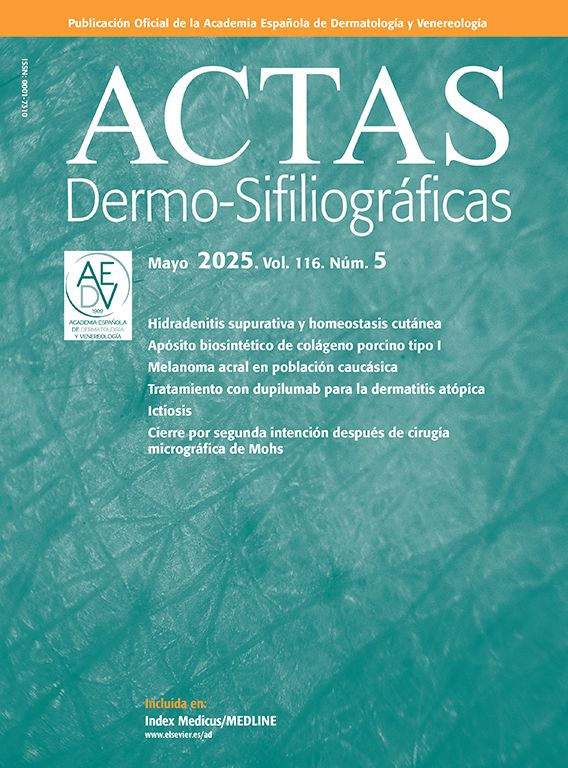
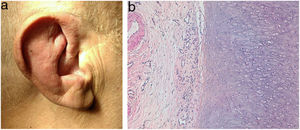
A 71-year-old man presented with a 6-month history recurrent inflammation of the pinnae (Fig. 1A) that led to a diagnosis of relapsing polychondritis. Additionally, he showed erythematous nodular lesions on both his trunk and extremities.
The patient reported a 21kg weight loss over the past 12 months, without associated fever. Bilateral episcleritis, atrial fibrillation, recurrent epididymitis, and pancytopenia were some of the patient's concomitant medical problems.
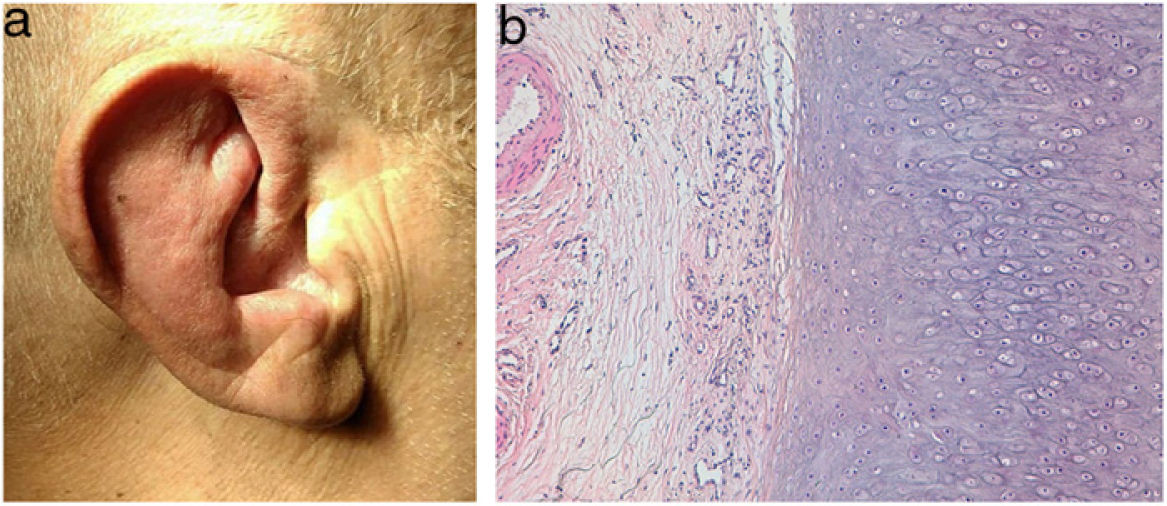
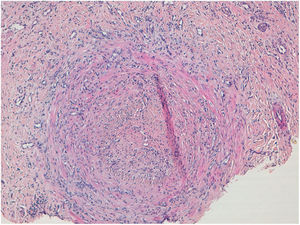
HistopathologyThe histopathological examination of the auricular cartilage revealed the presence of lymphocytic infiltration in the perichondrium (Fig. 1B), and the biopsy of cutaneous nodular lesions showed medium-sized artery vasculitis (Fig. 2), with a predominantly neutrophilic inflammatory infiltrate in the vascular wall, and vascular lumen occlusion.
Supplementary testsAcute phase reactants were elevated, with ferritin levels of 6830 (normal range from 20 to 250) and CRP levels of 130 (normal range from 0 to 5).
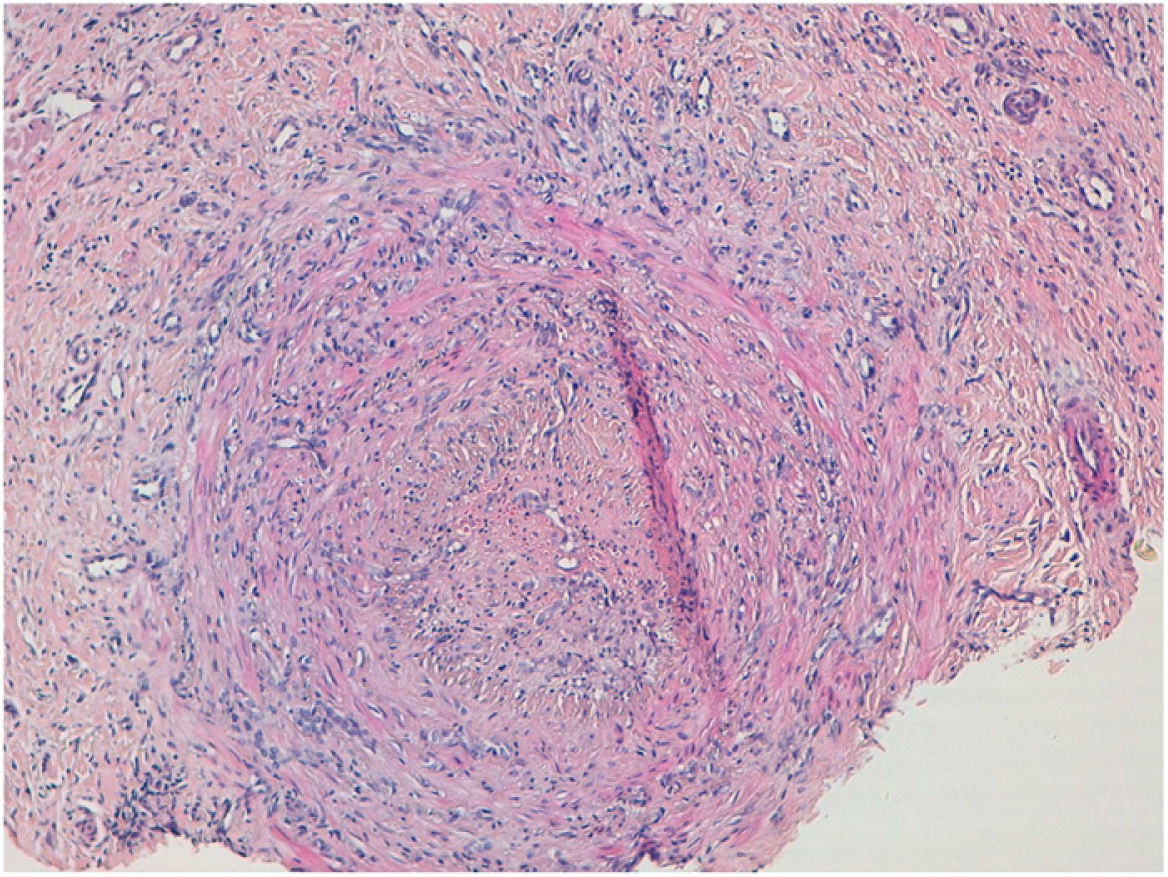
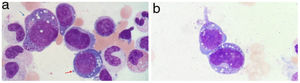
A bone marrow aspirate was performed to study pancytopenia, which revealed the presence of multilineage dysplasia and prominent cytoplasmic and nuclear vacuolization of myeloid and erythroid precursors (Fig. 3A and 3B).
A: Vacuolization of the nucleus and cytoplasm of myeloid (blue arrow) and erythroid (red arrow) precursors in the bone marrow aspirate. May-Grunwald-Giemsa, ×100. B: Vacuolization of the nucleus and cytoplasm of myeloid precursors in bone marrow aspirate. May-Grunwald-Giemsa, ×100.
For the diagnostic confirmation of the suspected syndrome, the UBA1 gene analysis performed confirmed the c.122T>C, p.(Met41Thr) mutation.
What is the diagnosis?
DiagnosisVEXAS syndrome (Vacuoles, E1 enzyme, X-linked, Autoinflammatory, Somatic).
Treatment and evolutionThe patient received off-label treatment with adalimumab but passed away 5 months after diagnosis.
CommentVEXAS syndrome is an adult-onset autoinflammatory condition first described by Beck et al. in December 2020.1 It is due to a somatic mutation of the UBA1 gene that causes dysfunctional ubiquitination and consequent proteotoxic stress with activation of innate immunity. It has mainly been described in middle-aged men.2
Patients develop systemic signs and symptoms such as fever, fatigue, and weight loss, with skin lesions in up to 83% of the cases,2 often in the form of erythematous-violaceous papules and nodules. The predominant histopathological pattern of such lesions is neutrophilic infiltration, with or without vasculitis. A total of 32% of the patients from Beck et al.’s series had previously been diagnosed with Sweet's syndrome, and 12% with polyarteritis nodosa.1 However, cases have also been reported where skin biopsies confirmed the presence of perivascular lymphocytic infiltrates without neutrophils or vasculitis.3 Other cutaneous findings associated with this entity include livedo racemosa and relapsing polychondritis in up to 64% of the patients.4
Hematological signs are characterized by cytopenias, myelodysplastic syndrome, and vacuolization of myeloid and erythroid precursors in bone marrow biopsies.1 However, precursor vacuolization is not pathognomonic of this entity and can also occur in alcoholic patients, those with copper deficiency, or due to myeloid neoplasms.
Other clinical signs of the VEXAS syndrome include arthritis, serositis, episcleritis, scleritis, pericarditis, myocarditis, neutrophilic alveolitis, epididymitis, large-vessel vasculitis, venous thromboembolism, abdominal pain, and GI bleeding.2 Elevated acute phase reactants are often seen too in the blood tests.
The disease often has an aggressive course. However, since this entity has been recently described, these data should be interpreted with caution, because milder cases may still go unnoticed, and genetic testing are only often performed in patients with more severe clinical signs. It has recently been observed that patients with the p.Met41Leu mutation in UBA1 gene may have a better prognosis.2
The proper management of this syndrome has not been standardized yet. A plethora of drugs has been suggested, including systemic corticosteroids, azathioprine, methotrexate, mycophenolate, cyclophosphamide, anti-IL-1, anti-IL-6, anti-TNF, rituximab, IV immunoglobulins, abatacept, and anti-JAK, with variable results.5 Recently, allogeneic hematopoietic stem cell transplantation has been proposed as an option with promising and sustained results.6
VEXAS syndrome is a complex, recently described entity with a fatal course in most cases. Therefore, awareness of this condition is important to facilitate early diagnosis and treatment. Targeted molecular therapy to restore ubiquitination in these patients may join the therapeutic arsenal in the coming future.
FundingNone declared.
Conflicts of interestNone declared.