The use and acceptance of teledermatology increased more in the last 2 months of the recent lockdown owing to coronavirus disease 2019 than in the preceding 20 years. This sudden popularity –even among the greatest skeptics– was driven by the need to offer solutions to patients in both public and private settings who suddenly found themselves unable to access in-person dermatological care. Even departments already offering an asynchronous, store-and-forward teledermatology service were obliged to create new systems to support direct interaction between specialists and patients (the direct-to-consumer model). This article suggests some practical ways to implement TD safely and to expedite and optimize teleconsultations; these ideas are not just applicable to a pandemic situation
La teledermatología ha avanzado en aceptación y uso en los últimos 2 meses de confinamiento por SARS-CoV-2 más que en los últimos 20 años. Su repentina popularidad –aun entre los más escépticos– ha sido el resultado de buscar una respuesta a las necesidades de los pacientes, que se han encontrado bruscamente sin atención dermatológica presencial tanto en lo privado como en lo público. Incluso aquellos servicios que incluían la modalidad asíncrona tuvieron que generar sistemas que permitieran la atención directa (direct-to-consumer) entre el especialista y el paciente. El siguiente artículo propone algunas maneras prácticas de implementación segura para agilizar y optimizar las consultas dermatológicas, aplicables no solamente a tiempos de pandemia.
Teledermatology (TD) is experiencing a golden age. Although it has been used for more than 20 years,1,2 its implementation has been slow. This slowness was first justified by its high cost following initial analyses, which appeared to support this theory, but access to quality photographic and dermoscopic equipment at more than affordable prices and to simple platforms for developing it have shown that, far from being more expensive, it represents savings not only in terms of material but also in terms of indirect costs and organization (fewer expenses in support personnel, physical space, health care transport, and occupational social costs).3 A second argument was the reticence of patients and primary-care physicians: it has now been shown that both groups widely accept virtual consultations.4,5 Third, the focus was placed on the management of institutions, who, contrary to expectations, at least at national level, have shown great interest in implementing systems that allow them to optimize management of dermatology consultations by improving both accessibility and results through the use of technology.
Only one loose end remains: the dermatology specialist. Although Spain is among the leading European countries in terms of active TD programs, with 25% of hospital departments having implemented some form of TD in consultations by 2014,6 much remains to be done. Several reasons exist for this resistance to TD (Table 1). The intrusion of SARS-CoV-2 into daily life worldwide has made it clear that our way of practising medicine needs rethinking. We must be able to react to future lockdowns as a cohesive medical corps and we must also use this opportunity to optimize our daily hospital and private work under normal conditions.
Some of the Fears Expressed by Specialists on the Implementation of TD and their Counterarguments.
| Common Fear | Counterargument |
|---|---|
| Continue to see TD as an “inadequate” way of seeing patients, an inferior form of consultation. | Depending on the functionality, TD may even be clearly better than in-person consultations, such as for screening. |
| Fear of diagnostic or management error. | Reliability and validity have been shown in a multitude of studies. |
| Fear of increased demand for consultations. | Better access may increase demand but also moderates it. |
| Fear of losing control of the profession. | On the contrary, TD provides control over demand and access. |
| Fear of being replaced by “machines” and loss of jobs. | By improving access and quality of patient care, departments tend to increase the number of physicians. |
| Fear of virtual consultations being taken by dermatologists from other countries or other areas. | The reality is that some underserved areas exist where TD alleviates the lack of specialists. |
| Fear that better resolution in the public sector will result in a reduction in private consultations. | TD is applicable in an efficient form in public and private medicine. |
| Fear of overburdening primary care. | Weekly referrals by doctors are scarce, overload is not high, and it is compensated for by improvements in training. |
The lack of dermatologists worldwide7 and the need to optimize resources makes it necessary to make decisions to manage consultations more appropriately. As long as dermatology departments indiscriminately receive any skin condition, no matter how irrelevant, there will never be enough human resources to invest in the patient-care system.
One of the advantages of TD is the fact that it allows the specialist to select rapidly and accurately which diseases should be attended in person and which do not need to be seen in hospital (cosmetic procedures and most benign tumors, for example). This screening is key to dealing with the avalanche of skin cancers due to the aging of the population and exposure to the sun through work and leisure, with cases numbering in the millions. Triage through TD has reduced in-person consultations by between 20% and 30%.8 Implementation of asynchronous (store-and-forward) TD systems between the specialist and the family doctor facilitate high quality clinical and dermoscopic images that can be used for the following purposes:
- -
Lesion triage. Lesions that require an in-person consultation (biopsies, excisions) are selected.
- -
Diagnosis and treatment for inflammatory disease (common psoriasis, eczema) and infectious disease (superficial mycosis, herpes).
- -
Monitoring a patient’s known conditions and controlling medication: psoriasis, acne, or rosacea.
- -
Indicating noninvasive therapies (PDT and natural daylight) or topical treatments following clinical, dermoscopic, or histopathology diagnosis. It is ideal for patients with limited mobility, patients who require treatment for solar damage, or topical treatment after diagnosing superficial carcinomas.
- -
Indicating analyses or imaging studies prior to the in-person consultation.
The images taken by family physicians are of increasingly high quality both because these doctors have gained experience and because the cameras of today’s smartphones take very good quality photographs with minimal photographic training. Security in terms of image transfer can be resolved by deleting the photograph taken of the patient from the cellphone once it has been downloaded to be sent or by using cellphones belonging to the institution, or by means of dedicated apps that do not save the images in the phone’s gallery but in encrypted form in the application itself (such as Clinicam®, developed by SESCAM).9
In terms of the platform, although it would be ideal to have a single national hospital system, the reality is that each asynchronous TD center has installed its own system and has included it in the clinical records, which allows for safe handling of all the patient’s medical information (not just images). The entire TD system must have an appropriate level of integration both in terms of the digital medical records and of the systems for making appointments, ordering additional tests, and identifying users. It should also have access to the electronic prescription system, which will make it possible to indicate new treatments and adjust or reactivate prescriptions. In the private sphere, several platforms provide asynchronous TD that ensures data protection. Images or other patient data should not be sent via social medias or unsecure electronic means.
Appropriate triage frees up time, which can be dedicated to patients with more difficult or severe disease, thus preventing exhaustion of scarce human resources in handling uncomplicated conditions. In this way, hospital departments with long waiting lists who continue to refuse to manage them by using a tool of recognized efficacy like TD with the argument that in-person care is the “only and best alternative” for managing medical consultations, will be preventing their patients from being seen in a timely manner and will be wasting the resources available to them.
Some asynchronous TD systems include sending reports to the patients (such as that of Hospital Virgen Macarena). This system provides patients with the knowledge that the specialist has been consulted and the specialist’s recommendation regarding therapy. This report will include the diagnosis and treatment or may be an automatic response that includes one of these 3 possibilities: a) the condition is benign and does not require treatment; b) proposed treatment or indication to contact the family physician; or c) appointment at the hospital to complete treatment. The first type of report requires generating templates with the most common diseases and provides patients with complete information about their conditions. The second type of response is easier to send and provides less information.
DuringWith the arrival of SARS-CoV-2 and the lockdown of the population as a result of the pandemic, patients suddenly found themselves without specialists to consult in person, in both the public and private sectors. The psychological impact of lockdown and the high mortality rate among the elderly and those with comorbidities increased the sensation of being abandoned among the population.
Asynchronous TD systems suddenly became impracticable as patients and even the doctors themselves were confined to their homes or in the emergency departments. It was necessary to switch to the system of telephone calls. Hospitals such as that of the authors used computers connected to the electronic medical records and telephones, which allowed their assistants to work from home via VPN. Some departments made hundreds of phone calls to determine the immediate needs of their patients and to be closer to them, and even identifying cases that might require the support of social services. In other hospitals, such as those of the Autonomous Community of Andalusia, a corporate technological solution was developed and implemented to send images and documents directly between physicians and patients. Many patients, especially among the elderly, were anxious and afraid. Reducing loneliness and the feeling of being abandoned in this group was important and was possible thanks to telephone calls. Where necessary, the lack of an image of the condition was solved by the patients themselves or their friends or family taking photographs and then sending them to the corporate e-mail address in some centers and in others, via an SMS system incorporated in the electronic medical records, through which the patient send the images directly to the specialist.
The results were highly satisfactory for the doctors and the patients who worked with these systems. Having good quality images sent by the patients facilitated qualitative and quantitative evaluation and made it possible to make decisions regarding treatment, medical discharges, etc. Having been trained in evaluating TD consultations made the entire process faster, more efficient, and with fewer errors.
AfterNow that it is clear that TD is finally here to stay, the system that appears to work best at present is the following:
- -
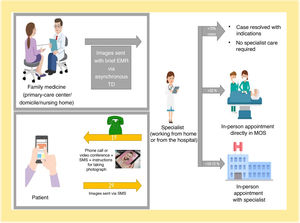
Asynchronous TD between family physician and specialist, with implementation of channels that make it possible to communicate between them more easily (messaging systems that are part of the electronic medical records platform) in order to exchange opinions, send comments regarding treatments, etc.
- -
Direct TD with the patient, by means of a telephone call or videoconference and exchange of images or other files (reports in PDF format) via SMS (Figs. 1 and 2).
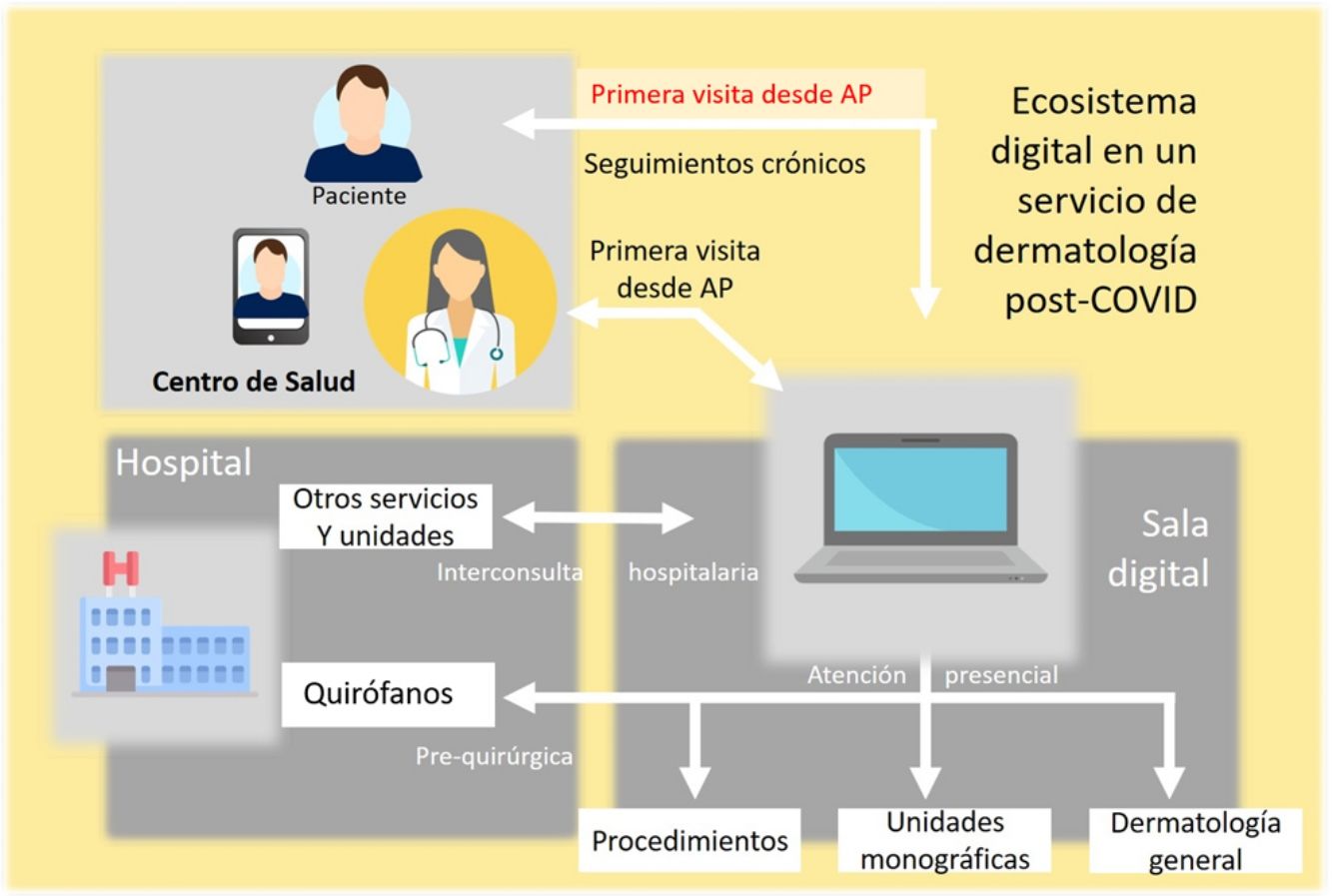
The dermatology department of the immediate future must have access to technologies (networks, platforms, applications, hardware) with which to generate a digital ecosystem that is integrated in all the clinical and patient-care activities. The implementation and successful rollout of this ecosystem will require a thorough but gradual functional redesign of the dermatology department, which includes the following structural, technical, and functional components (Table 2):
- -
Telemedicine platform integrated in the information systems and with functionalities for the following types of digital consultation:
- -
Indirect, asynchronous consultation: virtual consultation between the family physician and the dermatologist by means of clinical and dermoscopic images taken at the health care center for the initial visit from primary care. This functionality is applicable to the virtual consultation between a physician at a hospital department and the dermatologist for the hospital internal consultation and outpatient internal consultation.
- -
Direct, asynchronous consultation: virtual consultation between the patient and dermatologist by means of clinical images taken using the patient’s smartphone. This functionality is applicable to follow-up patients with chronic skin disease or in systemic treatment for control of the disease or therapeutic response. This functionality also allows for the initial visit of the patient to the dermatologist in situations where it is not possible to access the health center (lockdown, seasonal isolation, etc.).
- -
Real-time virtual consultation (video consultation): consultation between the patient or the family doctor and the dermatologist by means of an audio and video connection. This functionality is applicable to resolving specific incidences of patients in follow-up by the dermatology department. In the setting of private dermatology or in situations with low patient-care pressure, it can also be seen as a way of accessing the dermatologist.
- -
Reorganization of schedules and in-person activity in the dermatology department.
- -
Definition and generation of schedules for direct care of patients evaluated by means of virtual consultation and candidates for an in-person consultation without criteria for a monographic consultation.
- -
Availability of a schedule or procedures unit to apply treatments as a single event for patients seen by virtual consultation.
- -
Definition of consultation criteria in a monographic unit and procedure for direct management of appointments in these units.
- -
Redesign of care processes between the dermatology department and the primary care center with the objective of responding to the following needs:
- -
Performing necessary additional tests in the community (health center, domicile) to begin systemic treatments, guidance, diagnosis, etc.
- -
Direct access, apart from the virtual consultation, by primary-care professionals to the dermatology service.
- -
Procedure for managing patients seen via TD and not sent for an in-person consultation at the hospital (follow-up in primary care, discharges).
- -
Opening of the informed-consent process in patients enrolled in presurgical TD programs.
Recommendations on the Use of Modalities of Teledermatology.
| Indirect family doctor-dermatologist | Direct patient-dermatologist | |
|---|---|---|
| Deferred (store and forward) | Access to the initial visit from primary care | Follow-up of chronic patients |
| Static clinical and dermoscopic images | Perioperative care (preoperative and postoperative) | |
| Cosmetic periprocedural care (preprocedural and postprocedural) | ||
| Inability to access the health center for the initial visit with the dermatologist (lockdown, seasonal isolation, etc.) | ||
| Real time (video consultation or audio interaction) | Access to dermatologic care in closed institutions (prisons, nursing homes, etc.) | Access to dermatologic primary care in situations with low workloads |
| Follow-up of chronic patients | ||
| Perioperative care (preoperative and postoperative) | ||
| Cosmetic periprocedural care (preprocedural and postprocedural) | ||
| Inability to access the health center for the initial visit with the dermatologist (lockdown, seasonal isolation, etc.) |
TD is here to stay and the pandemic has shown that the efficient management of a dermatology department requires this tool to resolve a large number of dermatology consultations. In the initial screening, TD is unbeatable for speed and effectiveness, and the pandemic has shown us that it is possible to carry out part of the consultations online, including highly complex cases, with considerable savings in terms of time and expense, and with high satisfaction of physicians and patients. Overall, the percentage of cases that can potentially be managed at a distance may exceed 70%.
This will leave a not inconsiderable number of consultations that must be held in person, to which specialists can dedicate more time and resources. This group includes more complex cases, to which the current system, in departments that do not include TD, dedicates little consultation time.
In the near future, many of the consultations carried out today using TD will be made even easier by means of the combination of specialist and machine. But these improvements will only benefit those patients visiting departments that satisfactorily incorporate TD in their routine practice.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Pasquali P, Romero-Aguilera G, Moreno-Ramírez D. Teledermatología en tiempos de pandemia: El antes, el durante y el después. Actas Dermosifiliogr. 2021;112:324–329.