with melanoma and 305 controls were asked on their dietary habits. | A significant association was found between certain foods (such as fatty fish, fruits, and vegetables), and a reduced risk of melanoma. However, the methodological quality of the trial was poor, as it was retrospective, old, and had poorly defined inclusion and exclusion criteria. |
IGF-1, Insulin-like Growth Factor 1; IL, interleukin; PASI, Psoriasis Area and Severity Index; CRP, C-reactive protein; UAS 7, Urticaria Activity Score 7.
In a single-center, observational study (n=221) of patients with hidradenitis suppurativa, following the Mediterranean diet was associated with lower disease activity and lower Hurley stages (self-reported) and IHS4. The use of extra virgin olive oil was the dietary factor most strongly associated with reduced hidradenitis activity.39 Former studies had already shown an inverse association between adherence to the Mediterranean diet and the Sartorius index.40,41 A single-center cross-sectional study (n=82) revealed that the Mediterranean diet, when combined with moderate physical activity, was associated with better outcomes in the management of hidradenitis suppurativa.42 Other studies on the role of the Mediterranean diet in hidradenitis suppurativa are shown in Table 5.43,44
AcneThe association of acne with the consumption of dairy prodicts, foods high in sugars, sugary beverages, and other high-glycemic index foods has been described in multiple studies, including follow-up cohorts of over 24 000 patients.45 A recent French case-control study (n=90) revealed a linear association and a negative correlation between adherence to the Mediterranean diet and the severity of acne.41 In other words, greater adherence to the Mediterranean diet was associated with a lower likelihood of experiencing severe acne.41 A previous cross-sectional study (n=35) had hypothesized that there is an association between the Mediterranean diet and lower levels of insulin-like growth factor 1 (IGF-1),40 an agent implicated in the pathophysiology of acne. Other studies assessing the role of the Mediterranean diet in acne are shown in Table 5.
Atopic dermatitisIn a large multicenter national series (n=1934), a relationship was described between the Mediterranean diet and a lower incidence of atopic dermatitis, allergic rhinitis, and asthma.48 However, this could not be confirmed in a prospective observational trial (n=8907) that did not corroborate that Mediterranean diet in pregnant women protects vs the development of atopic dermatitis in childhood.49
Chronic spontaneous urticariaA cross-sectional study (n=200) reported lower activity levels in patients with chronic spontaneous urticaria on the Mediterranean diet.50 However, this has not been confirmed in subsequent series to date.
AlopeciaA recent literature narrative review (24 articles with 1787 patients) suggested that the Mediterranean diet and a high-protein diet could be effective complementary treatments in the management of non-scarring alopecia.51
Skin neoplasmsA recent multicenter prospective trial (n=91) of patients with advanced melanoma who started immunotherapy with checkpoint inhibitors described a positive association between following the Mediterranean diet and the overall response and progression-free survival at 12 months, as well as fewer adverse events.52 It is postulated that the Mediterranean diet would increase short-chain fatty acid-producing bacteria, while higher concentrations of these acids in fecal matter have been associated with better responses to immunotherapy.53
Several case-control studies that included preclinical and clinical data suggest that the Mediterranean diet is associated with a lower risk of basal cell carcinoma, mainly due to the high intake of polyphenol-rich fruits. Natural polyphenols would be protective vs radiation-induced inflammation, oxidative stress, DNA damage, and immunosuppression.54,55
A cross-sectional study of over 90 000 women in France registered between 1993 and 2008 revealed that the Mediterranean diet was associated with a lower risk of basal cell carcinoma and melanoma, but not squamous cell carcinoma.56 Other studies on the relationship between skin cancer and the Mediterranean diet are listed in Table 5.57,58
Gluten-free dietGluten is a protein found in wheat, barley, and rye. Gluten sensitivity induces an abnormal immune response in certain individuals, triggering celiac disease, and causing intestinal atrophy and the disruption of nutrient absorption. At the skin level, it can lead to dermatitis herpetiformis.59 The overall prevalence of celiac disease is nearly 1%.60
In recent years, following gluten-free diets has become popular in the management of various chronic diseases. In most cases, the evidence is limited and controversial. In a recent single-center cross-sectional study of patients with psoriasis (n=1621), 5% had started a gluten-free diet on their own to control psoriasis.61 Similar results were seen in a study of 1571 patients with acne.62 A recent literature narrative review (of 49 studies and over 1000 patients) suggests that there is an association between gluten sensitivity and various dermatoses, such as psoriasis, palmoplantar pustulosis, and aphthous stomatitis, and these conditions could potentially benefit from gluten-free diets in patients with demonstrated gluten sensitivity. However, these authors do not recommend systematic screening for gluten sensitivity in these individuals. Still, systematic screening could be considered in selected cases refractory to conventional treatments. In the same review, other dermatoses that could benefit from an association with gluten are also suggested, including dermatomyositis, alopecia areata, urticaria, IgA linear bullous dermatosis, lupus erythematosus, or vitiligo.59 Regarding vitiligo, both diseases are primarily mediated by T cells and IL-2, IL-6, IL-17, and IL-21.60 In a single-center prospective study of 174 patients with vitiligo, 5 of them (2.8%) were diagnosed with celiac disease, a higher prevalence compared to that of the overall population.63
In relation to psoriasis, a single-center prospective trial from 2000 demonstrated an improvement in psoriasis-related lesions in patients with celiac disease and positive antigliadin antibodies at the 3-month follow-up.64 These results have been supported by a recent meta-analysis (of 18 studies and over 1000 patients) that showed a positive association between celiac disease and psoriasis, which would be explained by a common inflammatory link.65
Vegan dietThe vegan diet is a strict vegetarian diet which avoids the consumption of meat, animal-derived foods such as dairy products, eggs, honey, and gelatin. Strict vegan diets can lead to various nutritional deficiencies, including iron and B-complex vitamin deficiencies.66 Multiple cases of pellagra have been described in these individuals as well.67 It is advisable for vegans to consider supplementing with B-complex vitamins.68 Multiple studies have associated this diet with depressive disorders too. Two recent systematic reviews showed different results: the first found a higher risk of depression and anxiety associated with this diet,69 while the second did not demonstrate that there was a clear association between depression and the vegan diet.70
Despite the scarce evidence available and controversy surrounding this diet, a balanced intake of vegetables and legumes is proposed as a useful tool in managing various dermatoses such as acne, psoriasis, and atopic dermatitis.68 A national survey of over 1000 patients reported overall fewer skin lesions and lower severity in patients with psoriasis treated with vegan diets compared to those who were not on such diets.71 However, a single-center prospective study (n=60) described more adverse events and delayed healing in vegan patients treated with photodynamic therapy for the management of actinic keratosis vs omnivorous individuals.72 Similarly, wound healing after surgical excision of skin tumors could be worse in vegan patients, with higher rates of dehiscence being reported, more frequent atrophic scars, and a worse overall scar appearance. This was demonstrated in a prospective trial (n=42) that compared vegan and non-vegan patients 6 months after surgery.66 As for the response to fractional radiofrequency as an anti-aging treatment, a comparative prospective trial (n=60) found that vegans had poorer mid and long-term responses compared to omnivores.73 Additionally, it has been reported that vegan patients may have a high consumption of furocoumarins and a more adverse events with UVB phototherapy compared to vegetarians or omnivores, suggesting that phototherapy protocols should be adapted in these cases.74
DiscussionDespite the therapeutic revolution represented by biologic drugs and targeted molecules in Dermatology, it is essential to address modifiable factors such as diet, and dermatologists can play a crucial role in recommending interventions in this regard. In our routine clinical practice, it is not unusual to encounter patients who follow popular diets such as the ketogenic one, intermittent fasting, vegan diet, gluten-free diet, or the “paleo” diet, or who want to know more about the benefits of these dietary regimens in the management of their dermatological diseases. The Mediterranean diet, the ketogenic diet, and intermittent fasting have the highest level of evidence to date in the management of chronic inflammatory diseases, including cardiovascular, metabolic, neurodegenerative diseases, and inflammatory dermatoses. The ketogenic diet and intermittent fasting have been associated with reduced cutaneous and articular activity in psoriasis, and better disease control in hidradenitis suppurativa, or in other entities such as acne, or atopic dermatitis. The Mediterranean diet has also been associated with better disease progresion in patients with psoriasis, hidradenitis suppurativa, acne, atopic eczema, chronic spontaneous urticaria, alopecia, and even skin cancer. Additionally, the Mediterranean diet is one of the most sustainable diets ecologically speaking.75 However, most studies conducted with these diets in Dermatology are retrospective, or case-control studies, or exhibit obvious methodological biases that hinder the generalization of these findings.
Regarding the gluten-free diet, although there might be an association between gluten sensitivity and certain dermatoses, empirically speaking, it should not be prescribed, or recommended for overall gluten sensitivity screenings.59 Similarly, very restrictive diets such as the vegan one can delay wound healing, and induce a series of adverse events after dermatological procedures.72–74
LimitationsThis article is limited in that it is a narrative, non-systematic review of the medical literature currently available. Additionally, many of the studies included have low methodological quality, with many having small sample sizes, no clear definition of inclusion criteria, and being retrospective in nature. Both these factors make it difficult to generalize the findings and conclusions reported.
ConclusionsMultiple diets have gained popularity in recent years. The Mediterranean diet, the ketogenic diet, and intermittent fasting could be an additional therapeutic tool in the management of various chronic inflammatory dermatoses, or even play a role in reducing the incidence of malignant skin tumors. However, more studies are needed to corroborate these results and make recommendations with a higher level of evidence, and determine which diet is superior in the management of these diseases.
Conflicts of interestNone declared.