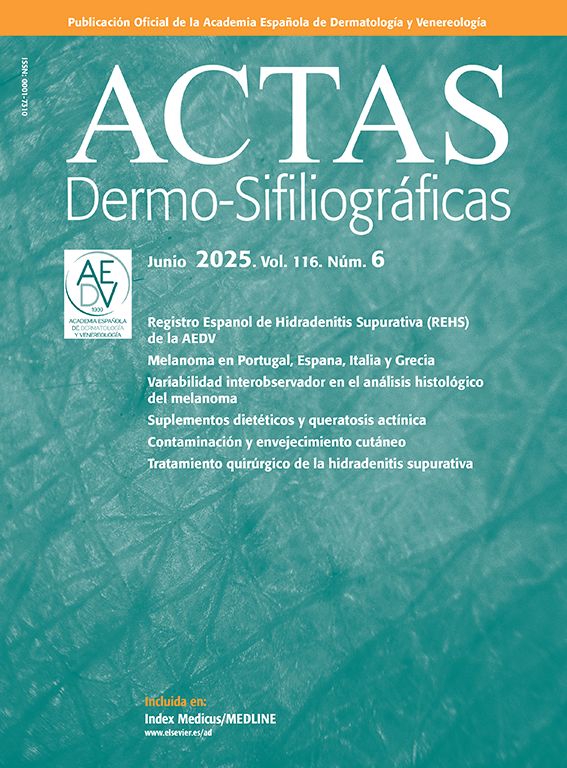
A 22-year-old man visited our department for assessment of loss of patches of hair that had begun 2 weeks earlier. Physical examination revealed small areas of alopecia distributed in the temporal and occipital regions, with no accompanying erythema or scaling (Fig. 1).
What is Your Diagnosis?
Syphilitic alopecia.
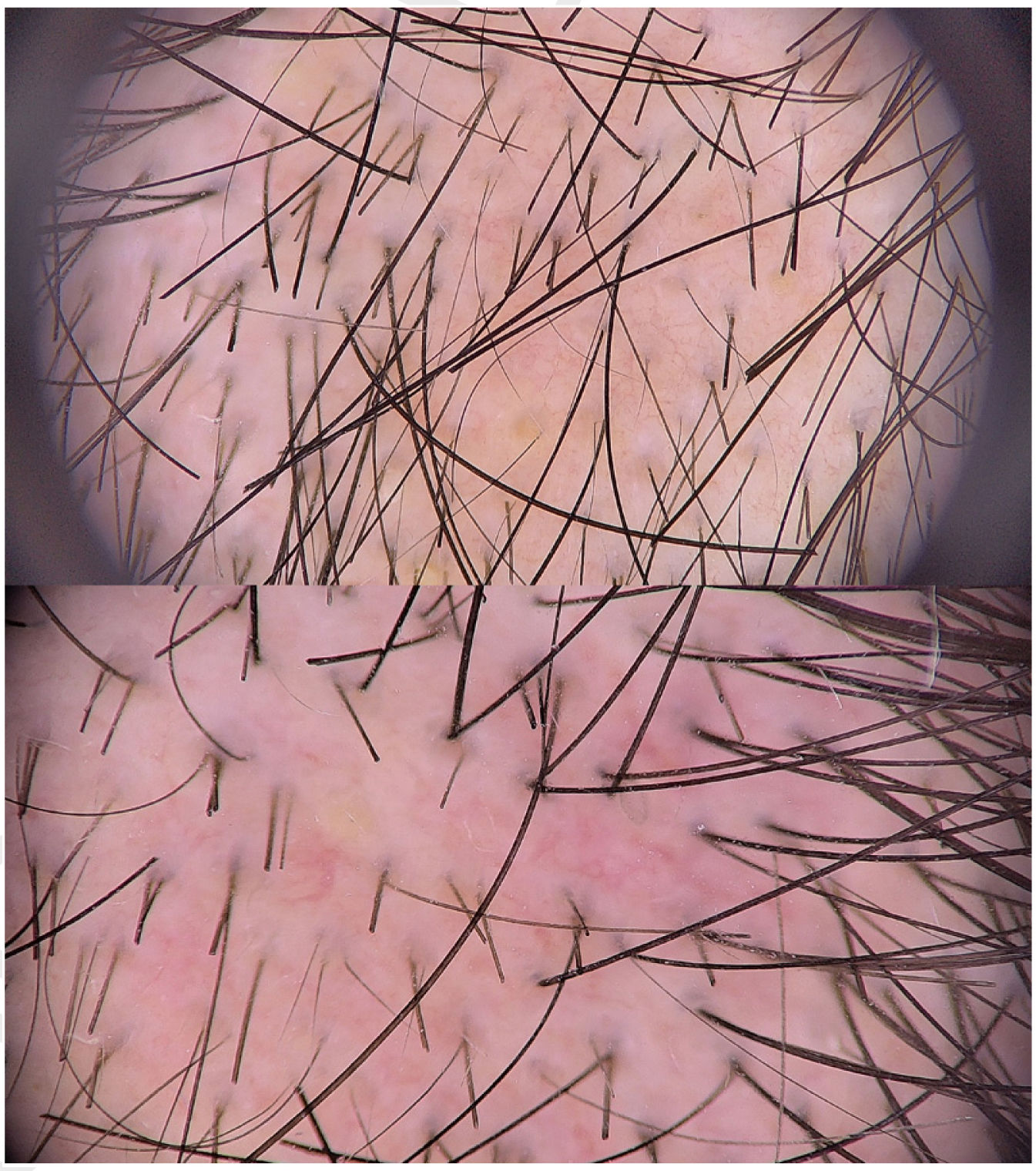
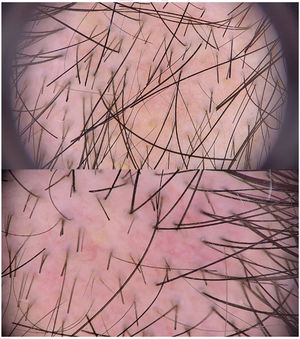
CommentDermoscopy findings are shown in Fig. 2. A directed history allowed for clinical suspicion of secondary syphilis. Serology positive for treponema and with an RPR titer of 1/16 confirmed this diagnosis.
Syphilitic alopecia is a rare clinical manifestation of secondary syphilis. Depending on its pattern (moth-eaten or diffuse), it may produce clinical findings similar to those of other nonscarring alopecias, such as alopecia areata, trichotillomania, or telogen effluvium. It is considered to be essential syphilitic alopecia when no evidence of other mucocutaneous disease exists (as in our case), which make diagnosis difficult.
Few dermoscopic findings of syphilitic alopecia have been described in the literature to date. In 2014, Ye et al. first described trichoscopy in a patient with moth-eaten syphilitic alopecia, in which they identified black spots, focal alopecia, hypopigmentation of the hair shaft, and yellow spots.1 Subsequent descriptions include yellow spots, vellus hair, sharp, bent, broken, or zigzag hairs, dilated and tortuous blood vessels with slight extravasation of blood, a brownish-erythematous background, and perifollicular hyperkeratosis.2–5
The most common dermoscopic findings in alopecia areata include black spots, exclamation point hairs, short regrowth hairs, and yellow spots. In trichotillomania, the most common finding is broken hairs of different lengths.
Broken hairs are the result of irregular transversal fracture of the terminal hair, weakened by an inflammatory process or by the rapid growth of a hair that has not been completely destroyed. Molecular studies have made it possible to identify the bacterium Treponema pallidum in the affected follicles.6 While the pathophysiology is not clear, it is thought that the presence of T. pallidum or the immune response to this bacterium may cause vasculitis of small vessels and damage to the follicle, with a loss of terminal hair and interruption of the hair-follicle growth cycle, which results in the presence of empty follicles and broken hairs.
In this case of essential moth-eaten essential syphilitic alopecia, dermoscopy supported the suspected diagnosis (given the absence of criteria for other possible clinical diagnoses) and made it possible to speed up treatment (an antibiotic was prescribed at the time of the initial assessment). Dermoscopy is a useful, noninvasive, and rapid method that can help to diagnose a suspected syphilitic alopecia, although serological tests is essential for a definitive diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.