Treatment options for hidradenitis suppurativa include light-based therapy. This systematic review aimed to update our understanding of the efficacy, effectiveness and safety of these treatments for hidradenitis suppurativa by evaluating the literature published since the 2015 Cochrane review on this topic. We conducted an electronic search of the following databases: MEDLINE, EMBASE, University of York Centre for Reviews and Dissemination database, Cochrane Database of Systematic Reviews, Cochrane Skin Group Specialised Skin Register, University of Nottingham’s Centre of Evidence Based Dermatology database, and TESEO. The systematic review included 6 case series, 3 systematic reviews, and 2 clinical trials on the use of conventional and intralesional photodynamic therapy, intense pulsed light therapy, and Nd:YAG, carbon dioxide, and diode laser therapy for hidradenitis suppurative in 248 patients.
La terapia con luz es una alternativa en el tratamiento de la hidradenitis supurativa (HS). El objetivo fue evaluar la eficacia, efectividad y seguridad de las distintas modalidades de terapia con luz en la HS, mediante una revisión sistemática actualizando la realizada en 2015 procedente de Cochrane Library. Se identificaron los estudios mediante una búsqueda electrónica en las bases de datos: MEDLINE, EMBASE, Universidad de York, Cochrane Database of Systematic Reviews, Cochrane Skin Group, Centre of Evidence based dermatology de la Universidad de Nottingham, TESEO finalmente se incluyeron 6 series de casos y 3 revisiones sistemáticas y 2 ensayos clínicos de pacientes tratados con terapia fotodinámica convencional o intralesional, láser Nd:YAG, CO2 o diodo y luz intensa pulsada, con un total de 248 pacientes tratados.
Hidradenitis suppurativa (HS) is a chronic, debilitating inflammatory disease of hair follicles and their associated sebaceous glands. HS usually appears after puberty. Underlying the condition is immune dysregulation in a genetically predisposed individual.1 The general population prevalence, which ranges from 0.1% to 1%, is higher in the second and third decades of life and in women.2 Smoking, obesity, hormonal imbalance, and stress from friction or shaving can trigger or aggravate HS.3
Nodules, abscesses, suppurative fistulous tracts, and scarring in skin folds (mainly the armpits, groin, and anogenital regions) are the most common presentations.4 The main symptoms are pain, burning or a local sensation of heat; pruritus; and hyperhidrosis. These manifestations have a negative impact on quality of life.5
The management of HS is complex and requires a multidisciplinary approach.6 Light-based treatments have been used experimentally in recent years. Photodynamic therapy (PDT) involves applying a photosensitizer that produces reactive oxygen species in a process that leads to cellular destruction. The hypothesized benefit of PDT in HS is based on a direct cytotoxic effect on biofilm bacteria and sebaceous glands as well as on immunomodulation.1 When a photosensitizer is applied topically to HS lesions, accumulation occurs more easily than in normal skin because openings and fistulas facilitate penetration.7 Lesions improve with light activation. Light at a wavelength of 630nm is sufficient for activating 5-aminolevulinic acid (ALA) and methylene blue (MB), which are 2 of the photosensitizers used.8 Topical PDT has advantages that make it an attractive alternative therapy for treating multiple lesions simultaneously; it is minimally invasive, has few adverse effects, and is well tolerated.9
Intense pulsed light (IPL) therapy uses a broad spectrum, high energy, noncoherent light. The underlying principle is photon absorption by endogen or exogen chromophores. The transfer of energy to target cells (in HA, the occluded hair follicle unit) generates heat, destroying the lesion in a process termed selective photothermolysis.10 IPL also has an antimicrobial effect due to the activation of bacterial porphyrins, which generates reactive oxygen species and leads to cell death.11
Nd:YAG, carbon dioxide (CO2), alexandrite, and diode laser therapies have also been used to treat HS. The aim of these treatments is to reduce the number of hair follicles in areas where HS lesions tend to develop.12
This systematic review aimed to update our understanding of the efficacy and safety of the various modalities of light-based therapy applied in HS. We considered both conventional PDT and intralesional and laser treatments. However, we did not compare them, given that their mechanisms of action differ and publications are few.
Material and MethodsLiterature Search StrategyWe searched for articles on light-based therapies used alone or with a photosensitizer (PDT) to treat HS. Articles had to be published between August 2015 and March 1, 2019. Additional limiters were set to select studies in humans that were published in either Spanish or English. We started the search with August 2015 because a systematic review in the Cochrane Library was updated at that time. Our intention was to update that review with the results of more recent studies.
We also searched backwards from the reference lists to identify any cited articles meeting our inclusion criteria.
The following databases were used: MEDLINE (through PubMed), EMBASE, the Centre of Reviews and Dissemination (University of York), the Cochrane Library (in the Cochrane Database of Systematic Reviews), the Cochrane Skin Group, the Centre of Evidence Based Dermatology (University of Nottingham), and TESEO (the Andalusian database of PhD theses). The following trial registries were also consulted: ClinicalTrials.gov, reec.aemps.es, and Clinicaltrialsregister.eu.
Finally, the PROSPERO register was searched for systematic reviews on HS. We specified reviews that included light-based therapies.
Search terms were chosen from the list of Medical Subject Headings (English) and its equivalent in Spanish (Descriptores en Ciencias de la Salud), as follows: photochemotherapy, photodynamic therapy, hidradenitis suppurativa, suppurative hidradenitis, light, lasers, laser therapy, intense pulsed light therapy.
Article inclusion criteria were as follows:
- •
Type of study: randomized controlled clinical trials (RCTs), systematic reviews, observational studies with a control group, and observational studies without a control group (case series)
- •
Population: adults with HS regardless of sex, ethnicity, comorbidity, or prior treatment
- •
Limiter: inclusion of patients whose HS was treated with PDT (using any type of laser or other light source)
- •
Limiter: publication in Spanish or English
Article exclusion criteria were as follows:
- •
Publication outside the time frame
- •
Studies not using accepted, validated HS evaluation tools (eg, the Hidradenitis Suppurativa Clinical Response criterion, the modified Sartorius score, and/or the Physician Global Assessment [PGA] of HS)
- •
Case series with fewer than 5 patients
- •
Editorials and narrative reviews
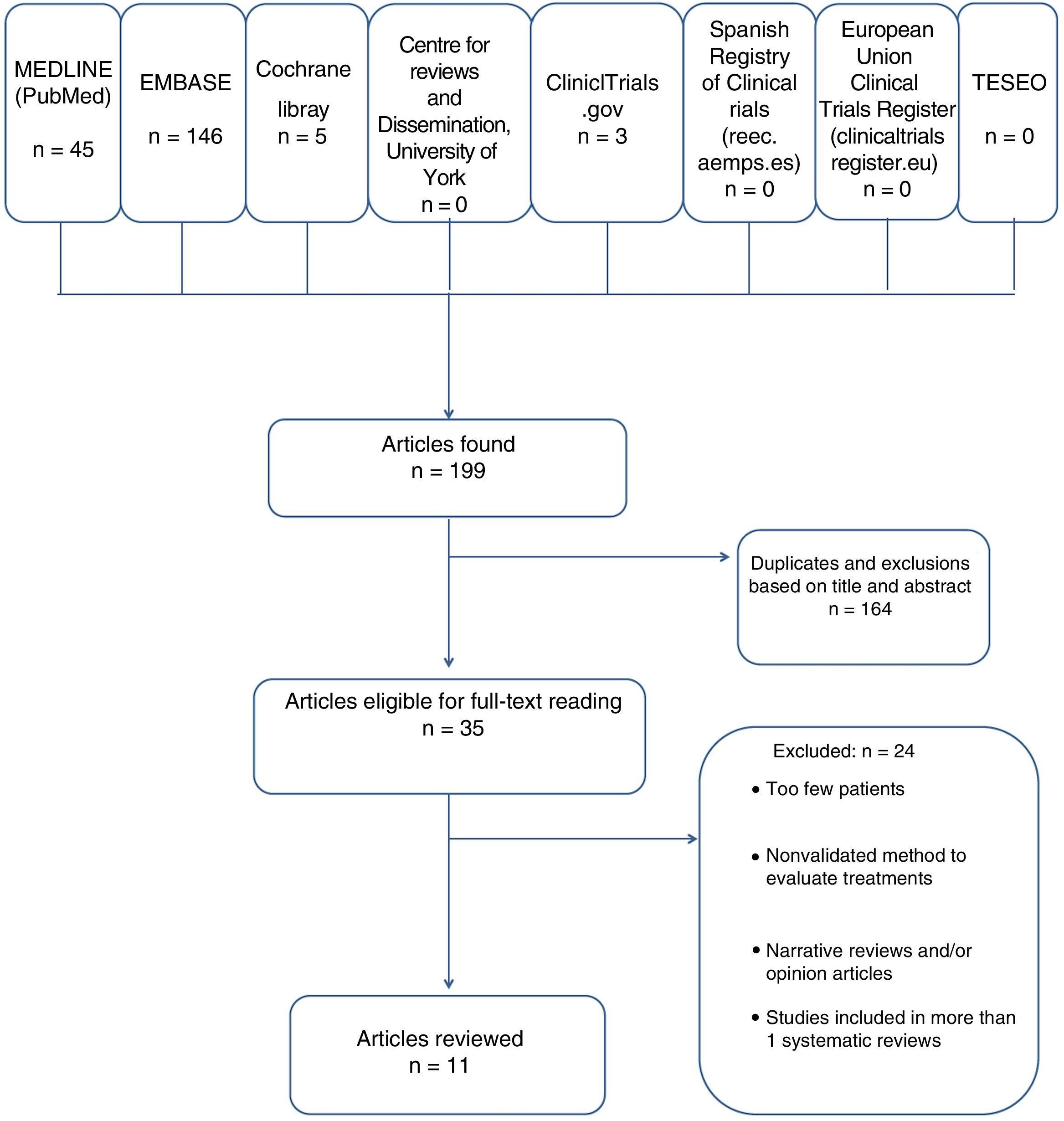
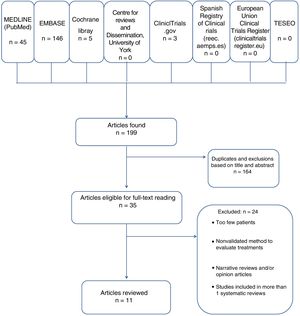
Search results were downloaded with Mendeley reference management software, with titles and abstracts in separate fields. All duplicate, discarded, and selected references were recorded (Fig. 1). The literature searchers were not blinded to authors’ names or institution or the publishing journal.
The scale of Jadad et al13 was used to evaluate RCTs. Critical analysis was based on the CONSORT guidelines (Consolidated Standards for Reporting Clinical Trials).14 The tool of the Basque Office for Health Technology Assessment (OSTEBA, its Spanish acronym)15 was used to assess the quality of evidence afforded by several types of studies and build a table synthesizing the results.
ResultsIncluded and Excluded StudiesOf the 199 studies found, we excluded 164 after removing duplicates and assessing the titles and abstracts. We evaluated 35 full texts, excluding 24 that did not meet the inclusion criteria. Some did not have 5 patients.9,12,16–37 (See Appendix B, supplementary material.) Because few clinical trials and systematic reviews were found, we included case series even though their evaluation of efficacy and effectiveness is limited.
Thus, we evaluated 6 case series (5 prospective and 1 retrospective). The evidence level was low in 4 of the series and moderate in 2 of them.
Most studies were carried out in Europe (Spain, the United Kingdom, France, and Italy), the United States, and Egypt. The remaining inclusions were 2 moderate-quality RCTs and 3 high-quality systematic reviews. The reviews included 4 trials and 5 case series on light-based treatments and are analyzed in depth in the present systematic review: Fadel and Tawfik,38 Highton et al,11 Tierney et al,39 Calzavara-Pinton et al,40 Schweiger et al,41 Sotiriou et al,42 Mahmoud et al,43 Madan et al,44 and Xu et al.45
Tables 1–3 summarize the studies’ periods of follow-up, numbers of patients and losses, population characteristics and interventions. One relevant study2 was found in a backward citation search of references.
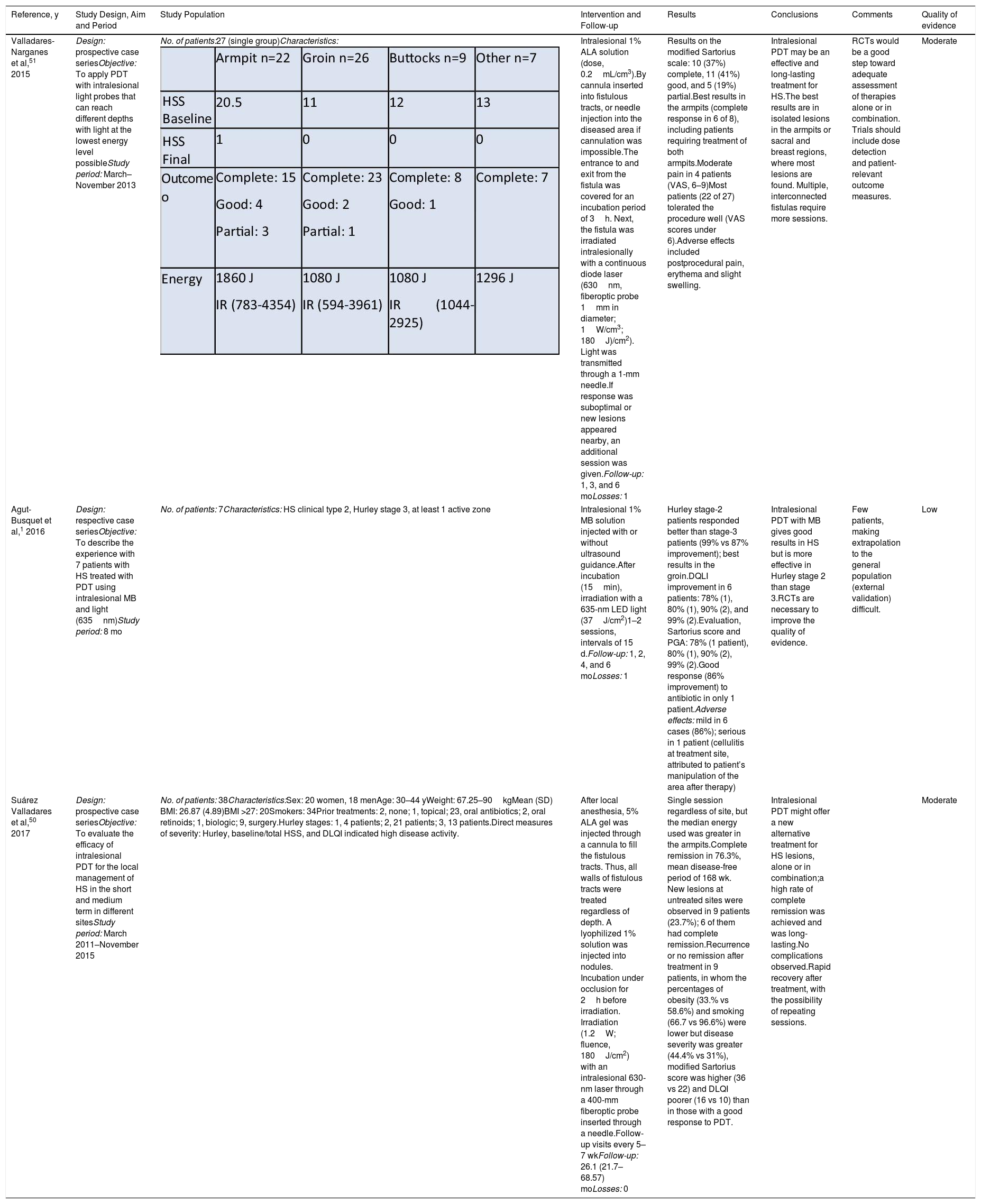
Summary of Studies Included in Systematic Reviews That Used PDT Alone or in Combination With Surgery to Treat HSa,b
| Reference, y | Study Design, Aim and Period | Study Population | Intervention and Follow-up | Results | Conclusions | Comments | Quality of Evidence |
|---|---|---|---|---|---|---|---|
| Andino Navarrete et al,2 2014 | Design: prospective case seriesObjective: To assess the efficacy (Sartorius, DLQI) and safety of PDT+ALA and 635-nm light treatment of moderate to severe HS | No. of patients: 5Characteristics: HS type 2 or Hurley stage 3; 4 armpit lesions, bilateral + 1 pubic;1 man, 4 women;Mean age, 26(5) y; Mean time since onset, 4(1) y | 20% ALA solution for 1.5h; light (635nm, 37J/cm2, 70mW/cm2) per sessionMinimum 4 sessions spaced 1–2 wkFollow-up: 4 and 8 wkLosses: 0 | Significantly improved severity, DLQI, and VAS scores at 8 wkMean Sartorius decrease of 35(5) to 18(8) pointsDLQI decrease, 21 points after 4 sessions, sustained at 8 wkVAS pretreatment, 3; decrease (0–1) at 4 and 8 wk, all patientsOnly adverse effect, burning on irradiation (2 patients) | Treatment with topical 20% ALA and 635-nm light could be effective for refractory HS, decreasing severity and improving QoL. | Small series, limiting external validity and extrapolation | Low |
| Fadel and Tawfik,38 2015 | Design: single-blind RCTObjectives: To assess the efficacy and safety of MB niosome gel as photosensitizer in IPL treatment of HSStudy period:6 mo (month and year not specified) | No. of patients: 17, intraindividual (contralateral control); 6 exclusions; 11 cases analyzed.Characteristics: 7 women, 4 men; mean age 27.1 y (range, 17–35 y).Lesions: both armpits (4); multiple gluteal (3); groin (2); under breasts (1).No topical or systemic treatment 2 weeks before enrollment. | Intervention side: PDT with topical 0.01% MB gel+IPL (630nm, 20ms, 25J) every 2 wk2 sessions/mo up to 6 moControl side: PDT with placebo topical MB-free gel+IPL (630nm, 20ms, 25J/cm2) every 2 wkFollow-up: 1, 3, and 6 mo after treatmentsLosses after randomization: 0 | PDT with topical 0.01% MB gel+IPL was superior to placebo gel; reduction of Sartorius score by 77.3% and 44.1%, respectively.Mean HS-LASI improvement was significant in both groups: active treatment, 77.3% (18.86%); vs placebo gel, 44.1% (28.19%)Similar adverse effects (pain, erythema, hyperpigmentation); no effect of treatment site or disease stageAdverse effects: 0 | IPL (630nm) with this photosensitizer (MB) is effective. MB in niosome formulation enhances dermal penetration.Hair follicle destruction was also attributed to 630-nm λ ray. | Limited by small sample size and short follow-up period. Intraindividual RCTs with more patients and longer follow-up are needed. RCTs with comparators (medical and surgical treatments) are also needed. | Moderate |
| Ingram et al,32015 | Design: systematic review of RCTsObjective: To evaluate the effects of interventions for HS in persons of any agePeriod searched: 1983–2015 | Any person (any sex, age, or ethnicity) with a clinical diagnosis of HS made by a physician and based on a standard definition of the disease | Interventions: More than 40 interventions for HS were included, though evidence was lacking for many. Interventions grouped as pharmacologic, surgical, and other. 3 trials:Fadel and Tawfik,382015Intervention 1: PDT with topical 0.01% MG gel+IPL (630nm, 20ms, 25J/cm2) every 2 wkIntervention 2: PDT with placebo gel+IPL (630nm, 20ms, 25J/cm2) every 2 wk,2 sessions/mo up to 6 moHighton et al,112011randomized sides, 1 untreated control side and 1 treated with IPL, twice weekly for 4 wk (420nm, 7–10J/cm2a 50ms)Tierney et al,392009Left and right sides of the same anatomical structure received 1 of the following treatments:- 10% benzoyl peroxide wash and 1% clindamycin in gel or lotion (frequency not indicated).- 4 Nd:YAG laser treatments monthly and topical 10% benzoyl peroxide and 1% clindamycin | No. of studies and patients: 12 trials with 615 patients Median, 27 participants; mean duration of treatment, 16 wk. Included studies were done between 1983 and 2015.Effect size: The 3 trials of laser or other light-based treatments were judged to offer a low level of evidence because of lack of precision and adequate blinding.Fadel and Tawfik,382015PDT with topical 0.01% MB gel+IPL was superior to placebo MB gel+IPL; Sartorius score fell by 77.3% and 44.1%, respectivelyHighton et al,112011Significant benefit from IPL in 18 patients: mean Sartorius score reduction of 12% immediately after therapy, 10% at 3 months, 10% at 6 months, and 3% at 12 months. No comparator. Patients assessed satisfaction on an unvalidated Likert scale.Tierney et al,39200917 patients, 4 Nd: YAG laser treatments at monthly intervals on 1 side of the body in 25 regions with lesions. Significantly improved Sartorius scores in treated armpits. A 65.3% reduction in HS severity at 3 mo overall. By locations: 73.4% groin, 62% armpits, 53.1% under breasts. | Studies of Nd:YAG laser, IPL, and topical PDT treatments were of poor quality because of lack of blinding and absence of placebo comparison. | High | |
| John et al,52 2016 | Design: systematic review of RCTs and nonrandomized trials, other systematic reviews, case–control cohort studies, case series, and expert opinionObjective: To evaluate the effects of laser treatment of HS in persons of all agesPeriod searched: 1987–April 2016 | Any individual regardless of sex, age, or ethnicity with a diagnosis of HS treated by any type of laser | Interventions: 47 studies found; 22 analyzed after applying inclusion and exclusion criteriaTwo studies provided grade A evidence (Jadad scale) and 1 provided grade B evidence.Laser therapy was assessed in 3 studies:Higher quality evidence (grade A, Jadad) from Highton et al,11 and Tierney et al,39 both included in the systematic review of Ingram et al3 (above).Xu et al45provided grade B evidence (Jadad).19 patients with Hurley stage 2 HS treated with long-wave Nd:YAG laser (1064nm) twice monthly | No. of studies and patients: 22 studies, 2 with grade A evidence, 1 with grade B, and the rest with grade C (very low)In total, 59 patients were treated in grade A or B studies. The included studies were done between 1987 and 2016.Effect size: grade A evidence assigned to the trials of Highton et al11 and Tierney et al,39 as explained in the entry for the inclusions of the systematic review of Ingram et al.3Xu et al,452011, grade B. The percent change in Sartorius score after 2 mo of treatment was 31.6% (P=.001) on average for all lesion sites; 24.4% (P=.008) for armpits and 36.8% for groin (P=.001). But on histology 3 patients still had inflammation, and the percent changes were not clinically significant. | The conclusion was that there was moderate support for the efficacy long-pulse Nd:YAG laser and IPL in HS and for reducing recurrence by means of hair follicle destruction; and limited evidence for CO2 laser. | Large RCTs, preferably multicenter ones, are needed to standardize assessment techniques and assess efficacy. | High |
| Robert et al,53 2017 | Design: systematic review of RCTs and nonrandomized trials, other systematic reviews, case–control cohort studies, case series, and expert opinionObjective: To summarize and analyze research on current nonsurgical techniques for treating HSPeriod searched: January 2005–September 2015 | Included: all original research articles on nonsurgical HS treatments (RCTs, prospective or retrospective observational studies, and case series of at least 4 patients)Excluded: single case studies, narrative reviews, discussions, opinion articles, research letters, and editorials | Interventions: 64 included articles. Evidence level generally low; most were retrospective observational studies.Biological treatments (44%), PDT or other phototherapies (16%), antibiotic therapy (11%), laser (8%), retinoids (6%), and other immunosuppressant therapies.10 articles on PDT: 4 have already been mentioned elsewhere in our review (Fadel and Tawfik,38 Valladares-Narganes et al,51 Andino Navarrete et al,2 and Highton et al11). After applying our inclusion and exclusion criteria, we evaluated the following:Calzavara-Pinton et al,402013, treated 6 patients (no Hurley stage reported) with MAL-PTD (red light, 635nm) every 2 wk for 4 wkSchweiger et al,412011, treated 12 patients with ALA-PTD (IPL or blue light), weekly for 4 wkSotiriou et al,422009, treated 5 patients (Hurley stage 2 or higher with 20% ALA and red light (570–670nm) 3h later; 4 sessions at 15-d intervals; assessment with VAS, Sartorius score and DLQILaser was used in 5 studies. We excluded 2 reports of <5 patients or with nonvalidated assessment tools and Mikkelsen et al,35a retrospective series that was not relevant (only evaluating long-term recurrence after CO2 laser).Mahmoud et al,432010, treated 22 patients (Hurley stage 2) with 4 sessions of long-pulse Nd:YAG laser monthly for 4 mo; follow-up, 6 mo.Madan et al,442008, treated 9 medically and surgically refractory cases of HS with CO2 (1 session, follow-up at 12 mo). | No. of studies, patients and effect sizes:Calzavara-Pinton et al,402013, assessed response by PGA. Response was >75% in 33% of patients, moderate in half, and <50% in 1.Schweiger et al,412011, saw a Sartorius score reduction of 50.8% at 4 wk and 29.9% at 8 wk. Mean DLQI scores were 17.3 at baseline and 13.1 at 4 wk. Tolerance was better with blue light than IPL.Sotiriou et al,422009, reported that mean Sartorius scores went from 18.8 at baseline to 17.2 on treated sides at the first follow-up visit. Mean VAS evaluations of disease activity/pain went from 2.4 to 2.1. DLQI scores fell by 6.4%.Mahmoud et al,432010, measured the effect of Nd:YAG laser in 22 patients with the Sartorius score, reporting a 72% reduction.Madan et al,442008, reported the PGA of the effect; 7 out of 9 patients had complete remission and expressed high satisfaction. | No nonsurgical treatment leads to long-term remission. The authorsemphasized the need for surgery in refractory and debilitating cases. | Low quality of evidence. Heterogeneous methods of assessment, scarcely comparable. Few RCTs; most studies are of retrospective cohorts | High |
Abbreviations: ALA, 5-aminolevulinic acid; CO2, carbon dioxide; DLQI, Dermatology Life Quality Index; HS, hidradenitis suppurativa; HS-LASI, HS lesion, area and severity index; IPL, intense pulsed light; MAL, methyl aminolevulinate; MB, methylene blue; Nd:YAG, neodymium and neodymium:yttrium aluminum garnet; PDT, photodynamic therapy; QoL, quality of life; RCT, randomized clinical trial; VAS, visual analog scale.
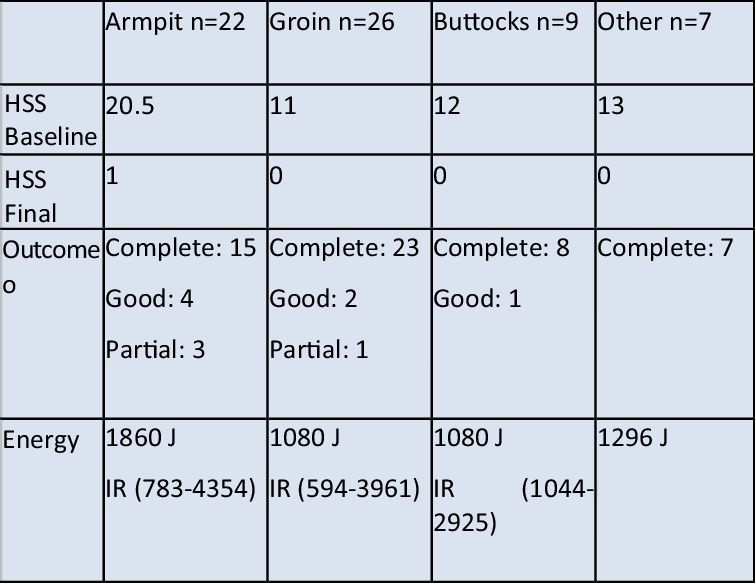
Summary of Articles on Intralesional PDT for HS
| Reference, y | Study Design, Aim and Period | Study Population | Intervention and Follow-up | Results | Conclusions | Comments | Quality of evidence |
|---|---|---|---|---|---|---|---|
| Valladares-Narganes et al,51 2015 | Design: prospective case seriesObjective: To apply PDT with intralesional light probes that can reach different depths with light at the lowest energy level possibleStudy period: March–November 2013 | No. of patients:27 (single group)Characteristics: | Intralesional 1% ALA solution (dose, 0.2mL/cm3).By cannula inserted into fistulous tracts, or needle injection into the diseased area if cannulation was impossible.The entrance to and exit from the fistula was covered for an incubation period of 3h. Next, the fistula was irradiated intralesionally with a continuous diode laser (630nm, fiberoptic probe 1mm in diameter; 1W/cm3; 180J)/cm2). Light was transmitted through a 1-mm needle.If response was suboptimal or new lesions appeared nearby, an additional session was given.Follow-up: 1, 3, and 6 moLosses: 1 | Results on the modified Sartorius scale: 10 (37%) complete, 11 (41%) good, and 5 (19%) partial.Best results in the armpits (complete response in 6 of 8), including patients requiring treatment of both armpits.Moderate pain in 4 patients (VAS, 6–9)Most patients (22 of 27) tolerated the procedure well (VAS scores under 6).Adverse effects included postprocedural pain, erythema and slight swelling. | Intralesional PDT may be an effective and long-lasting treatment for HS.The best results are in isolated lesions in the armpits or sacral and breast regions, where most lesions are found. Multiple, interconnected fistulas require more sessions. | RCTs would be a good step toward adequate assessment of therapies alone or in combination. Trials should include dose detection and patient-relevant outcome measures. | Moderate |
| Agut-Busquet et al,1 2016 | Design: respective case seriesObjective: To describe the experience with 7 patients with HS treated with PDT using intralesional MB and light (635nm)Study period: 8 mo | No. of patients: 7Characteristics: HS clinical type 2, Hurley stage 3, at least 1 active zone | Intralesional 1% MB solution injected with or without ultrasound guidance.After incubation (15min), irradiation with a 635-nm LED light (37J/cm2)1–2 sessions, intervals of 15 d.Follow-up: 1, 2, 4, and 6 moLosses: 1 | Hurley stage-2 patients responded better than stage-3 patients (99% vs 87% improvement); best results in the groin.DQLI improvement in 6 patients: 78% (1), 80% (1), 90% (2), and 99% (2).Evaluation, Sartorius score and PGA: 78% (1 patient), 80% (1), 90% (2), 99% (2).Good response (86% improvement) to antibiotic in only 1 patient.Adverse effects: mild in 6 cases (86%); serious in 1 patient (cellulitis at treatment site, attributed to patient’s manipulation of the area after therapy) | Intralesional PDT with MB gives good results in HS but is more effective in Hurley stage 2 than stage 3.RCTs are necessary to improve the quality of evidence. | Few patients, making extrapolation to the general population (external validation) difficult. | Low |
| Suárez Valladares et al,50 2017 | Design: prospective case seriesObjective: To evaluate the efficacy of intralesional PDT for the local management of HS in the short and medium term in different sitesStudy period: March 2011–November 2015 | No. of patients: 38Characteristics:Sex: 20 women, 18 menAge: 30–44 yWeight: 67.25–90kgMean (SD) BMI: 26.87 (4.89)BMI >27: 20Smokers: 34Prior treatments: 2, none; 1, topical; 23, oral antibiotics; 2, oral retinoids; 1, biologic; 9, surgery.Hurley stages: 1, 4 patients; 2, 21 patients; 3, 13 patients.Direct measures of severity: Hurley, baseline/total HSS, and DLQI indicated high disease activity. | After local anesthesia, 5% ALA gel was injected through a cannula to fill the fistulous tracts. Thus, all walls of fistulous tracts were treated regardless of depth. A lyophilized 1% solution was injected into nodules. Incubation under occlusion for 2h before irradiation. Irradiation (1.2W; fluence, 180J/cm2) with an intralesional 630-nm laser through a 400-mm fiberoptic probe inserted through a needle.Follow-up visits every 5–7 wkFollow-up: 26.1 (21.7–68.57) moLosses: 0 | Single session regardless of site, but the median energy used was greater in the armpits.Complete remission in 76.3%, mean disease-free period of 168 wk. New lesions at untreated sites were observed in 9 patients (23.7%); 6 of them had complete remission.Recurrence or no remission after treatment in 9 patients, in whom the percentages of obesity (33.% vs 58.6%) and smoking (66.7 vs 96.6%) were lower but disease severity was greater (44.4% vs 31%), modified Sartorius score was higher (36 vs 22) and DLQI poorer (16 vs 10) than in those with a good response to PDT. | Intralesional PDT might offer a new alternative treatment for HS lesions, alone or in combination;a high rate of complete remission was achieved and was long-lasting.No complications observed.Rapid recovery after treatment, with the possibility of repeating sessions. | Moderate | |
Abbreviations: BMI, body mass index; DLQI, Dermatology Life Quality Index; E, energy ; HS, hidradenitis suppurativa; HSS, hidradenitis severity score; IR, irradiation; MB, methylene blue; PDT, photodynamic therapy; PGA, Physician’s Global Assessment; RCT, randomized clinical trial; VAS, visual analog scale.
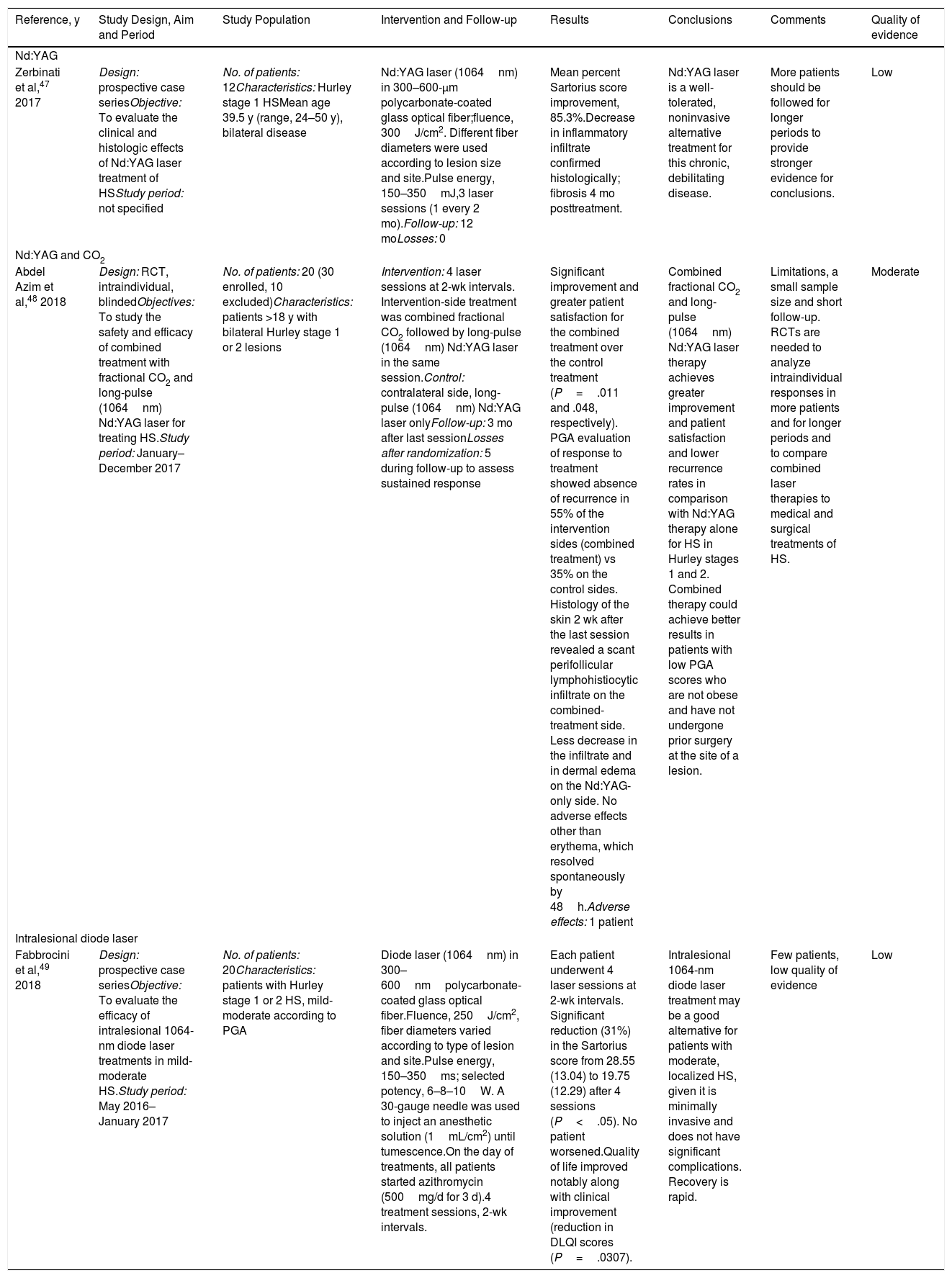
Summary of Articles Included in This Systematic Review According to Light Sources Used To Treat HSa
| Reference, y | Study Design, Aim and Period | Study Population | Intervention and Follow-up | Results | Conclusions | Comments | Quality of evidence |
|---|---|---|---|---|---|---|---|
| Nd:YAG | |||||||
| Zerbinati et al,47 2017 | Design: prospective case seriesObjective: To evaluate the clinical and histologic effects of Nd:YAG laser treatment of HSStudy period: not specified | No. of patients: 12Characteristics: Hurley stage 1 HSMean age 39.5 y (range, 24–50 y), bilateral disease | Nd:YAG laser (1064nm) in 300–600-μm polycarbonate-coated glass optical fiber;fluence, 300J/cm2. Different fiber diameters were used according to lesion size and site.Pulse energy, 150–350mJ,3 laser sessions (1 every 2 mo).Follow-up: 12 moLosses: 0 | Mean percent Sartorius score improvement, 85.3%.Decrease in inflammatory infiltrate confirmed histologically; fibrosis 4 mo posttreatment. | Nd:YAG laser is a well-tolerated, noninvasive alternative treatment for this chronic, debilitating disease. | More patients should be followed for longer periods to provide stronger evidence for conclusions. | Low |
| Nd:YAG and CO2 | |||||||
| Abdel Azim et al,48 2018 | Design: RCT, intraindividual, blindedObjectives: To study the safety and efficacy of combined treatment with fractional CO2 and long-pulse (1064nm) Nd:YAG laser for treating HS.Study period: January–December 2017 | No. of patients: 20 (30 enrolled, 10 excluded)Characteristics: patients >18 y with bilateral Hurley stage 1 or 2 lesions | Intervention: 4 laser sessions at 2-wk intervals. Intervention-side treatment was combined fractional CO2 followed by long-pulse (1064nm) Nd:YAG laser in the same session.Control: contralateral side, long-pulse (1064nm) Nd:YAG laser onlyFollow-up: 3 mo after last sessionLosses after randomization: 5 during follow-up to assess sustained response | Significant improvement and greater patient satisfaction for the combined treatment over the control treatment (P=.011 and .048, respectively). PGA evaluation of response to treatment showed absence of recurrence in 55% of the intervention sides (combined treatment) vs 35% on the control sides. Histology of the skin 2 wk after the last session revealed a scant perifollicular lymphohistiocytic infiltrate on the combined-treatment side. Less decrease in the infiltrate and in dermal edema on the Nd:YAG-only side. No adverse effects other than erythema, which resolved spontaneously by 48h.Adverse effects: 1 patient | Combined fractional CO2 and long-pulse (1064nm) Nd:YAG laser therapy achieves greater improvement and patient satisfaction and lower recurrence rates in comparison with Nd:YAG therapy alone for HS in Hurley stages 1 and 2. Combined therapy could achieve better results in patients with low PGA scores who are not obese and have not undergone prior surgery at the site of a lesion. | Limitations, a small sample size and short follow-up. RCTs are needed to analyze intraindividual responses in more patients and for longer periods and to compare combined laser therapies to medical and surgical treatments of HS. | Moderate |
| Intralesional diode laser | |||||||
| Fabbrocini et al,49 2018 | Design: prospective case seriesObjective: To evaluate the efficacy of intralesional 1064-nm diode laser treatments in mild-moderate HS.Study period: May 2016–January 2017 | No. of patients: 20Characteristics: patients with Hurley stage 1 or 2 HS, mild-moderate according to PGA | Diode laser (1064nm) in 300–600nmpolycarbonate-coated glass optical fiber.Fluence, 250J/cm2, fiber diameters varied according to type of lesion and site.Pulse energy, 150–350ms; selected potency, 6–8–10W. A 30-gauge needle was used to inject an anesthetic solution (1mL/cm2) until tumescence.On the day of treatments, all patients started azithromycin (500mg/d for 3 d).4 treatment sessions, 2-wk intervals. | Each patient underwent 4 laser sessions at 2-wk intervals. Significant reduction (31%) in the Sartorius score from 28.55 (13.04) to 19.75 (12.29) after 4 sessions (P<.05). No patient worsened.Quality of life improved notably along with clinical improvement (reduction in DLQI scores (P=.0307). | Intralesional 1064-nm diode laser treatment may be a good alternative for patients with moderate, localized HS, given it is minimally invasive and does not have significant complications. Recovery is rapid. | Few patients, low quality of evidence | Low |
Abbreviations: CO2, carbon dioxide; DLQI, Dermatology Life Quality Index; HS, hidradenitis suppurativa; Nd:YAG, neodymium-doped yttrium aluminum garnet; PGA, Physician’s Global Assessment; RCT, randomized clinical trial.
The number of participants in the included studies ranged widely. The maximum was 3846 and the minimum was 5,2,42 for a total of 248 patients (mean, 15.5 patients).
ParticipantsAll the studies included men and women older than 18 years with a clinical diagnosis of HS.
One study included only Hurley stage 1 patients (Zerbinati et al47) and 1 included only Hurley stage 2 patients (Mahmoud et al43). Two studies included both Hurley 1 and 2 stages (Abdel Azim et al48 and Fabbrocini et al49). Six studies required moderately severe HS (Hurley stages 2 or 3) at baseline (Andino Navarrete et al,2 Agut-Busquet et al,1 Highton et al,11 Tierney et al,39 Xu et al,45 and Sotiriou et al42). One study included any stage of severity (stages 1, 2, or 3) (Suárez Valladares et al50). Finally, 5 studies did not specify stage (Valladares-Narganes et al,51 Fadel and Tawfik,38 Calzavara-Pinton et al,40 Madan et al,44 and Schweiger et al41).
Study DesignsWe included 3 systematic reviews for this systematic update (Ingram et al,3 John et al,52 and Robert et al53) and 2 clinical trials (Fadel and Tawfik38 and Abdel Azim et al48). The remaining studies were case series.
The systematic review of Ingram et al3 included 3 RCTs comparing topical PDT, IPL and Nd:YAG laser therapy.11,38,39 Fadel and Tawfik38 used an active comparator in the control group. Controls were untreated in Highton et al,11 whereas Tierney et al39 applied 1% clindamycin cream in the control group. The systematic review of John et al52 included 22 studies. Three provided high-quality evidence (and were also included by Ingram et al). The only additional inclusion that met our criteria was that of Xu et al,45 which assessed Nd:YAG laser treatment. The most up-to-date systematic review was by Robert et al,53 who included 64 articles about the nonsurgical treatment of HS (with medications or light therapies). Studies of light-based treatments that were not included in the aforementioned reviews were those of Calzavara-Pinton et al40 (PDT with methyl aminolevulinate [MAL]) and Schweiger et al41 and Sotiriou et al42 (PDT with ALA). This third systematic review also included two case series of patients treated with Nd:YAG laser (Mahmoud et al43) and CO2 laser (Madan et al44).
Only 2 RCTs were retrieved. One was by Fadel and Tawfik,38 which was found by backwards searching of citations as described above. The other was by Abdel Azim et al,48 which evaluated a combined treatment with CO2 laser followed by Nd:YAG laser.
One of the case series we included studied the use of PDT with 20% ALA as the photosensitizer and 635-nm laser (Andino Navarrete et al2). Three studies analyzed intralesional PDT. Two used ALA at concentrations of 5% and 1% and a 630-nm laser light source.50,51 The third used MB and a 635-nm light-emitting diode (LED) lamp (Aktilite).1
Zerbinati et al47 analyzed case series in which Nd:YAG laser was used, and Fabbrocini et al49 evaluated the efficacy of diode laser irradiation in mild to moderate HS.
Outcome MeasuresThe included studies assessed outcomes in somewhat different ways. Most used the Sartorius score of 2003,1,2,11,38,39,41–43,45,47,49 but 2 studies used the modified version of this score.50,51 Five (Agut-Busquet et al,1 Abdel Azim et al,48 Calzavara-Pinton et al,40 Fabbrocini et al,49 and Madan et al44) used the PGA.
Six evaluated changes in quality of life with the Dermatology Life Quality Index (DLQI) published by Finlay in 1994).1,2,41,42,49,50 General satisfaction was evaluated by Highton et al11 with an unvalidated Likert scale and by Madan et al44 with a score of 0 (very unsatisfied) to 10 (very satisfied).
Two studies assessed pain during and after treatment using a visual analog scale (VAS).2,51
Four studies provided information about adverse effects,1,2,51 although Highton et al11 only reported such effects if treatment had to be interrupted.
Finally, 5 studies reported recurrence rates. Agut-Busquet et al1 emphasized recurrence, explaining each case. Suárez Valladares et al50 reported recurrence in 9 patients. Highton et al11 found that HS tended to recur 12 months after treatment. Recurrence 3 and 12 months after treatment was assessed by Abdel Azim et al48 and Madan et al,44 respectively.
Outcomes Obtained With Light-Based TherapiesTables 1–3 summarize the research designs used and quality of evidence obtained by researchers studying the use of conventional PDT, intralesional PDT, and laser treatments. As explained above, the 3 systematic reviews we consulted included patients treated with both PDT and laser therapy. Therefore, to avoid repetition, one table (Table 1) presents the studies that applied laser treatments and IPL in bold face type.
PDTAndino Navarrete et al2 treated 5 patients with a 20% ALA solution for 1.5h and then irradiated the area with a 635-nm LED lamp at a fluence of 37J/cm2 and intensity of 70mW/cm2 per session. The patients experienced improvements (Sartorius score, DLQI, and VAS) that was maintained at 8 weeks, although the differences were not statistically significant.
Fadel and Tawfik38 used PDT with a 0.01% MB gel (formulation in liposomes with surfactants to increase penetration) and compared it to placebo (MB-free) gel. The area was irradiated with IPL (630nm) for 20ms at a fluence of 25J/cm2. The participants were authorized to receive treatment at every affected area of the body (armpits, buttocks, groin, and under the breasts). Results showed a Sartorius score reduction of 77.3% (liposome MB gel formulation) and 44.1% (MB-free placebo) (P<.01). The authors concluded that PDT with MB in this formulation is superior to irradiation after MB-free gel.38
Calzavara-Pinton et al40 studied patients with various diseases treated with MAL-PDT; 6 patients with HS were among them. The authors irradiated with red light (635nm) every 2 weeks for 4 weeks and reported a PGA assessment of more than 75% in 33% of the cases, moderate improvement in half, and a poor response in 1 patient.
Schweiger et al41 described 12 patients treated with ALA-PDT with blue light and IPL weekly for 4 weeks. Four weeks after treatment they observed a reduction in the Sartorius score of 50.8%. At 8 weeks the reduction was 29.9%. The DLQI score fell from 17.3 to 13.1. Blue light was tolerated better than IPL.
Finally, Sotiriou et al42 applied a 20% ALA formulation in 5 sessions in 5 patients with Hurley stage 2 or higher HS. The mean Sartorius score decreased from 18.8% to 17.2%, and DLQI impact fell 6.4% on average. These results are summarized in Table 1.
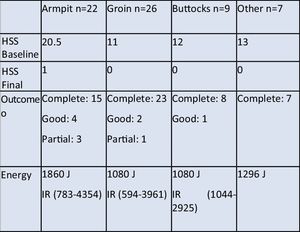
Intralesional PDTValladares-Narganes et al51 administered 1% ALA (0.2mL/cm3) into lesions followed by light exposure, as noted above, in a series of 27 patients with 1 to 3 lesions each. After 26.21 months (range, 21.07–68.57 months), responses were complete in 10 patients (37%), moderate in 11 (41%), and partial in 5 (19%). The authors saw the best results in armpit lesions (Table 2).
Agut-Busquet et al1 injected a 1% MB solution into lesions under ultrasound guidance in 7 patients. After incubation (15minutes), the lesions were irradiated with an LED lamp (Aktilite, 635nm, 37J/cm2). After 6 months the global assessment of response was 78% in 1 patient, 80% in 1, 90% in 2, and 99% in 2. Patients with Hurley stage 2 HS responded better (99%) than those with Hurley stage 3 (87%), and the best results were observed in groin lesions. DLQI improved significantly for 6 patients, coinciding with excellent response to treatment. Mild adverse effects (swelling or erythema) were observed in 6 patients (86%), but they resolved within a week (Table 2).
Suárez Valladares et al50 injected a 5% ALA gel into lesions through a cannula placed along the sinus tract in 38 patients. After incubation under opaque occlusion for 2hours, intralesional laser irradiation (630nm, 1.2W; fluence, 180J/cm2) was applied with a fiberoptic probe (400mm). All regions treated improved according to modified Sartorius scale results. There were 53 complete responses, 7 good responses, and 4 partial responses. However, the differences were not statistically significant (Table 2).
Nd:YAG Laser TreatmentTierney et al39 compared Nd:YAG treatments with 10% benzoyl peroxide and daily application of 1% clindamycin versus application of the topical antibiotic alone. Seventeen patients were enrolled and 4 laser sessions were given at intervals of 1 month (Table 1). The reduction in severity according to modified Sartorius assessment was 65.3% at 3 months on average over all regions (73.4% in the groin, 62% in the armpits, and 53.1% under the breasts). Improvement was significant in laser-treated patients, but not in the control group (topical clindamycin only) (P<.02).
Xu et al45 published a prospective, controlled histopathologic study in 19 patients with Hurley stage 2 HS. The patients were treated in 2 monthly sessions of Nd:YAG laser therapy (1064nm). The percent response to treatment on the Sartorius score after 2 months was 31.6% (P=.001). Greater improvement was recorded in groin lesions (Table 1).
Zerbinati et al47 observed a mean improvement of 85.3% in the Sartorius score with Nd:YAG treatment of very early Hurley stage 1 HS in 12 patients (Table 3). In a similar study, but with 22 patients with more severe HS (Hurley stage 2), Mahmoud et al43 evaluated the response at 6 months to 4 sessions of a series of 1 long-pulse Nd:YAG treatment per month for 4 months. They also observed a decrease in the Sartorius score (−72%) (Table 1).
Other Types of Laser TreatmentAn RCT of CO2 laser treatment was carried out by Abdel Azim et al48 in 20 patients over the age of 18 years who had Hurley stage 1 or 2 HS. The aim was to assess the safety and efficacy of combining fractional CO2 irradiation with long-pulse Nd:YAG laser irradiation (1064nm) in 4 sessions separated by 2 weeks. On the intervention side the patients received fractional CO2 laser treatment followed by long-pulse Nd:YAG laser (1064nm) in the same session. On the control side, only the Nd:YAG treatment was used. The authors concluded that improvement and satisfaction were greater with the combined treatment of early (Hurley stage 1 and 2) disease and that the recurrence rate was lower (Table 3).
Of 9 patients with medically and surgically refractory HS who received CO2 laser treatments from Madan et al,44 7 had achieved complete remission at 12 months. Satisfaction was high (Table 1).
Finally, Fabbrocini et al49 used laser diode light in a group with Hurley stage 1 or 2 HS and mild to moderate disease according to PGA. The patients received 4 sessions spaced every 2 weeks. A significant reduction of 31% was seen in the Sartorius scores, which changed from 28.55 (SD, 13.04) to 19.75 (SD, 12.29) (P<.05). The authors also reported a direct association between improvement and better quality of life (Table 3).
IPLHighton et al11 enrolled 18 patients in an RCT comparing active and control treatments on contralateral sides. The active treatment was IPL (50ms, 420nm, fluence of 7–10J/cm2). They observed a mean reduction in the Sartorius score of 12% immediately after therapy, 10% at 3 to 6 months, and 3% at 12 months. The difference between the treated and control sides was significant (P<.01). Patient satisfaction was high. Response was complete in 1 case, excellent in 2 cases, good in 10, and moderately good in 4. Fifteen did not experience significant changes on the control side: 1 patient reported slight improvement and another experienced slight worsening. The treatment was applied once a week for 4 weeks. Follow-up was 12 months (Table 1).
DiscussionConsidering the limited evidence available for light-based treatments for HS, it is difficult to draw conclusions about the efficacy of either intralesional versus topical approaches, or IPL or Nd:YAG laser. Variation in study designs makes comparison difficult.
We identified 3 photosensitizers being used in PDT: ALA, MAL, and MB. All of them were applied at different concentrations from 1% to 20% for ALA, 16% for MAL, and 0.01% to 1% for MB. Which concentration leads to a better response rate is difficult to establish because evaluation methods differ. Moreover, the type of light used to irradiate lesions also varies, as some groups use LED lamps,1,40,42 while others apply external2 or intralesional laser50,51 and still others use IPL.38,41 The possibility of treating deep HS lesions is an important factor in efficacy, yet these light sources have frank differences in penetration. The light doses also differ, although the wavelength applied is similar at 630 or 635nm.
The studies also treated lesions at different sites, for different durations and numbers of sessions (from 150 to 1238). The main difference in technique, however was between the use of topical versus intralesional application of both the photosensitizer (ALA, MAL, or MB) and the light source (LED, laser, or IPL).
We found that intralesional treatment approaches also differed between authors. Suárez Valladares et al50 and Valladares-Narganes et al51 used 630-nm diode lasers and ALA at different concentrations. They assessed response with the modified Sartorius score, finding that response was better with a 5% ALA gel and a 400-nm diode laser (1.2W and 180J/cm2). Agut-Busquet et al,1 on the other hand, used a 1% MB formulation and a 635-nm LED with a fluence of 37J/cm2. They assessed efficacy with the DQLI and the Sartorius score, reporting responses that varied from 99% for cases involving Hurley stage 1 to 87% in Hurley stage 3.
The single study of IPL we found reported that statistically significant improvement was maintained for 12 months and that the risk of complications was low.11
The RCT of Nd:YAG laser treatment by Tierney et al39 demonstrated efficacy. Later case series describing this treatment have reported reduction in the number of exacerbations and in severity.43,47 Efficacy has been reported to be greater in the groin.45
Very few studies have been published on other types of lasers, but all of them report promising results. The combination of CO2 and Nd:YAG lasers obtained better results than Nd:YAG irradiation alone and patient satisfaction was higher.48 Madan et al44 showed that CO2 laser therapy and marsupialization also led to high rates of complete remission in spite of adverse effects, such as hypertrophic scarring.
We found a single study of diode laser therapy for HS that was considered mild to moderate according to the PGA.48 The authors reported clinical and quality-of-life improvement after therapy.
In summary, the evidence supporting the use of light-based therapies for HS is limited. There are 2 major groupings of these therapies according to whether a photosensitizer is used or not. In 1 group, for which only a low-moderate level of evidence is available, the authors applied Nd:YAG laser, CO2 laser, or IPL. In the other, for which the quality of evidence is also low-moderate, PDT (with photosensitizer) was used. Thus, all the treatments reviewed used light but they are not comparable: different techniques have different mechanisms of action. However, results for individual treatments do seem to suggest that approaches that offer greater penetration — whether by means of intralesional application or lasers — lead to better results.
RCTs are necessary to confirm the efficacy of these treatments. We also need to see standardized research protocols applying the design that is most appropriate for providing stronger evidence for the efficacy and safety of each technique.
AuthorshipT. Gracia Cazaña and L.V. Berdel García contributed equally to this article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
We thank Ms Visitación Ortega Riba and Ms Montserrat Salas Valera for their help with the systematic literature review and downloading of articles.
We are also grateful to the Government of the Spanish Autonomous Community of Aragon for their recognition of our research group (reference number B18_17D).
Please cite this article as: Gracia Cazaña T, et al. Revisión sistemática de las terapias con luz en el tratamiento de la hidrosadenitis supurativa. Actas Dermosifiliogr. 2020;111:89–106.