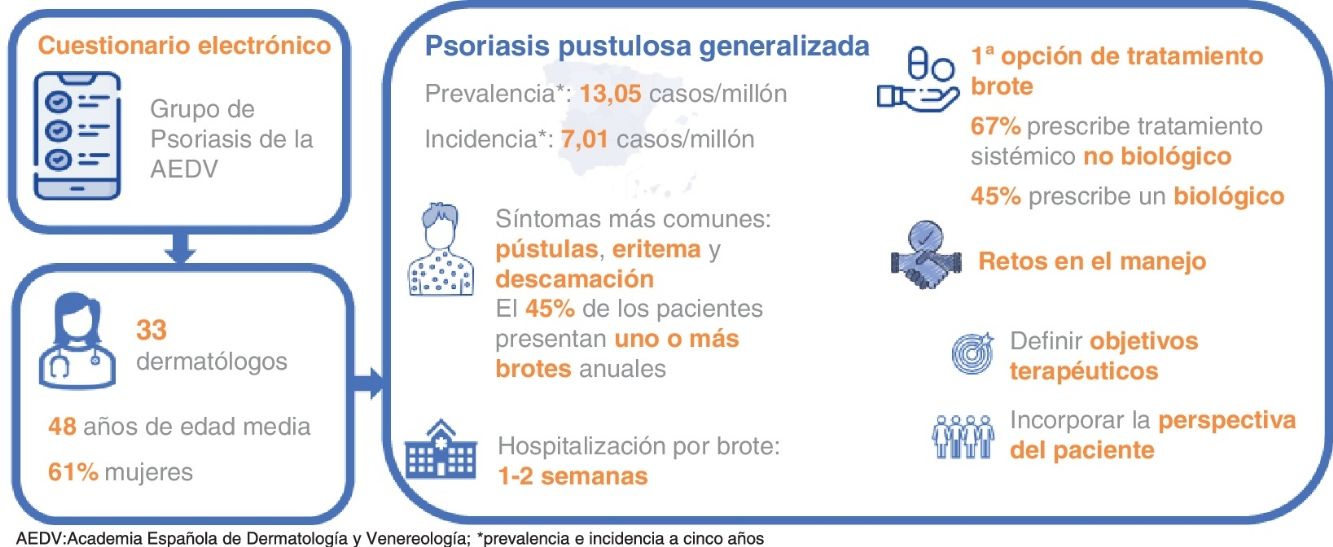
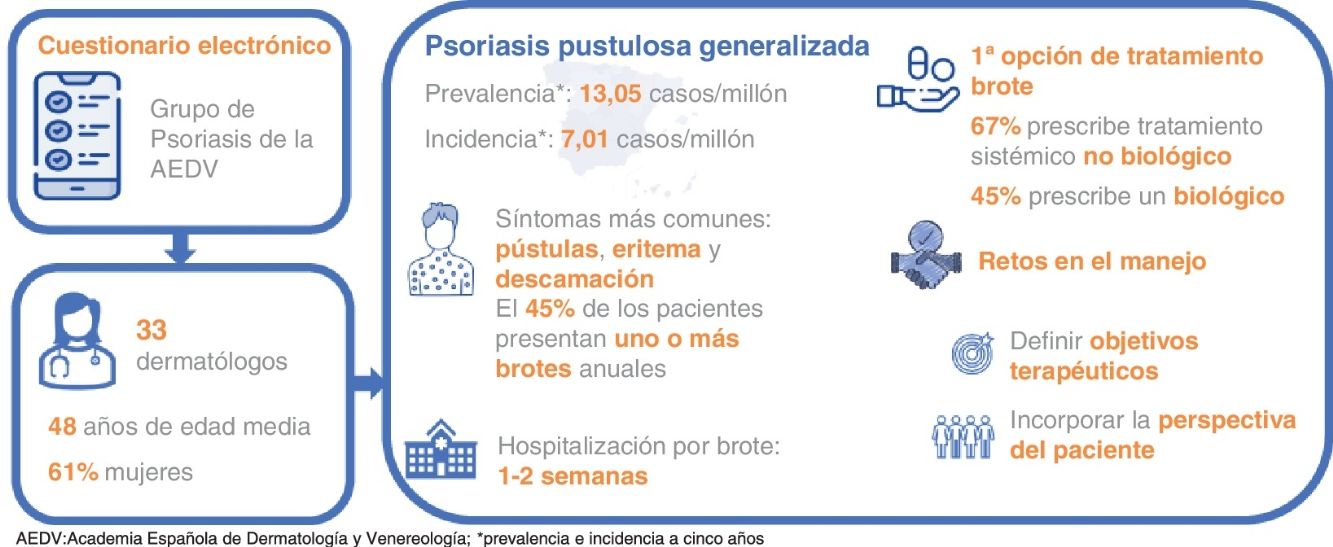
Generalized pustular psoriasis (GPP) is a rare and severe inflammatory skin disease characterised by recurrent or intermittent flares. Epidemiological and disease management data in Spain are limited. Our goal was to estimate the epidemiology of GPP, explore its management, and reach consensus on the current challenges faced in Spain.
MethodsAn electronic survey was submitted to dermatologists from the Spanish Academy of Dermatology and Venereology Psoriasis Working Group. This group is experienced in the management of GPP. It included a Delphi consensus to establish the current challenges.
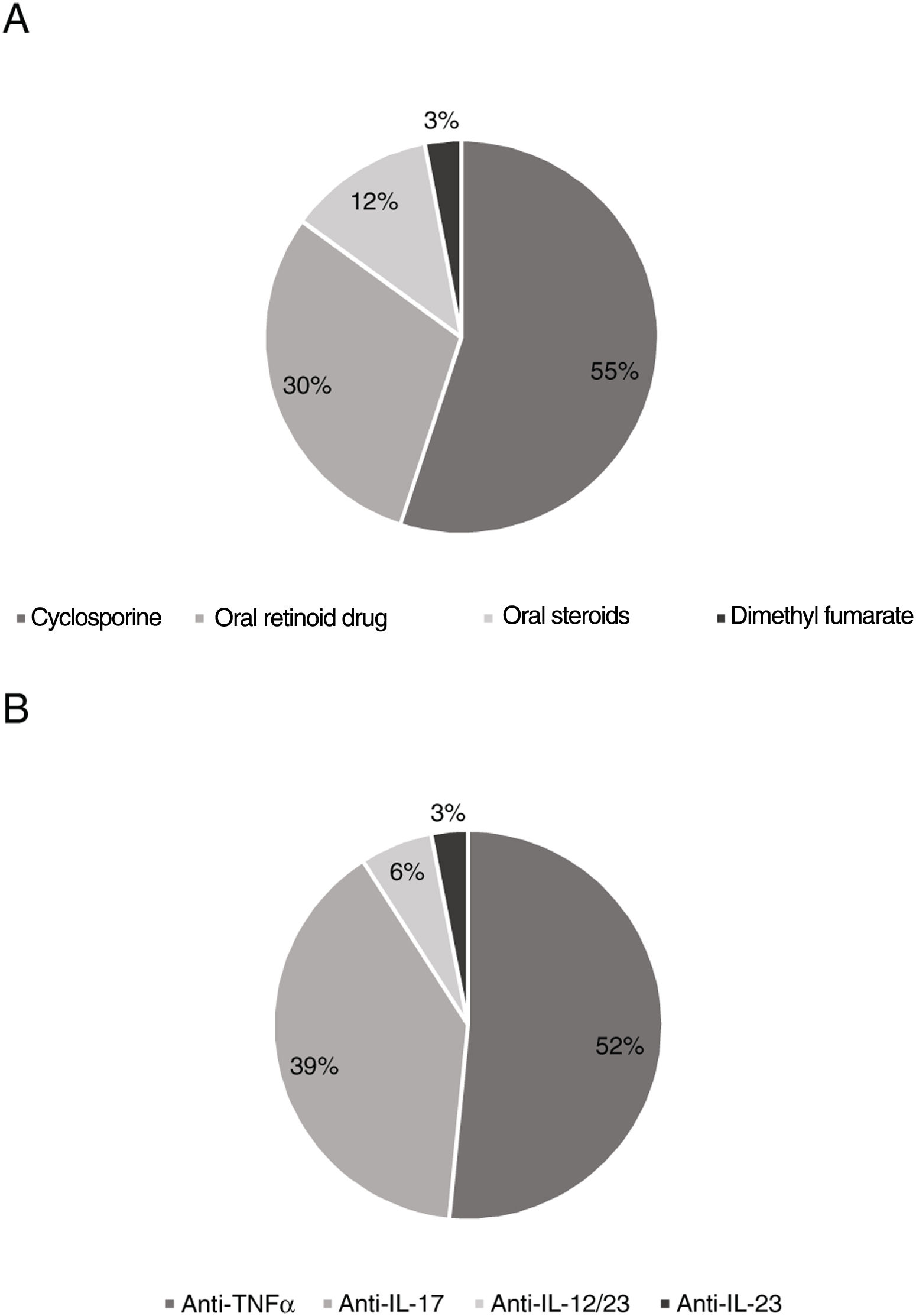
ResultsA total of 33 dermatologists responded to the survey. A 5-year prevalence and incidence of 13.05 and 7.01 cases per million inhabitants, respectively, were estimated. According to respondents, the most common GPP symptoms are pustules, erythema, and desquamation, while 45% of patients present > 1 annual flares. A total of 45% of respondents indicated that flares often require a length of stay between 1 and 2 weeks. In the presence of a flare, 67% of respondents often or always prescribe a non-biological systemic treatment as the first-line therapy [cyclosporine (55%); oral retinoid (30%)], and 45% a biological treatment [anti-TNFα (52%); anti-IL-17 (39%)]. The dermatologists agreed that the main challenges are to define and establish specific therapeutic goals to treat the disease including the patients’ perspective on the management of the disease.
ConclusionOur study describes the current situation on the management of GPP in Spain, increasing the present knowledge on the disease, and highlighting the current challenges faced at the moment.
La psoriasis pustulosa generalizada (PPG) es una enfermedad rara e inflamatoria grave de la piel que cursa con brotes recurrentes o intermitentes. Los datos epidemiológicos y sobre su manejo en España son limitados. Nuestro objetivo fue estimar la epidemiologia de la PPG, explorar su manejo y consensuar los retos actuales en España.
MétodosCuestionario electrónico dirigido a los dermatólogos del Grupo de Psoriasis de la Academia Española de Dermatología y Venereología con experiencia en el manejo de la PPG, que incluía un consenso Delphi para establecer los retos actuales.
ResultadosTreinta y tres dermatólogos respondieron al cuestionario. Se estimó una prevalencia e incidencia a 5 años de 13,05 y 7,01 casos por millón de habitantes, respectivamente. Según los dermatólogos, los síntomas de la PPG más comunes son las pústulas, el eritema y la descamación, y el 45% de los pacientes presentan uno o más brotes anuales. El 45% indicó que es muy común que un brote requiera hospitalización y dure 1-2 semanas. Ante un brote, el 67% prescribe a menudo o siempre como primera opción un tratamiento sistémico no biológico (ciclosporina [55%]; retinoide oral [30%]) y el 45% un biológico (anti-TNFα [52%]; anti-IL-17 [39%]). Se consensuaron como principales retos la necesidad de definir y establecer objetivos terapéuticos específicos de la enfermedad e incorporar la perspectiva del paciente en el manejo de la enfermedad.
ConclusionesNuestro estudio describe la situación actual de la PPG en España, y amplía el conocimiento sobre la enfermedad, poniendo de manifiesto los retos actuales en su manejo.
Generalized pustular psoriasis (GPP) is a severe inflammatory skin disease characterized by the sudden and widespread eruption of superficial sterile pustules,1 high fever, asthenia, and leukocytosis.2,3
GPP is a rare disease, with limited data on its prevalence. Nevertheless, it appears to be more common in Asian than Caucasian populations, more prevalent in women,1 and often appear in the adult population aged 40 to 50 years.1
The course of the disease is heterogeneous, with recurrent or intermittent flare-ups,4 which along with the lack of standardized international guideline criteria, poses a challenge4 as both the early diagnosis and treatment of the disease are crucial for preventing the potential morbidity and mortality associated with GPP.5-7
The main objective of our study was to estimate the epidemiological data of GPP, describe its management including patient characteristics, diagnosis, clinical course, and disease burden, and identify the possible challenges we currently face in Spain.
MethodsThe study was conducted using an electronic questionnaire (for its efficiency in distribution and completion) sent to dermatologists from the Psoriasis Working Group of the Spanish Academy of Dermatology and Venereology (AEDV) with experience in managing GPP (they had seen, at least, 1 patient with GPP over the past 5 years).
Guidance to design and develop the study was provided by a scientific committee including 6 dermatologists experienced in the management of GPP (JMC, GC, PC, NE, RR, and EV). The questionnaire collected information on sociodemographic and health care variables of each dermatologist, epidemiological data of GPP over the past 5 years, characteristics, signs and symptoms of patients with GPP, diagnosis and assessment of GPP, natural course of the disease (flare-ups and systemic complications), burden, disease management, and challenges in its management.
The definition of GPP provided to dermatologists was proposed by the European Rare and Severe Psoriasis Expert Network (ERASPEN): the appearance of primary, sterile, and macroscopically visible pustules on non-acral skin (excluding cases in which pustulation is limited to psoriatic plaques), which may occur with or without systemic inflammation, with or without psoriasis, and which may be a recurring (> 1 episode) or persistent (> 3 months) disease.8
To reach consensus on the current challenges faced in the management of GPP, 2 rounds of Delphi consultation were conducted, exploring the level of agreement (7-point Likert scale) on 7 statements. Consensus was established if 75% of participants agreed (6,7) or disagreed (1,2) on each statement. Additionally, a prioritization exercise was included on current needs in the development of new treatments for GPP.
Data analysisMeasures of central tendency and dispersion (mean, standard deviation [SD], and number of observations) were calculated for quantitative variables, and relative and absolute frequencies for qualitative variables. Analyses were performed with the total valid data for each question.
The prevalence and mean 5-year incidence were estimated based on the reference areas of the hospitals that reported treating patients with GPP during this period.
Statistical analysis was performed using STATA® v.14 software.
ResultsCharacteristics of participant dermatologistsThe survey was sent to 180 dermatologists who were members of the Psoriasis Working Group (PGW), 38 of whom (21%) contributed to the study. Thirty-three (18%) out of these 38 dermatologists from 28 Spanish hospitals had treated, at least, 1 patient with GPP in the past 5 years and, therefore, were eligible to participate in the study.
The mean age (SD) of participants was 48 (10.1) years, 61% were women, with a mean experience (SD) in their specialty of 18.9 (10.4) years.
EpidemiologyThe 5-year prevalence of GPP was estimated from 106 patients treated in 25 centers during this period, which resulted in a total of 13.05 cases per million inhabitants. The 5-year incidence rate was estimated from 57 patients treated in 23 centers who reported experiencing a flare-up for the first time, resulting in 7.01 cases per million inhabitants (supplementary table 1).
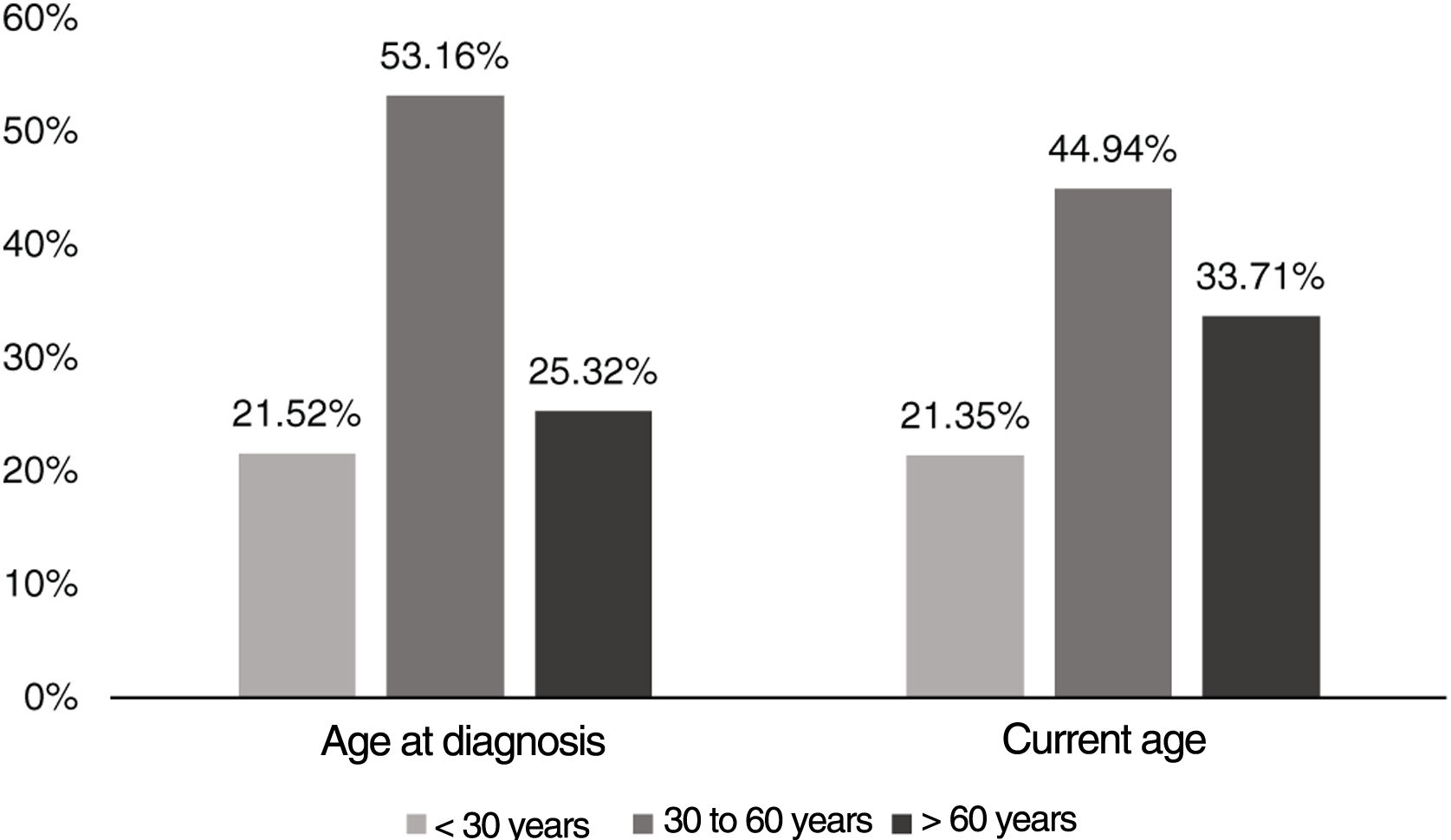
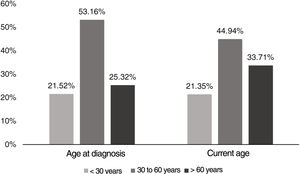
Characteristics of the patientsA total of 45% of the patients with GPP treated by the participant dermatologists were between 30 and 60 years-old, and 57% were women (figure 1).
Dermatologists indicated that 35% of the patients with GPP had a family history of other forms of psoriasis, 12% had psoriatic arthritis, and 4% had GPP. Additionally, 46% of the patients with GPP had plaque psoriasis, while 15% had psoriatic arthritis.
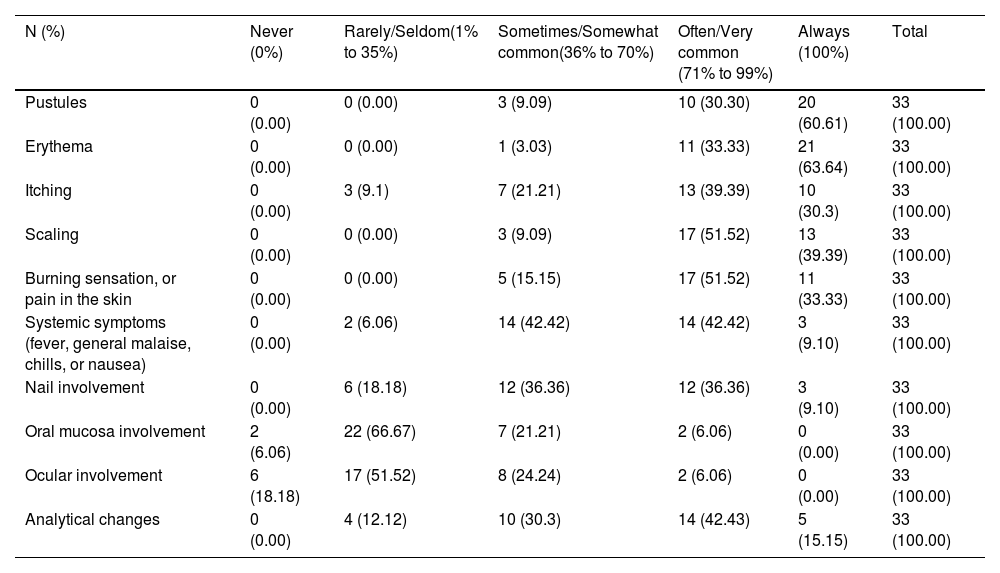
Signs and symptoms of the diseaseAccording to most dermatologists, pustules (91%), erythema (97%), itching (70%), scaling (91%), burning or pain sensation on the skin (85%), and laboratory abnormalities (58%) usually or always appear in patients with GPP. In contrast, most specialists (73% and 70%) believed that oral and ocular mucosal involvement rarely or never occur. Systemic symptoms occur somewhat commonly (42%) or very commonly (42%) (table 1).
Frequency of signs and symptoms in patients with GPP.
| N (%) | Never (0%) | Rarely/Seldom(1% to 35%) | Sometimes/Somewhat common(36% to 70%) | Often/Very common (71% to 99%) | Always (100%) | Total |
|---|---|---|---|---|---|---|
| Pustules | 0 (0.00) | 0 (0.00) | 3 (9.09) | 10 (30.30) | 20 (60.61) | 33 (100.00) |
| Erythema | 0 (0.00) | 0 (0.00) | 1 (3.03) | 11 (33.33) | 21 (63.64) | 33 (100.00) |
| Itching | 0 (0.00) | 3 (9.1) | 7 (21.21) | 13 (39.39) | 10 (30.3) | 33 (100.00) |
| Scaling | 0 (0.00) | 0 (0.00) | 3 (9.09) | 17 (51.52) | 13 (39.39) | 33 (100.00) |
| Burning sensation, or pain in the skin | 0 (0.00) | 0 (0.00) | 5 (15.15) | 17 (51.52) | 11 (33.33) | 33 (100.00) |
| Systemic symptoms (fever, general malaise, chills, or nausea) | 0 (0.00) | 2 (6.06) | 14 (42.42) | 14 (42.42) | 3 (9.10) | 33 (100.00) |
| Nail involvement | 0 (0.00) | 6 (18.18) | 12 (36.36) | 12 (36.36) | 3 (9.10) | 33 (100.00) |
| Oral mucosa involvement | 2 (6.06) | 22 (66.67) | 7 (21.21) | 2 (6.06) | 0 (0.00) | 33 (100.00) |
| Ocular involvement | 6 (18.18) | 17 (51.52) | 8 (24.24) | 2 (6.06) | 0 (0.00) | 33 (100.00) |
| Analytical changes | 0 (0.00) | 4 (12.12) | 10 (30.3) | 14 (42.43) | 5 (15.15) | 33 (100.00) |
GPP, generalized pustular psoriasis.
The most common referral pathway for patients with GPP to dermatology clinics is through the ER (97%), followed by primary care (39%) and other specialists (33%), 33% of whom came from dermatology, 33% from internal medicine, and 25% from rheumatology.
A total of 90.9% of respondents considered it important to perform a biopsy to confirm the diagnosis of GPP.
To assess disease severity, the most widely used tool is the Body Surface Area (94%), followed by the Physician Global Assessment (79%) and the Dermatology Life Quality Index (67%) (supplementary table 2).
Natural course of the diseaseInformation on the number of annual flare-ups (defined as any sign of the disease requiring dermatologist consultation) was available for 76 patients. Of these, 55.3% experienced < 1 flare-up per year, while 31.6% and 13.2% experienced 1 to 2 flare-ups per year and > 2 flare-ups per year, respectively.
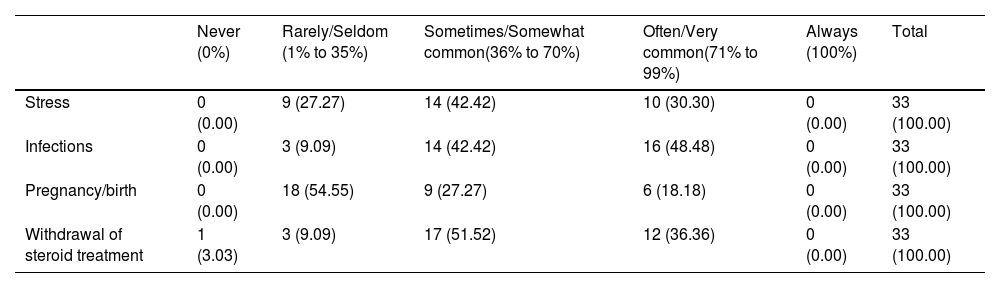
A total of 55% of dermatologists considered that the trigger of a flare-up can sometimes be identified, being infections a very common triggering factor, followed by steroid withdrawal and stress (table 2).
Frequency of factors capable of triggering an outbreak.
| Never (0%) | Rarely/Seldom (1% to 35%) | Sometimes/Somewhat common(36% to 70%) | Often/Very common(71% to 99%) | Always (100%) | Total | |
|---|---|---|---|---|---|---|
| Stress | 0 (0.00) | 9 (27.27) | 14 (42.42) | 10 (30.30) | 0 (0.00) | 33 (100.00) |
| Infections | 0 (0.00) | 3 (9.09) | 14 (42.42) | 16 (48.48) | 0 (0.00) | 33 (100.00) |
| Pregnancy/birth | 0 (0.00) | 18 (54.55) | 9 (27.27) | 6 (18.18) | 0 (0.00) | 33 (100.00) |
| Withdrawal of steroid treatment | 1 (3.03) | 3 (9.09) | 17 (51.52) | 12 (36.36) | 0 (0.00) | 33 (100.00) |
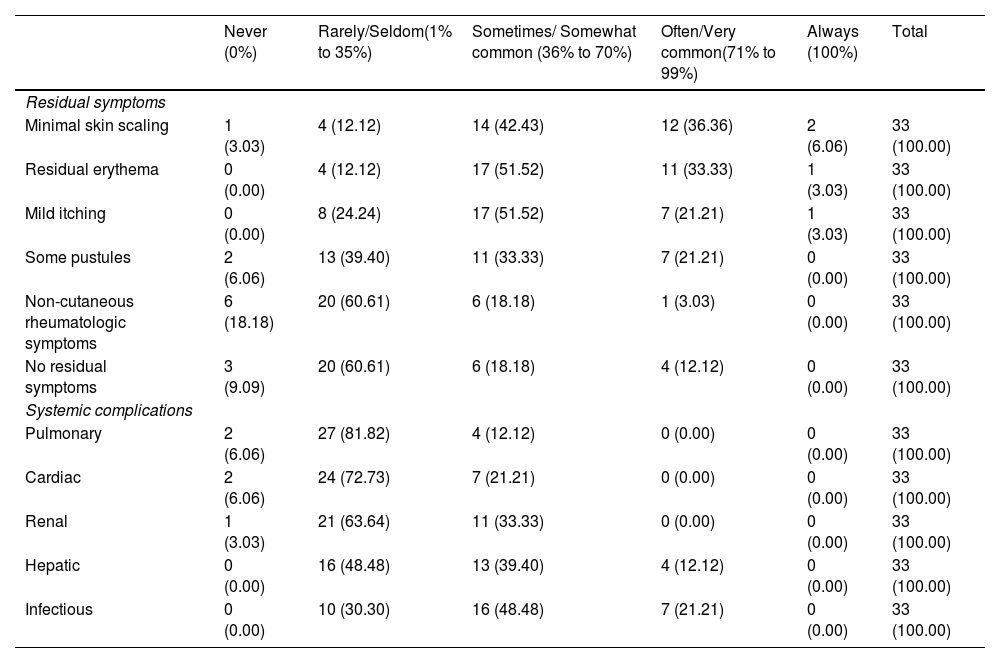
According to most dermatologists, flare-ups rarely resolve without residual symptoms, being minimal skin scaling, residual erythema, and mild itching somewhat or very common (table 3). Infectious complications are a very common finding, while pulmonary, renal, or cardiac systemic complications are rare (table 4).
Frequency of residual symptoms and systemic complications.
| Never (0%) | Rarely/Seldom(1% to 35%) | Sometimes/ Somewhat common (36% to 70%) | Often/Very common(71% to 99%) | Always (100%) | Total | |
|---|---|---|---|---|---|---|
| Residual symptoms | ||||||
| Minimal skin scaling | 1 (3.03) | 4 (12.12) | 14 (42.43) | 12 (36.36) | 2 (6.06) | 33 (100.00) |
| Residual erythema | 0 (0.00) | 4 (12.12) | 17 (51.52) | 11 (33.33) | 1 (3.03) | 33 (100.00) |
| Mild itching | 0 (0.00) | 8 (24.24) | 17 (51.52) | 7 (21.21) | 1 (3.03) | 33 (100.00) |
| Some pustules | 2 (6.06) | 13 (39.40) | 11 (33.33) | 7 (21.21) | 0 (0.00) | 33 (100.00) |
| Non-cutaneous rheumatologic symptoms | 6 (18.18) | 20 (60.61) | 6 (18.18) | 1 (3.03) | 0 (0.00) | 33 (100.00) |
| No residual symptoms | 3 (9.09) | 20 (60.61) | 6 (18.18) | 4 (12.12) | 0 (0.00) | 33 (100.00) |
| Systemic complications | ||||||
| Pulmonary | 2 (6.06) | 27 (81.82) | 4 (12.12) | 0 (0.00) | 0 (0.00) | 33 (100.00) |
| Cardiac | 2 (6.06) | 24 (72.73) | 7 (21.21) | 0 (0.00) | 0 (0.00) | 33 (100.00) |
| Renal | 1 (3.03) | 21 (63.64) | 11 (33.33) | 0 (0.00) | 0 (0.00) | 33 (100.00) |
| Hepatic | 0 (0.00) | 16 (48.48) | 13 (39.40) | 4 (12.12) | 0 (0.00) | 33 (100.00) |
| Infectious | 0 (0.00) | 10 (30.30) | 16 (48.48) | 7 (21.21) | 0 (0.00) | 33 (100.00) |
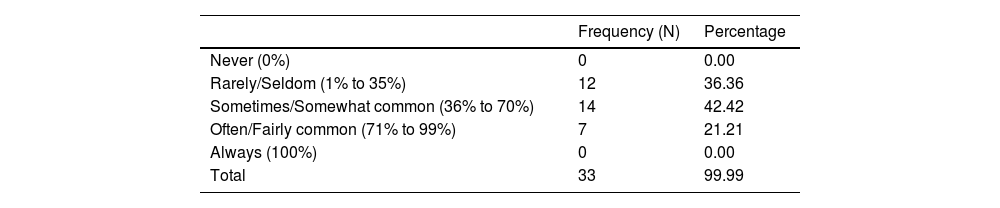
Frequency with which patients require consultation with specific services due to psychosocial impact.
| Frequency (N) | Percentage | |
|---|---|---|
| Never (0%) | 0 | 0.00 |
| Rarely/Seldom (1% to 35%) | 12 | 36.36 |
| Sometimes/Somewhat common (36% to 70%) | 14 | 42.42 |
| Often/Fairly common (71% to 99%) | 7 | 21.21 |
| Always (100%) | 0 | 0.00 |
| Total | 33 | 99.99 |
A total of 45% of dermatologists indicated that hospitalization due to a flare-up is very common, and 82% that admission to the ICU is uncommon. The length of stay is often < 1 to 2 weeks (70%).
A total of 70% indicated that patients with GPP require between 4 and 6 annual visits to the dermatologist. There was disparity of opinions among dermatologists on the frequency with which a patient requires referral to specific services and/or treatment following the psychosocial impact of the disease (table 4).
A total of 52% of dermatologists indicated that the mean time of the sick leaves associated with a flare-up is 2 to 4 weeks, while 48% indicated it is over 4 weeks.
Two deaths were reported due to GPP or associated complications, which represents 2.1% of the patients with available data (n = 97).
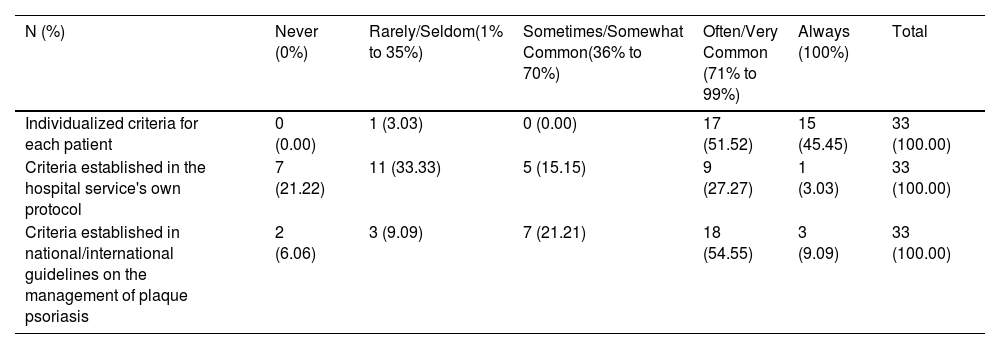
Management of the diseaseThe criteria used for therapeutic decision-making in patients with GPP often or always involve individualized criteria for each patient (97%) and/or criteria established in national/international clinical practice guidelines on the management of plaque psoriasis (64%) (table 5).
Frequency of criteria for therapeutic decision making in patients with GPP.
| N (%) | Never (0%) | Rarely/Seldom(1% to 35%) | Sometimes/Somewhat Common(36% to 70%) | Often/Very Common (71% to 99%) | Always (100%) | Total |
|---|---|---|---|---|---|---|
| Individualized criteria for each patient | 0 (0.00) | 1 (3.03) | 0 (0.00) | 17 (51.52) | 15 (45.45) | 33 (100.00) |
| Criteria established in the hospital service's own protocol | 7 (21.22) | 11 (33.33) | 5 (15.15) | 9 (27.27) | 1 (3.03) | 33 (100.00) |
| Criteria established in national/international guidelines on the management of plaque psoriasis | 2 (6.06) | 3 (9.09) | 7 (21.21) | 18 (54.55) | 3 (9.09) | 33 (100.00) |
GPP, generalized pustular psoriasis.
In the event of a GPP flare-up, 67% of dermatologists often or always use non-biologic systemic drugs as the first-line therapy. The most widely used ones are cyclosporine (55%) and oral retinoids (30%) (figure 2A) as opposed to 45% of dermatologists who often or always use a biologic drug as the first-line therapy, being anti-TNFα (52%) and anti-IL-17 (39%) the most common ones (figure 2B). In this context, 55% of dermatologists considered that patients often or always require a combination of different systemic/biologic drugs to control the flare-up.
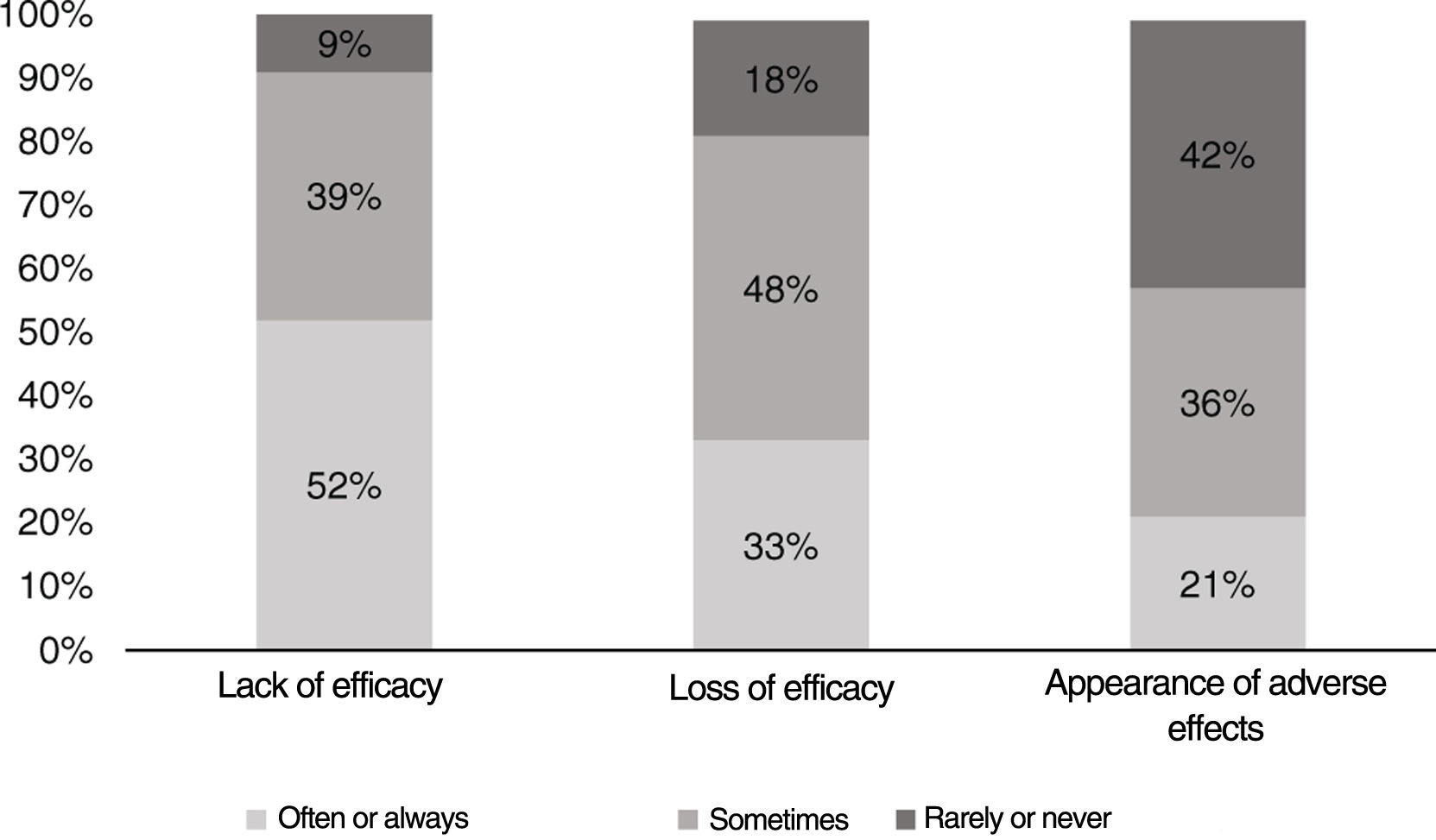
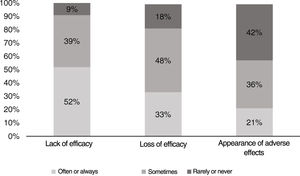
When the therapeutic strategy used to treat the flare-up fails, 52% of dermatologists indicated that it is often due to a lack of efficacy, 48% that it is sometimes due to loss of efficacy, and 42% that it is rarely due to the appearance of side effects (figure 3).
Once the flare-up is controlled, 61% of dermatologists use the same treatment for maintenance as for flare-up control.
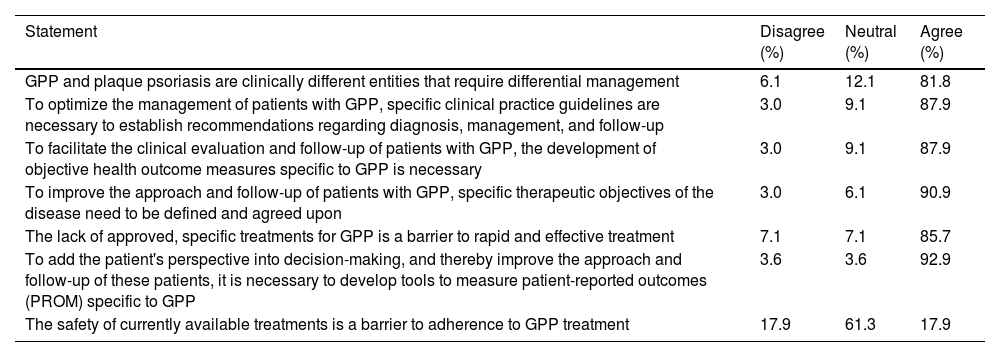
Challenges in the management of generalized pustular psoriasisTable 6 illustrates the consensus reached on the current challenges faced in the management of GPP after 2 rounds of Delphi consultation, with 33 dermatologists participating in the 1st round (response rate, 18%) and 28 in the 2nd one (response rate, 85%).
level of consensus reached by dermatologists on various aspects related to GPP.
| Statement | Disagree (%) | Neutral (%) | Agree (%) |
|---|---|---|---|
| GPP and plaque psoriasis are clinically different entities that require differential management | 6.1 | 12.1 | 81.8 |
| To optimize the management of patients with GPP, specific clinical practice guidelines are necessary to establish recommendations regarding diagnosis, management, and follow-up | 3.0 | 9.1 | 87.9 |
| To facilitate the clinical evaluation and follow-up of patients with GPP, the development of objective health outcome measures specific to GPP is necessary | 3.0 | 9.1 | 87.9 |
| To improve the approach and follow-up of patients with GPP, specific therapeutic objectives of the disease need to be defined and agreed upon | 3.0 | 6.1 | 90.9 |
| The lack of approved, specific treatments for GPP is a barrier to rapid and effective treatment | 7.1 | 7.1 | 85.7 |
| To add the patient's perspective into decision-making, and thereby improve the approach and follow-up of these patients, it is necessary to develop tools to measure patient-reported outcomes (PROM) specific to GPP | 3.6 | 3.6 | 92.9 |
| The safety of currently available treatments is a barrier to adherence to GPP treatment | 17.9 | 61.3 | 17.9 |
GPP, generalized pustular psoriasis.
a Consensus reached in the 2nd round.
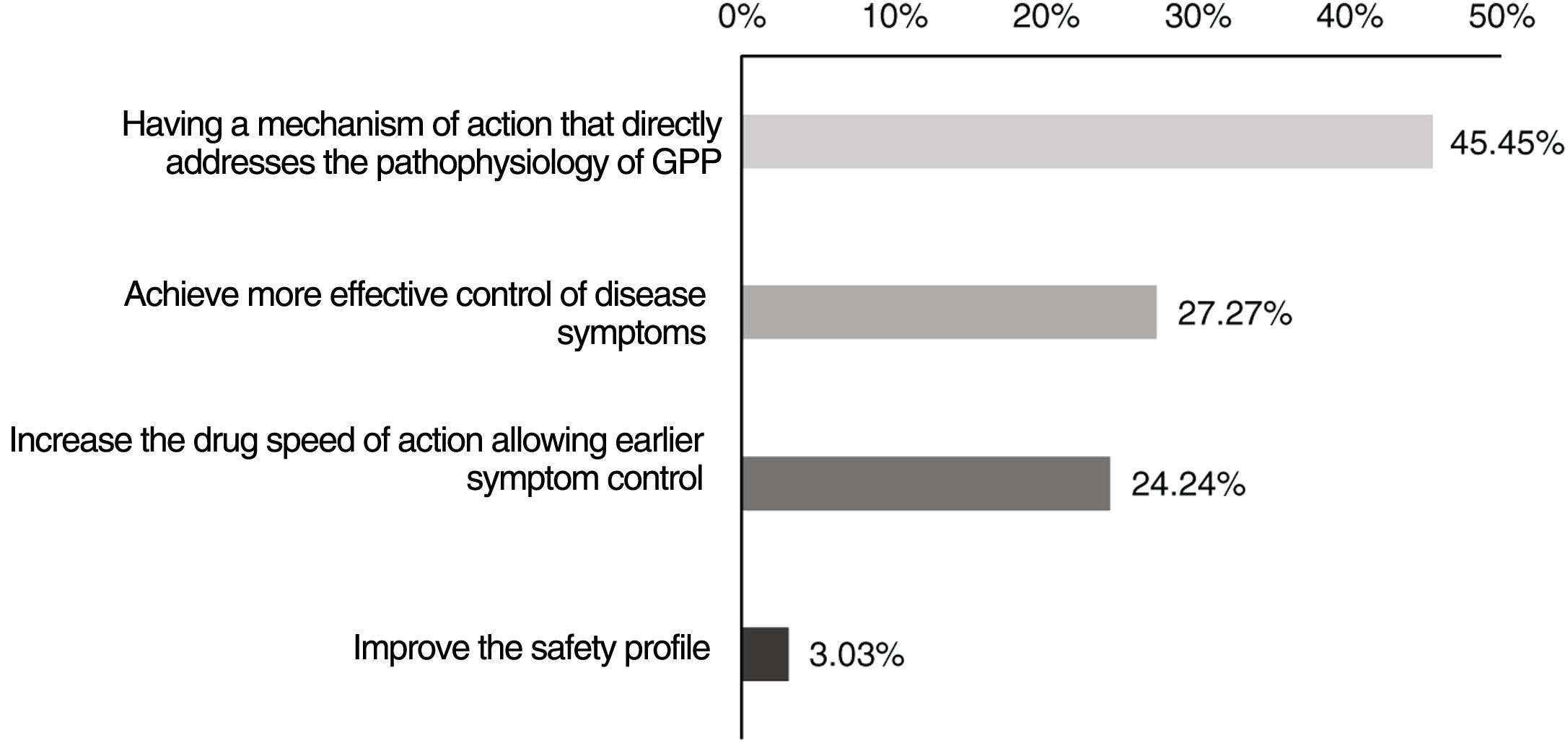
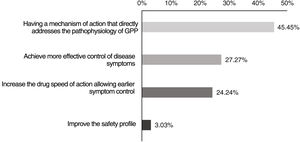
Finally, in the prioritization exercise on the current needs for developing new therapies for GPP, most respondents (45%) said that the top priority is that these drugs should have a mechanism of action directly addressing the pathophysiology of GPP (figure 4).
DiscussionOur study is the first approach ever to the epidemiology of GPP in Spain through a survey directed to dermatologists experienced in GPP.
The estimated 5-year prevalence and incidence were 13.05 and 7.01 cases per million inhabitants, respectively. Recently, data on the incidence of GPP in Spain have been published based on hospital discharges from the minimum basic data set of the National Health System. In this study, the incidence of new GPP related hospitalizations was 3.18 patients per million per year.9 The differences reported in both estimations are due to the methodology used in each one of them, as this study only took hospitalizations into consideration, which may reflect only the most severe cases, while our study gives an overall view of the epidemiological situation of GPP. Few studies have evaluated the epidemiology of GPP in other settings, and data are heterogeneous. Therefore, the reported prevalence estimates vary from 1.76 in France,10 15.3 in Sweden,11 and 124 cases per million inhabitants in Korea.12 We should mention that prevalence is higher in Asian compared to Caucasian populations.6
The age and sex of the patients treated (women, 57%; age range at diagnosis, 30 to 60 years) are similar to those previously published with a mean age of GPP onset at 40 to 60 years,13,14 and more prevalence among women (man/woman ratio between 1.2/1 and 2/1).5,14
According to the specialists consulted, 46% of the patients with GPP had plaque psoriasis, which is consistent with previously published values that state that nearly 31% to 77% of the patients have a history of plaque psoriasis.6,14
On the other hand, the most frequent symptoms reported by dermatologists were pustules, erythema, and scaling, which is consistent with the reports seen in the scientific medical literature on this matter.15 In addition, a similar study to ours conducted in the United States stated that the dermatologists surveyed indicated that the main symptoms leading to suspicion of a GPP flare-up are pustules, worsening of skin lesions, and erythema.16
Similarly to the published data,16,17 dermatologists indicated that 55% of the patients experience less than1 flare-up per year, often requiring hospitalization for 1 to 2 weeks.
Most dermatologists considered infectious complications to be somewhat or very common, while pulmonary, renal, or cardiac systemic complications were considered uncommon. In the scientific medical literature currently available, the most GPP related common complications are secondary infections. However, unlike our study, acute respiratory distress syndrome, acute kidney failure, and congestive heart failure are also reported as common complications in the literature.5,6,14,15
Regarding mortality, dermatologists reported a mortality rate of 2.1%, which is lower than the one reported in the medical literature currently available (3% to 7%).6,14,16,17
Currently, the management of GPP faces certain challenges. Dermatologists agreed on the lack of specific clinical practice guidelines on the diagnosis, management, and follow-up of patients with GPP, and the absence of specifically approved treatments vs GPP, as the main challenges currently faced. As evidence of this, we should mention that, despite the definition of GPP proposed by ERASPEN, not all dermatologists who participated in the study considered pustules to always appear in patients with GPP. We should also mention that espesolimab,18 a monoclonal antibody vs interleukin (IL)-36, has recently been approved to treat GPP flare-ups19 in the European Union, while other regions already have approved treatments such as therapies vs tumor necrosis factor-α and IL-17 and IL-23.7 In this context, when necessary, Spanish dermatologists use currently approved biologic drugs to treat plaque psoriasis in the management of GPP, which is the same management seen in Europe and the United States, although off-label.6,14 The lack of specific tools allowing an objective evaluation of GPP through patient-reported outcomes was also mentioned, as current tools for plaque psoriasis are often used.6 Also, defining specific therapeutic objectives for the disease would improve patient management and follow-up. Furthermore, study participants highlighted the importance of considering the patient's perspective and adding it to the decision-making process.
The study has some limitations. Although the survey was sent to a high number of dermatologists, only 33 responded to the survey. However, considering the low prevalence of the disease and the requirement of having seen, at least, 1 patient in the last 5 years, we believe that the sample size is adequate and representative of the disease situation in Spain. We should mention that the estimated prevalence and incidence obtained constitute an approximate approximation, given that consulting the patients’ health records was not required, and therefore, there could be a memory bias on the part of some participants. On the other hand, and although it was not the objective of this study, patient opinions were not collected, and therefore, their perspective on the disease burden is not reflected, which is something that should be taken into consideration in future studies.
In conclusion, our study provides an overall view of the status of GPP in Spain through the perspective of dermatologists. Results expand our current knowledge of the disease while potentially help us establish or improve clinical practice guidelines and highlight the specific needs of GPP.
FundingThis project was initiated and funded by the Spanish Academy of Dermatology and Venereology (AEDV) and managed through the Spanish Psoriasis Working Group thanks to an unrestricted grant from Boehringer Ingelheim. No person related to Boehringer Ingelheim has participated in the proposal development, or in the drafting of this manuscript.
Conflicts of interestEV has received consultation and lecture fees, and/or participated in sponsored clinical trials conducted by Abbvie, Almirall, Amgen, Bayer, Boehringer Ingelheim, Celgene, Gebro, Isdin, Janssen, LEO Pharma, Lilly, Merck Serono, MSD, Novartis, Pfizer, Roche, Sandoz, Sanofi, and UCB.
RR has received consultation and lecture fees, and/or participated in sponsored clinical trials conducted by Abbvie, Almirall, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Incyte, Janssen, LEO Pharma, Lilly, Novartis, Pfizer, Sandoz, and UCB.
NE has received consultation, and/or lecture fees and support to attend meetings, and/or travel from Abbvie, Janssen, LEO Pharma, Lilly, Almirall, Novartis, and UCB.
GC has received consultation and/or lecture fees from Janssen, Abbvie, Novartis, Pfizer, MSD, and Celgene.
PC has received consultation and lecture fees, and/or participated in sponsored clinical trials conducted by Abbvie, Almirall, BMS, Boehringer, Celgene, Janssen, LEO Pharma, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi, and UCB.
JMC has received consultation and lecture fees, and/or participated in sponsored clinical trials conducted by Boehringer Ingelheim, Janssen, LEO Pharma, Lilly, Amgen, BMS, Sandoz, Almirall, Novartis, and Abbvie.
The authors would like to thank the members of the Spanish Psoriasis Working Group (PWG) for their contributions to the document and Outcomes’10 for the support and methodological coordination of the project.