Reconstruction of surgical defects located close to eyelid edges, nostrils, or the mouth is challenging, as tension generated by direct closure or skin flaps in these sensitive regions tends to cause distortion. New repair techniques that prevent retraction may significantly improve outcomes.
Patients and methodsRetrospective study of the use of 2 novel flap designs-the nautilus flap and the bullfighter crutch flap-to repair surgical defects in the peripalpebral, perivestibular, nasal, and perioral areas. The nautilus flap was used to repair 4 peripalpebral defects and 2 perioral defects, and the bullfighter crutch flap to repair 14 nasal ala defects.
ResultsCosmetic and functional outcomes were very satisfactory in all 20 patients, with no cases of ectropion, nasal vestibule collapse, or labial asymmetry. Necrosis did not occur in any of the cases.
ConclusionsThe nautilus and bullfighter crutch flaps appear to be excellent choices for reconstructing surgical defects in periorificial areas.
La reconstrucción de defectos quirúrgicos en regiones anatómicas próximas a bordes palpebrales, fosas nasales o boca es un reto debido su tendencia a ser deformadas por la tensión del cierre directo o los colgajos cutáneos. El empleo de nuevas técnicas reconstructivas que eviten la retracción de estas zonas sensibles puede suponer un avance importante.
Pacientes y métodosSe emplean 2 nuevos diseños, el colgajo nautilus y el colgajo en muleta taurina, para la reconstrucción de defectos quirúrgicos periorificiales, realizando una recolección retrospectiva de los mismos en las zonas periparpebral, perivestibular nasal y peribucal. El colgajo nautilus se empleó en 4 pacientes con defectos periparpebrales y 2 peribucales. El colgajo en muleta taurina se utilizó para la reconstrucción de 14 defectos en ala nasal.
ResultadosEn los 20 pacientes se obtuvieron resultados muy satisfactorios tanto a nivel estético como funcional, sin la aparición de ectropión, colapso del vestíbulo nasal o asimetría de borde labial. No se observó necrosis en ningún caso.
ConclusionesProponemos el colgajo nautilus y el colgajo en muleta taurina como una excelente opción reconstructiva para defectos quirúrgicos localizados en zonas periorificiales.
When it is necessary to remove skin lesions located near the free edges of perioral areas, such as the eyelid margin, the nasal wing, or the perioral region itself, we face the reconstructive challenge of having to close the defect without causing deformities. A simple excision or a poorly designed flap in these areas can generate retraction forces on the free edge that lead to unaesthetic asymmetries or, even worse, functional consequences such as ectropion, mouth deformity, or collapsed nasal cavities. Traditionally, the direct closure of these areas is based on finding a vertical scar to avoid any horizontal tensions that could deform the anatomical structure. Various flaps have been used in these areas.1 On one hand, subcutaneous island flaps allow us to mobilize skin with minimal vertical tension and are widely used in the malar region, along with lateral advancements or A to T flaps. In the perioral area, advancements, sliding, transposition, or subcutaneous pedicle island flaps are often used. Finally, in the perivestibular nasal area, bilobed flaps, M-plasty, or AIRNS2 flaps are commonly used, among others.
Russo-de la Torre et al. recently published a paper3 on new skin flaps for the reconstruction of triangular surgical defects that have demonstrated to generate minimal tension at the free edge area thanks to a new experimental model that includes a digital tension meter.4 These findings encouraged us to use 2 of these flaps in patients who required closure of defects located in various perioral facial areas.
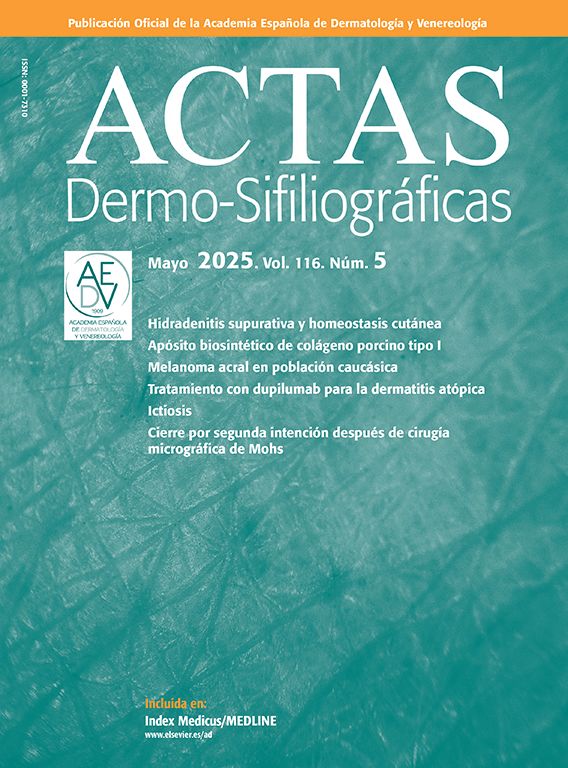
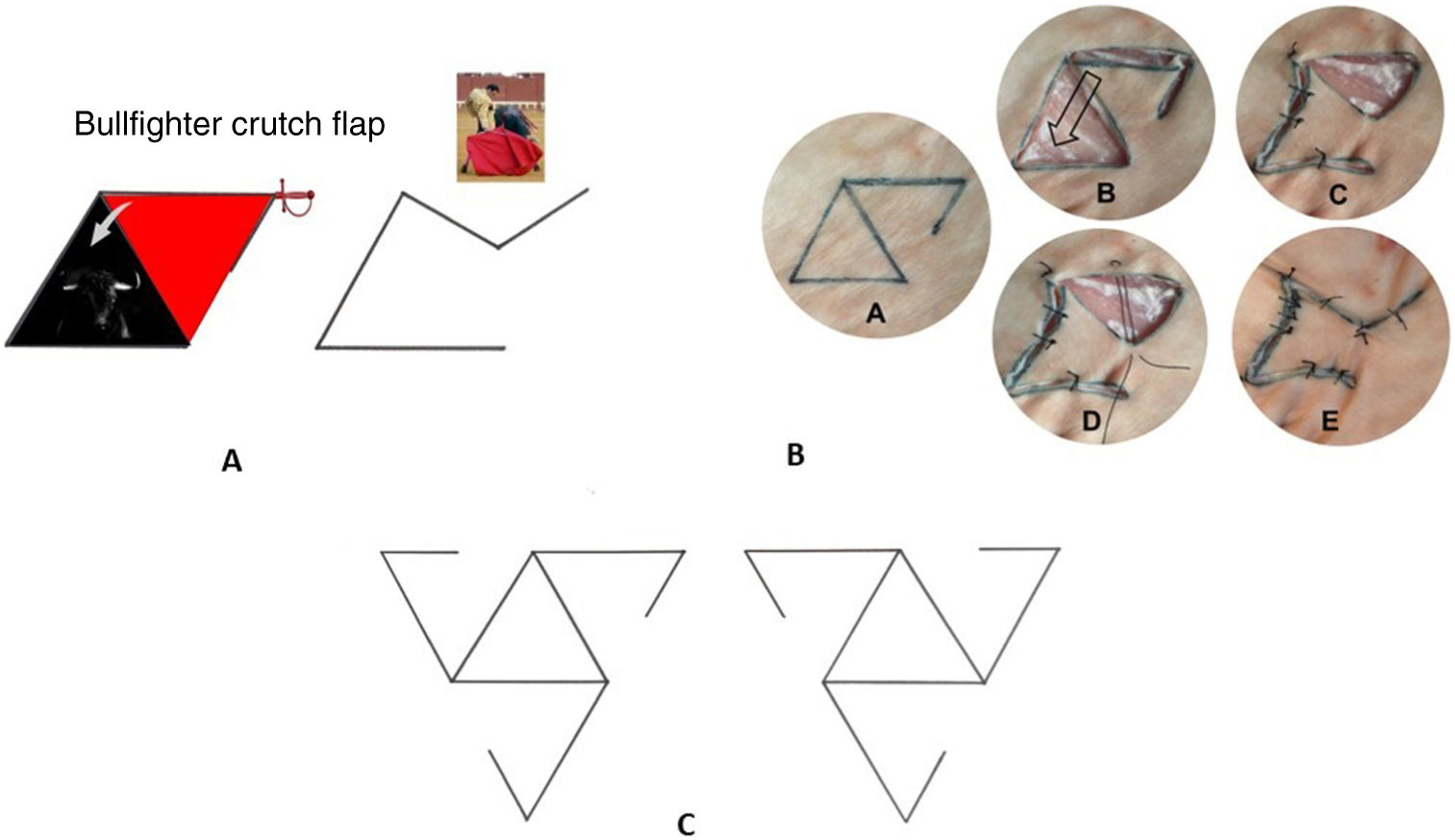
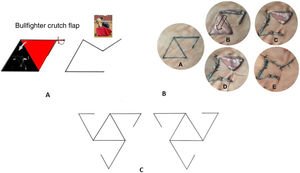
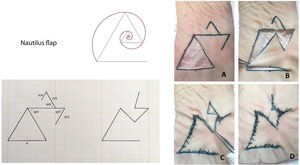
The bullfighter crutch flap is a triangular rotation flap with a very simple design. It is named after the bullfighters’ crutch (figure 1). The nautilus flap follows the same principle as the bullfighter crutch flap. However, in cases where tension prevents us from direct closure procedures of the secondary triangular defect, a second triangular rotation flap is added in the opposite direction, simulating the Fibonacci spiral or the infinite fractal of the nautilus shell (figure 2).
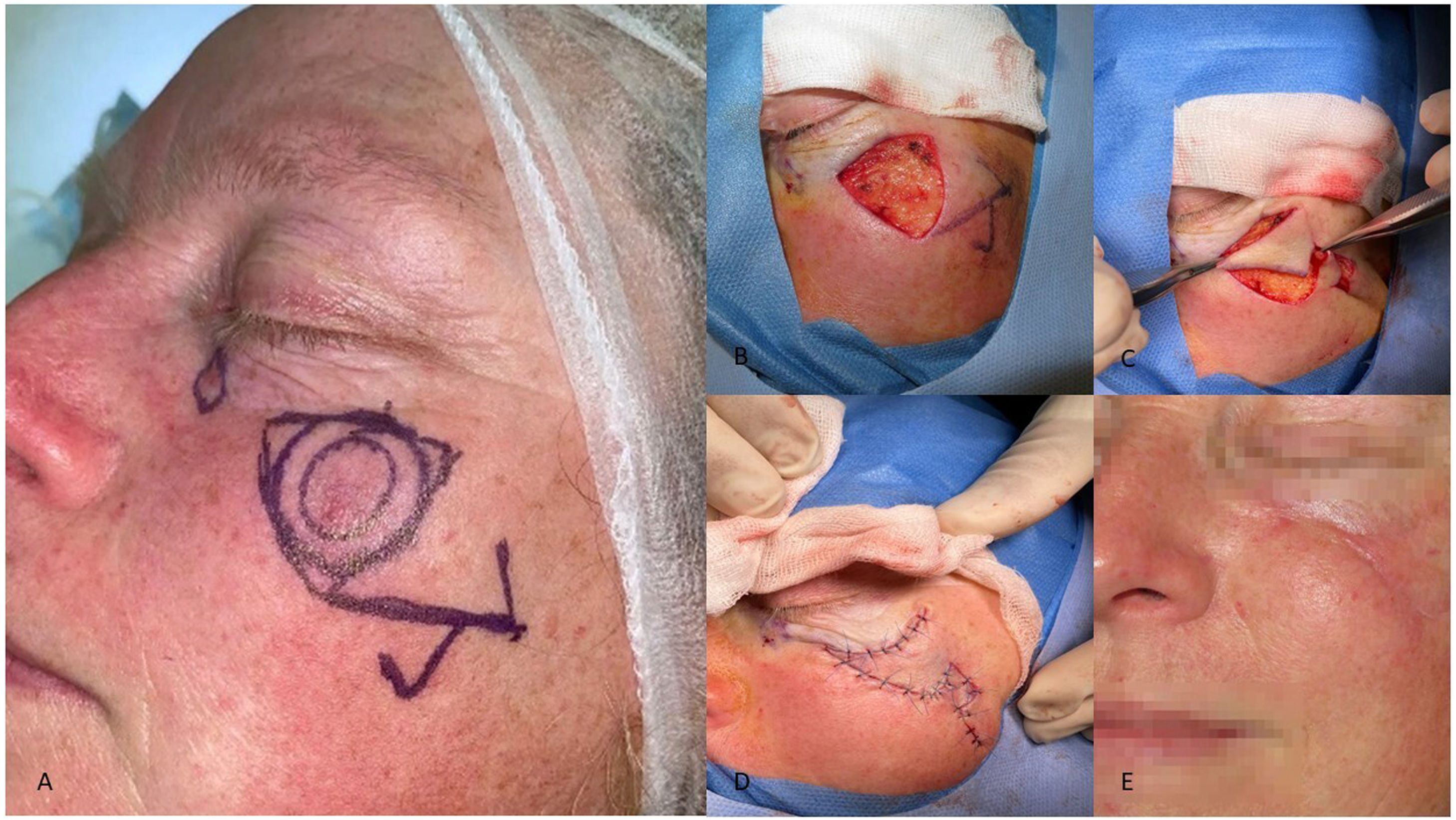
a) Bullfighter crutch flap. b)A: Flap design. On an equilateral triangle, we draw the inverted triangular flap that shares one of the sides while the other side–the pedicle–only gets halfway there. B: Excision and dissection of the flap. C: The flap is rotated to close the primary surgical defect, thus creating a smaller secondary defect. D: Angle point to close the secondary surgical defect. E: Final closure. c) The flap has 6 different design options to choose from to best suit the perioral surgical defect.
Nautilus flap: on the same design pattern of the bullfighter crutch flap, an additional upper triangle is drawn, whose sides measure half of the initial flap. This new triangle will be rotated in the opposite direction to close the secondary defect. A: Flap design on a triangular defect. B: Rotation of the flap to close the primary surgical defect. C: Closure of the secondary defect by rotating the upper triangle. E: Final closure.
This was a multicenter retrospective study that included malignant tumors of the perioral, periorbital, or perivestibular nasal regions that underwent reconstruction using the nautilus or the bullfighter crutch flap with conventional surgery with 3mm margins. Local anesthesia was used in all the cases. The tumor histopathology, disease progression, location and tumor size, follow-up time, and possible signs of recurrence were all recorded.
The surgical technique used is described below:
- 1.
An equilateral triangle is drawn including the lesion and its surgical margins plus a second inverted triangular flap that shares one of the sides in case the operator wishes to perform the bullfighter crutch flap, followed by a third triangular flap in the opposite direction if the nautilus flap is the preferred option, as mentioned earlier.
- 2.
Once the flap design has been completed, the surgical technique is started by removing the central equilateral triangle containing the defect.
- 3.
Afterwards, the flap surgical bed is detached and rotated 60 degrees to cover the entire main defect.
- 4.
Finally, the free edges are sutured, obtaining a triangular image that resembles a bullfighter's crutch or, alternatively, a nautilus shell.
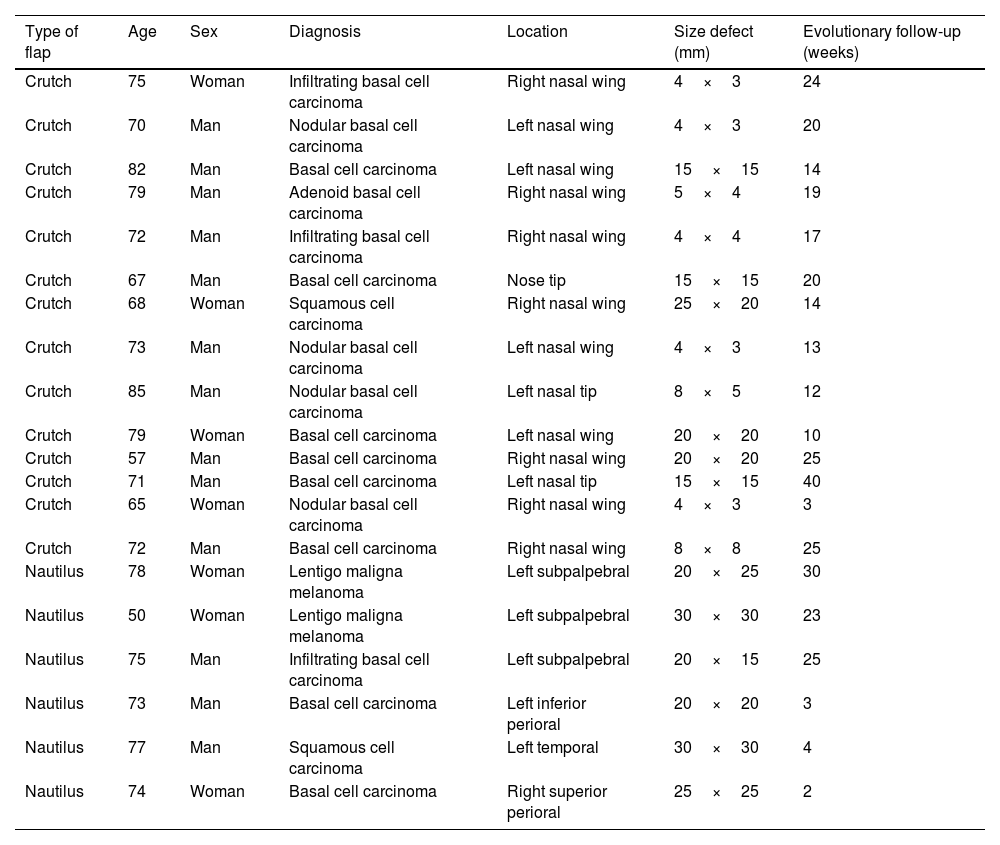
The results are shown in table 1. A total of 20 patients were included-7 women (35%) and 13 men (65%)-whose age ranges from 50 to 85 years, and a median age of 72 years.
Flaps performed, patient characteristics, tumor type, size, location, and follow-up time.
| Type of flap | Age | Sex | Diagnosis | Location | Size defect (mm) | Evolutionary follow-up (weeks) |
|---|---|---|---|---|---|---|
| Crutch | 75 | Woman | Infiltrating basal cell carcinoma | Right nasal wing | 4×3 | 24 |
| Crutch | 70 | Man | Nodular basal cell carcinoma | Left nasal wing | 4×3 | 20 |
| Crutch | 82 | Man | Basal cell carcinoma | Left nasal wing | 15×15 | 14 |
| Crutch | 79 | Man | Adenoid basal cell carcinoma | Right nasal wing | 5×4 | 19 |
| Crutch | 72 | Man | Infiltrating basal cell carcinoma | Right nasal wing | 4×4 | 17 |
| Crutch | 67 | Man | Basal cell carcinoma | Nose tip | 15×15 | 20 |
| Crutch | 68 | Woman | Squamous cell carcinoma | Right nasal wing | 25×20 | 14 |
| Crutch | 73 | Man | Nodular basal cell carcinoma | Left nasal wing | 4×3 | 13 |
| Crutch | 85 | Man | Nodular basal cell carcinoma | Left nasal tip | 8×5 | 12 |
| Crutch | 79 | Woman | Basal cell carcinoma | Left nasal wing | 20×20 | 10 |
| Crutch | 57 | Man | Basal cell carcinoma | Right nasal wing | 20×20 | 25 |
| Crutch | 71 | Man | Basal cell carcinoma | Left nasal tip | 15×15 | 40 |
| Crutch | 65 | Woman | Nodular basal cell carcinoma | Right nasal wing | 4×3 | 3 |
| Crutch | 72 | Man | Basal cell carcinoma | Right nasal wing | 8×8 | 25 |
| Nautilus | 78 | Woman | Lentigo maligna melanoma | Left subpalpebral | 20×25 | 30 |
| Nautilus | 50 | Woman | Lentigo maligna melanoma | Left subpalpebral | 30×30 | 23 |
| Nautilus | 75 | Man | Infiltrating basal cell carcinoma | Left subpalpebral | 20×15 | 25 |
| Nautilus | 73 | Man | Basal cell carcinoma | Left inferior perioral | 20×20 | 3 |
| Nautilus | 77 | Man | Squamous cell carcinoma | Left temporal | 30×30 | 4 |
| Nautilus | 74 | Woman | Basal cell carcinoma | Right superior perioral | 25×25 | 2 |
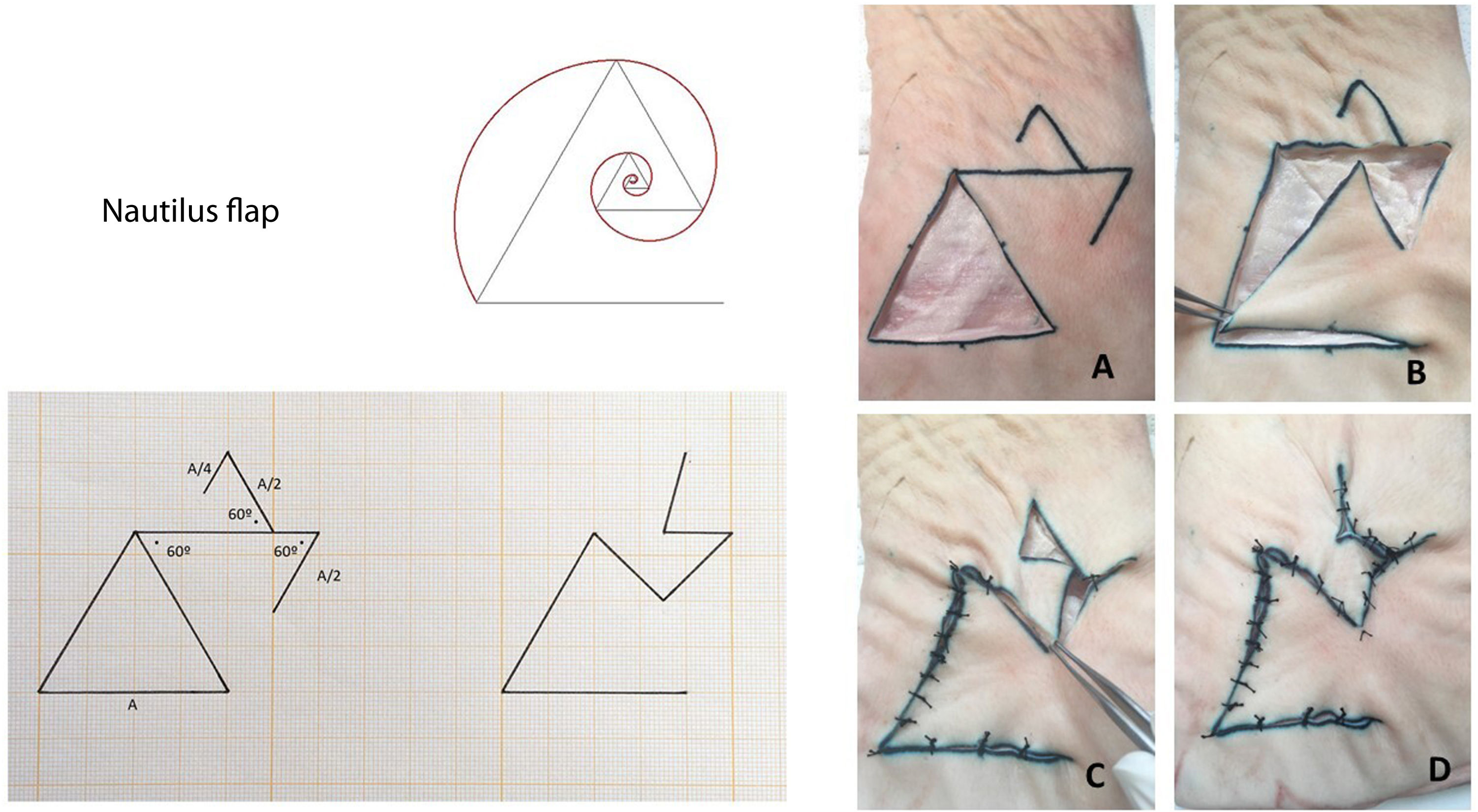
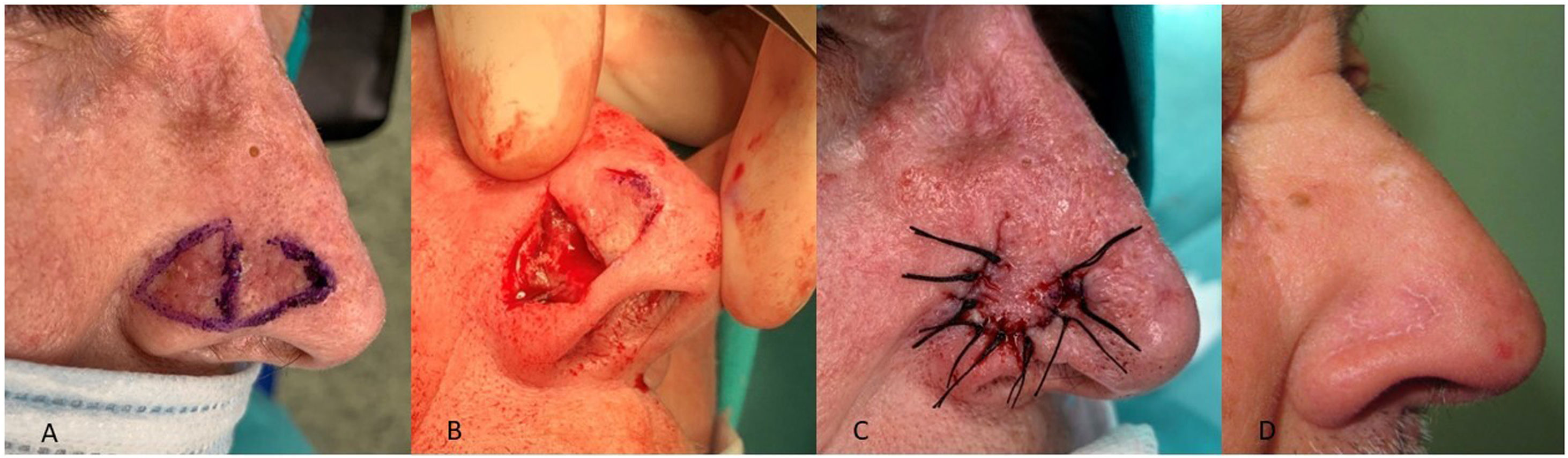
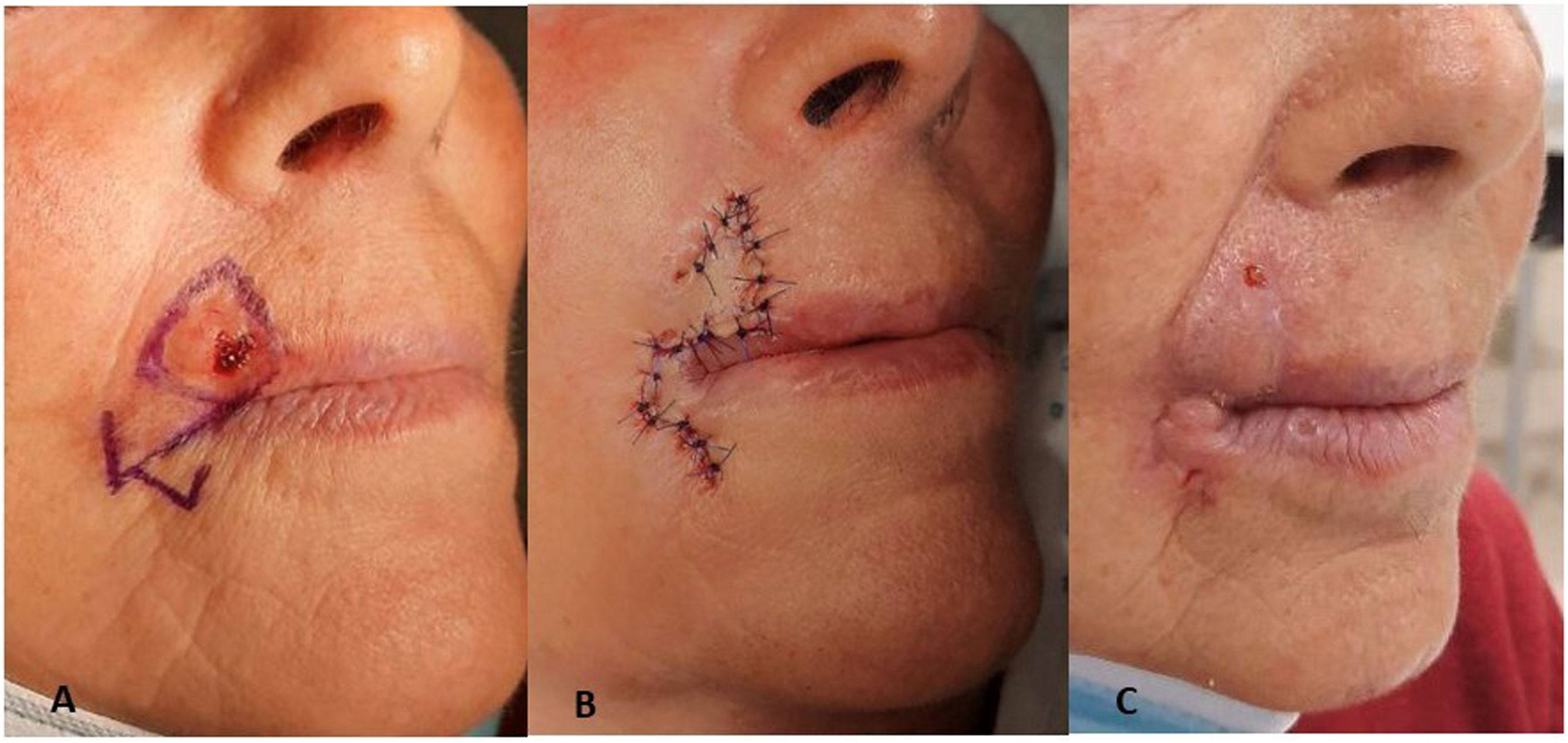
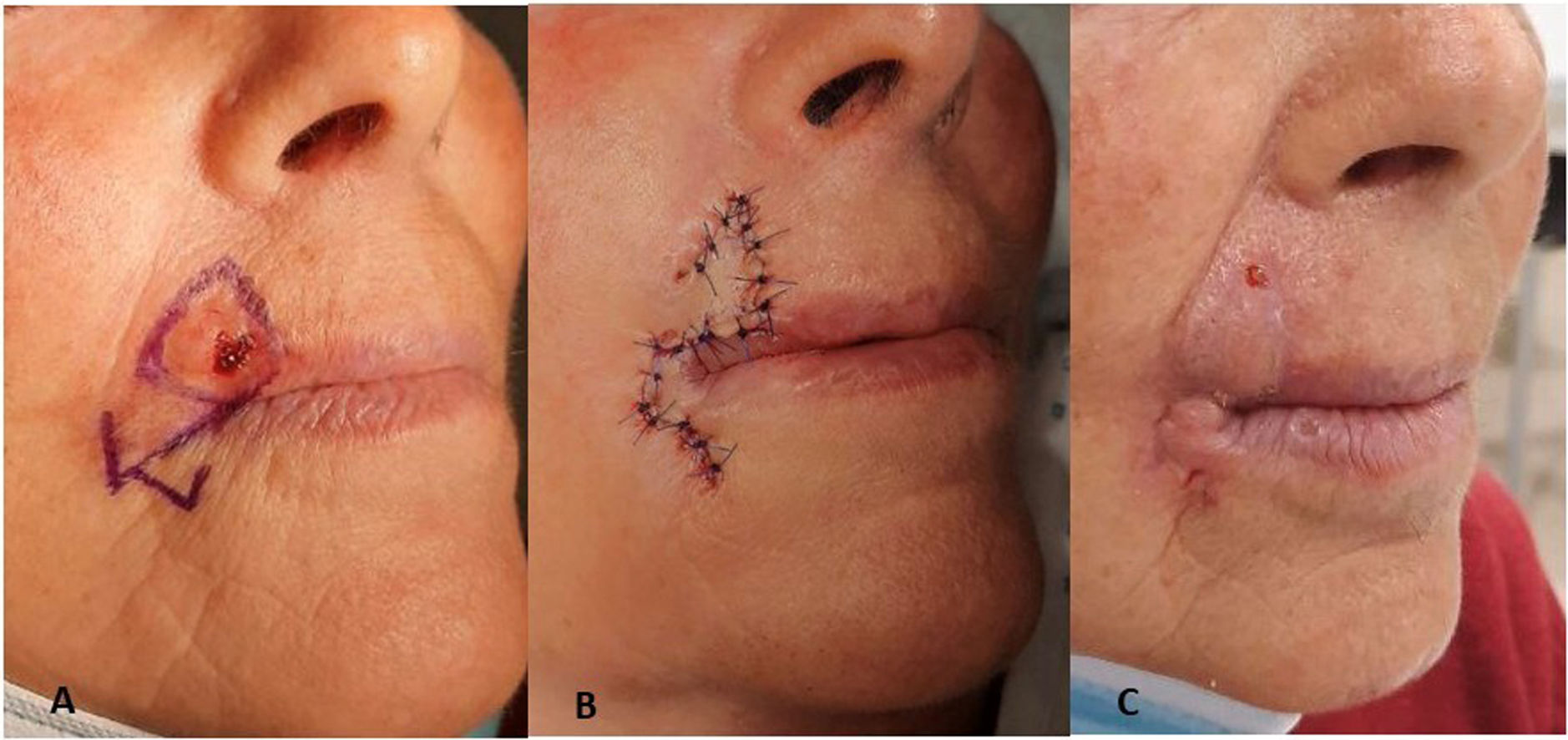
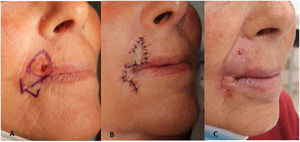
The primary lesion excised was basal cell carcinoma in 80% of the patients (16 in total), predominantly the nodular subtype, followed by squamous cell carcinoma and lentigo maligna melanoma, each accounting for 10% of the cases reported. The largest diameter of the defects ranged from 4mm to 30mm with a mean of 14.8mm, areas between 0.12 cm2 and 9 cm2, and a mean area of 2.66 cm2. The bullfighter crutch flap was used to reconstruct 14 defects in the nasal wing (figure 3), and the nautilus flap to repair 4 palpebral and 2 perioral defects (Figures 4 and 5). There was no margin involvement reported in any of the excised tumors. Regarding complications, 1 patient developed an area of perioral hypertrophic scarring that required intralesional corticosteroid injections, with a good response and no functional repercussions. No cases of dehiscence or necrosis were seen.
Design, performance, and postoperative outcomes of the nautilus flap on a left subpalpebral lesion, along with a simple spindle design for another smaller lesion medial to it. A: Flap design. B: Lesion excision creating a triangular surgical defect. C: Rotation of the 2 triangular flaps in opposite directions. D: Final suturing of the flaps. E: Final outcomes at the 3-month follow-up.
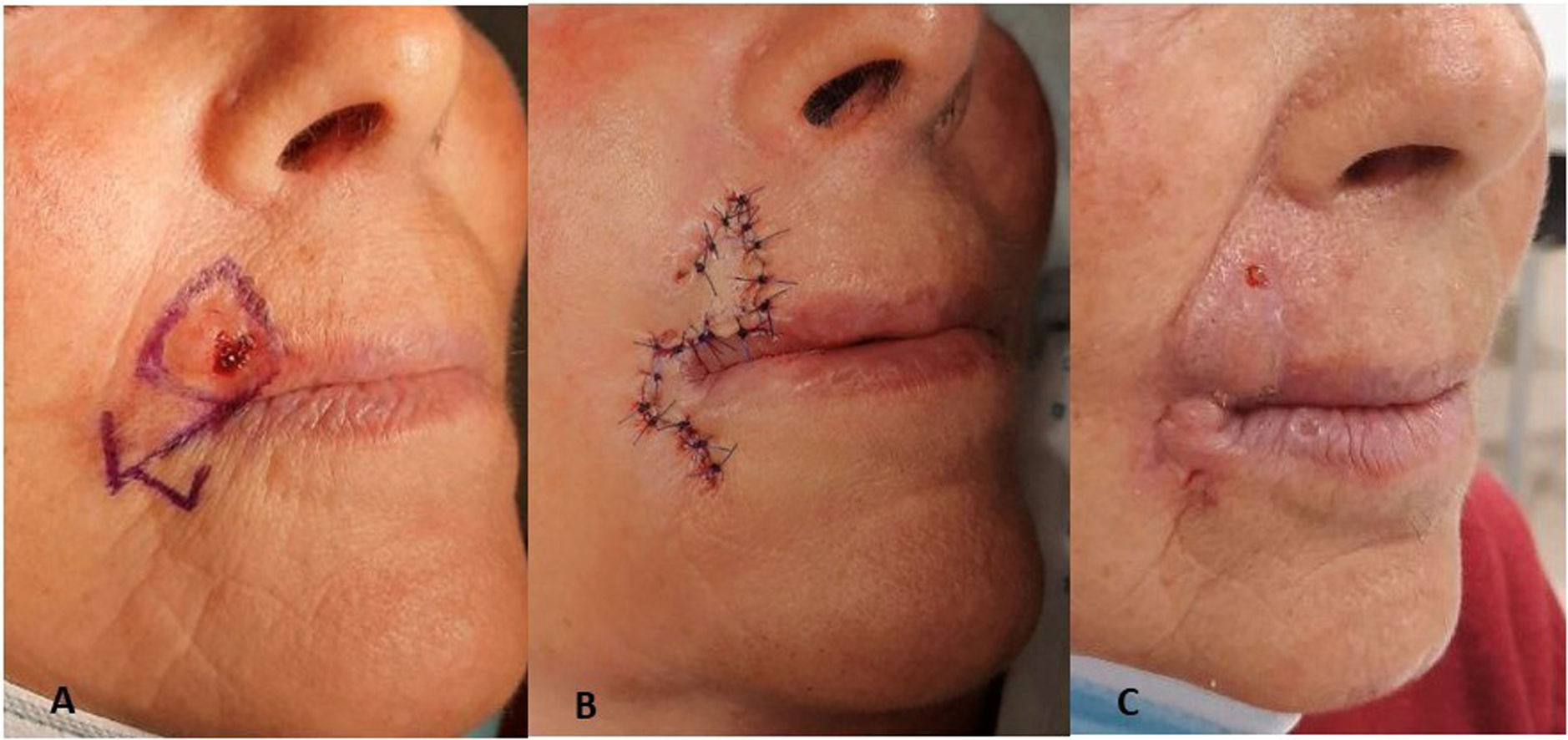
Nautilus flap used in the reconstruction of a surgical defect on the upper lip after the removal of an infiltrating basal cell carcinoma. A: Flap design turning the circular defect into a triangular one. B: Immediate postoperative, suture with prolene 4.0. C: Aesthetic result after suture removal. The morphology of the tumor requires designing the triangle with the base facing the free edge of the upper lip. However, the direction of the tension vector is the same, which is why it does not pull from the free edge. In this case, maximum tension is perpendicular to the free edge, which is right one to prevent retraction. Therefore, the resulting scar from the flap suture perfectly fits the patient's perioral region without ever distorting it.
None of the patients experienced any recurrences of the excised lesions with a median follow-up time of 18 weeks (range, 2 to 40 weeks).
DiscussionThe reconstruction of facial skin defects in areas next to orifices is surgically challenging. In these areas, performing certain flaps can be a complicated task to perform due to the possibility of causing functional defects such as ectropion, notches, or microstomia. Bullfighter crutch or nautilus flaps are an interesting alternative in these situations because they limit the tensions generated near the orifice. The use of these types of flaps is not limited to triangular defects since a circular or an irregular defect can easily be converted into a triangle, while still sparing the surgical margins. One could argue that, a priori, a triangular excision involves sacrificing healthy tissue at the vertices of the triangle, but the truth is that the flap's design perfectly aligns with the vertices when performed accurately. Similarly, several authors have mentioned that triangulating surgical defects reduces the trapdoor effect.
Excessive tension in a flap has been described as a factor causing ischemia potentially leading to total or partial necrosis of the flap. In this regard, an experimental model demonstrated that triangular flaps achieve closure with minimal tension being generated.4
Although this flap has a simple rectilinear geometry that facilitates its design, performing the bullfighter crutch or the nautilus flaps takes manual dexterity, and knowledge of dermatological surgery. The key to these flaps lies in their design, making sure that the free edge always remains at the base of the equilateral triangle, which is the area where the least tension will be generated. During the surgical act, we should avoid leaving a narrow pedicle that could compromise the viability of the flap since these are free flaps. We should mention that no total or partial necrosis was reported in any of the patients, indicating a high flap viability.
ConclusionsBoth the nautilus flap and the bullfighter crutch flap are excellent reconstructive options to treat surgical defects located in perioral areas. These techniques are easy to use, and with the proper design, reduce the tension associated with the free edge of the nasal wing, eyelid margin, or lip edge. It is not necessary to dissect too much tissue either. Both flaps are good alternatives in the management of closing defects in these anatomical regions.
FundingNone declared.
Conflicts of interestNone whatsoever.