Although psoriasis is a chronic and systemic inflammatory disease characterized by a bimodal incidence, it can manifest at any age.1 Literature on the behavior of this disease in the elderly is scarce, despite the significant frequency of cases in this age range. While plaque psoriasis is the most common clinical sign overall, and particularly in older age,2 pustular forms of psoriasis in the elderly—excluding palmoplantar pustulosis (PPP)—have been poorly characterized.1,3,4
We conducted a retrospective, observational study with patients older than 65 years with a diagnosis of late-onset pustular psoriasis (PP)—onset after the age of 50—with a > 4-week history of generalized pustulosis without associated palmoplantar pustulosis, who had already been seen and/or were being followed in the psoriasis clinic at Hospital General Universitario Gregorio Marañón, Madrid, Spain from January 2000 through December 2021. Clinical, analytical, therapeutic, and evolutionary data were obtained from the electronic health records of the department.
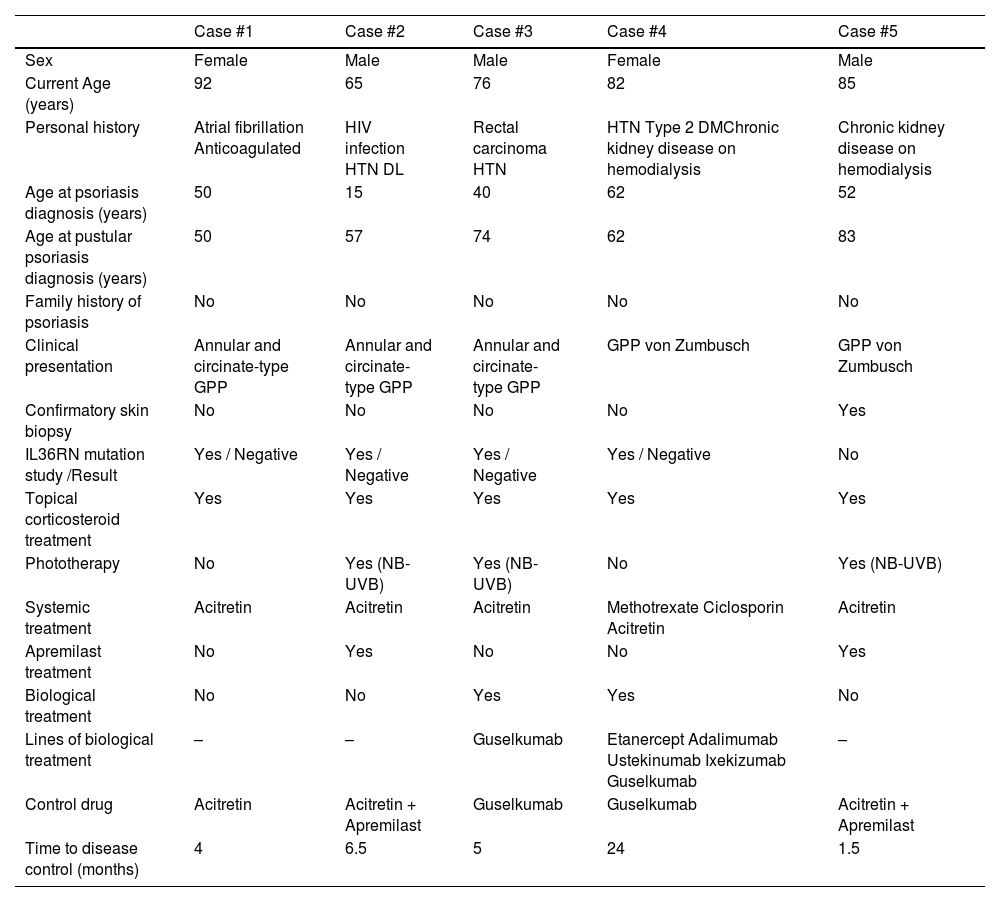
A total of 5 patients were included (Table 1), 3 of whom were male (60%). These 3 patients exihibited plaque psoriasis lesions before the onset of pustular signs; the time from the diagnosis of plaque psoriasis to the development of generalized pustular forms was 31, 34, and 42 years, respectively. The 2 women had no personal or family history of psoriasis or other dermatological diseases. The age at diagnosis of pustular forms went from 50 up to 83 years (Table 1).
Characteristics of the patients included in the series.
| Case #1 | Case #2 | Case #3 | Case #4 | Case #5 | |
|---|---|---|---|---|---|
| Sex | Female | Male | Male | Female | Male |
| Current Age (years) | 92 | 65 | 76 | 82 | 85 |
| Personal history | Atrial fibrillation Anticoagulated | HIV infection HTN DL | Rectal carcinoma HTN | HTN Type 2 DMChronic kidney disease on hemodialysis | Chronic kidney disease on hemodialysis |
| Age at psoriasis diagnosis (years) | 50 | 15 | 40 | 62 | 52 |
| Age at pustular psoriasis diagnosis (years) | 50 | 57 | 74 | 62 | 83 |
| Family history of psoriasis | No | No | No | No | No |
| Clinical presentation | Annular and circinate-type GPP | Annular and circinate-type GPP | Annular and circinate-type GPP | GPP von Zumbusch | GPP von Zumbusch |
| Confirmatory skin biopsy | No | No | No | No | Yes |
| IL36RN mutation study /Result | Yes / Negative | Yes / Negative | Yes / Negative | Yes / Negative | No |
| Topical corticosteroid treatment | Yes | Yes | Yes | Yes | Yes |
| Phototherapy | No | Yes (NB-UVB) | Yes (NB-UVB) | No | Yes (NB-UVB) |
| Systemic treatment | Acitretin | Acitretin | Acitretin | Methotrexate Ciclosporin Acitretin | Acitretin |
| Apremilast treatment | No | Yes | No | No | Yes |
| Biological treatment | No | No | Yes | Yes | No |
| Lines of biological treatment | – | – | Guselkumab | Etanercept Adalimumab Ustekinumab Ixekizumab Guselkumab | – |
| Control drug | Acitretin | Acitretin + Apremilast | Guselkumab | Guselkumab | Acitretin + Apremilast |
| Time to disease control (months) | 4 | 6.5 | 5 | 24 | 1.5 |
DL: dyslipidemia; DM: diabetes mellitus; HTN: hypertension; IL36RN: IL36 receptor antagonist; GPP: generalized pustular psoriasis; NB-UVB: narrowband ultraviolet B; HIV: human immunodeficiency virus.
In 4 cases, the mutational status of the IL36 receptor antagonist gene (IL36RN) was analyzed, but no pathological variants were found in any of these cases.
All patients required hospitalization at some point during the course of their PP, with 2 cases requiring hospitalization at the onset of the pustular form due to fever and systemic symptoms (generalized pustular psoriasis [GPP] von Zumbusch).
The 5 patients in the series received topical corticosteroids and acitretin as first-line systemic therapy—usual therapeutic doses, 10 to 25mg/day—which was sufficient to control the skin symptoms in only 1 case. The combination with apremilast was the control treatment in 2 patients, and in the remaining cases, biological treatment with guselkumab was used.
Compared with series on vulgar psoriasis, studies on the epidemiological and clinical-evolutionary characteristics of patients with PP are scarce,5–10 and even more so when talking about patients older than 60-65 years, with only 1 series specifically addressing this patient subgroup.5
The diagnosis of pustular forms of psoriasis is usually established around the 4th decade of life,6 forms in which mutations associated with PP are more prevalent.7–9
In the series of 7 cases of GPP in patients older than 60 years—mean age 70.7 ± 9.2 years—5 no patients had a personal or family history of psoriasis, and the genetic study turned out negative in 6 of the 7 cases analyzed. Compared with a series of 32 patients with GPP without age differentiation, older patients had a greater tendency towards erythroderma.5,7–9
Although rare, PP is a disease that, especially in its GPP form, can become severe, leading to patient death and frequently requiring hospitalization.8–10 In our setting, the need for intensive care unit admission is estimated at 6.1%, with a mortality rate of 4.8% for GPP patients overall, without considering age ranges.10 In our series, all patients required hospitalization at some point during the course of the disease. Two out of the 7 patients from the above-mentioned series5 required hospitalization.
Regarding treatment, elderly patients, per se, are a more fragile population,1 with more comorbidities1,4 and, considering the potential severity of the disease, all this can complicate therapeutic management.2,3 That is why the use of biological drugs in the management of GPP is on the rise.6,8,9 Similarly, although in our series of 7 elderly patients with GPP,5 acitretin was the first-line therapy, 3 required biological therapies.
PP can be a late-onset condition, especially in patients without prior plaque psoriasis,5,8 requiring systemic treatment for its control.9 It can manifest severely with systemic involvement10 and does not necessarily carry mutations in IL36RN,5–7 especially when it in the elderly.7–9 Despite the typical immunosenescence of these patients, these cases can be resistant to therapy and may require biological therapy to achieve remission of lesions and control of psoriasis.8
FundingNone declared.
Authors’ contributionsAll authors contributed to the drafting of this work, and agreed on the publication of this article.
Conflicts of interestNone declared.